
10.1111@pace.13216
.pdf
Heart failure and supraventricular arrhythmias frequently co-exist. 4, 5
Supraventricular tachycardia and atrial fibrillation are the most common sources of inappropriate ICD therapies. Smaller, single-center studies previously identified such factors as non-ischemic cardiomyopathy and history of atrial tachyarrhythmias as predictors of inappropriate therapy.7, 8 Larger studies subsequently confirmed prior atrial fibrillation as an important predictor, and found additional variables such as younger age, smoking, and diastolic hypertension to be associated with inappropriate therapies.9, 10 However, data are scarce describing the relationship between HF severity and inappropriate therapies. While a limited number of studies have provided evidence that greater HF severity may lead to greater risk of inappropriate shock, these investigations were performed over a decade ago, when CRT-D was less prevalent.14, 15 Further, cardiac resynchronization therapy lowers risk of atrial fibrillation as a result of left atrial reverse remodeling, but whether HF severity still affects risk of inappropriate therapies in CRT-D patients is less clear. 21
Thus, the present study, which consists of a larger number of patients from multiple centers, investigated the impact of HF severity in ICD and CRT-D patients separately. As previously described, in MADIT-RIT, CRT-D patients had overall lower risk of inappropriate therapy than ICD patients.22 It is not known, however, whether this relationship is further modified by HF severity. We now report that, in both CRT-D and ICD recipients, NYHA III relative to NYHA I-II was associated with a greater risk of inappropriate ICD therapy. Driving this increased risk was inappropriate ATP for arrhythmias < 200 bpm, which were mainly supraventricular tachycardia and atrial fibrillation/flutter events as reported previously. 23 In general, inappropriate shock and inappropriate therapy for rhythms ≥ 200 bpm were far less prevalent in MADIT-RIT.17
Randomized and cohort-controlled studies in addition to MADIT-RIT have
This article is protected by copyright. All rights reserved. 11

demonstrated that novel programming utilizing increased heart rate thresholds and prolonged detection for treatment of ventricular arrhythmias can effectively reduce risk of inappropriate therapy.16-18 Improving efficacy of ICD therapy is particularly relevant given potential harms associated with inappropriate therapies, ranging from psychological trauma to heart failure progression and even mortality.11-13 In our secondary analysis in the present study, we show that both moderate and mild HF patients derive marked benefit from novel programming in terms of risk reduction in inappropriate therapy, despite the greater baseline risk of inappropriate ICD therapy among moderate HF patients.
Our findings have important clinical implications for the management of patients with more severe HF with both CRT-D and ICD-only devices. First, we document increased risk of inappropriate ICD therapy in patients with more severe HF, driven by ATP due to arrhythmias < 200 bpm, even among those receiving CRT-D. Despite this increased risk, there is benefit from novel ICD programming with reductions in inappropriate ICD therapy, regardless of HF severity. We, therefore, suggest the implementation of high-rate cut-off and prolonged detection strategies in both mild and moderate HF patients. However, to date, a minority of ICD and CRT-D patients has been reprogrammed to higher rate cut-off or prolonged detection following publication of the MADIT-RIT study. Varma et al reported that, among those receiving ICD after publishing the primary findings of MADIT-RIT, ICD programming strictly based on parameters from Arms B and C was found only in 8.9% of patients.24 When less strict adoption of MADIT-RIT ICD programming principles were evaluated, they found that VT therapy ≥ 200 bpm programming occurred in 21.7% of recipients, while longer detection delay > 60 seconds was programmed only in about 3.5%. These observations are further relevant, since long-detection intervals from the ADVANCEIII trial have been associated with reduction in subsequent cardiovascular hospitalizations,
This article is protected by copyright. All rights reserved. 12

lengths-of-stay, and cost, relative to standard-interval programming. 25 Therefore, focusing reprogramming in high-risk cohorts such as moderate HF patients, either with an implanted ICD or CRT-D, may be warranted.
Limitations
We acknowledge that the NYHA classification of HF symptoms involves a degree of subjectivity, but remains a commonly used method of assessing HF severity, including for the purposes of determining CRT-D eligibility. As stated above, given the low percentage of patients with inappropriate ICD shock in this analysis, we were limited in our ability to study this end point adequately. We do not have data available on changes in drug therapy during follow-up.
This study is a retrospective analysis of MADIT-RIT and has the inherent biases of post-hoc analyses. Although we adjusted our multivariable models for potential confounders and conducted sensitivity analyses, there may have been unmeasured confounders that were not taken into consideration. The average follow-up time of 1.4 years in this study may be considered relatively short, however similar studies assessing novel ICD programming had even shorter follow-up times.
CONCLUSIONS
Moderate heart failure patients with NYHA class III are at an increased risk of inappropriate ICD therapy, dominated by inappropriate ATP for supraventricular arrhythmias less than 200 bpm, when compared to mild heart failure patients with NYHA class I-II. Furthermore, novel ICD programming with high-rate cut-off and prolonged detection significantly reduced the
This article is protected by copyright. All rights reserved. 13

risk of inappropriate ICD therapies in both moderate and mild heart failure patients. Implementation of novel ICD programming with high-rate cut-off and delayed therapy is warranted for both and moderate heart failure patients to reduce the risk of inappropriate ICD therapy and improve outcomes.
Sources of Funding
The MADIT-RIT study was supported by a research grant from Boston Scientific to the University of Rochester.
Disclosures
Dr. Kutyifa has received research grants from Boston Scientific and Zoll. Drs. Schuger, Zareba, and Moss have received research grants from Boston Scientific. Dr. James Daubert reports the following relationships with industry: (1) Research grants to Duke University from Biosense Webster, Medtronic, Gilead, St. Jude, and NIH. (2) Remuneration for lectures, consultation, Advisory Board, Data Safety Monitoring Board, Events Committee, and/or consultation from: ARCA Biopharma, Biosense Webster, Biotronik, Boston Scientific, Cardiofocus, Gilead, Medtronic, Northwestern University, St. Jude, Vytronus, and Zoll. All other authors declare no conflict of interest.
REFERENCES
This article is protected by copyright. All rights reserved. 14

1.Bardy GH, Lee KL, Mark DB, Poole JE, Packer DL, Boineau R, Domanski M, Troutman C, Anderson J and Johnson G. Amiodarone or an implantable cardioverter– defibrillator for congestive heart failure. New England Journal of Medicine. 2005;352:225-
2.Moss AJ, Hall WJ, Cannom DS, Daubert JP, Higgins SL, Klein H, Levine JH, Saksena S, Waldo AL and Wilber D. Improved survival with an implanted defibrillator in patients with coronary disease at high risk for ventricular arrhythmia. New England Journal of Medicine. 1996;335:1933-1940.
3.Moss AJ, Zareba W, Hall WJ, Klein H, Wilber DJ, Cannom DS, Daubert JP, Higgins SL, Brown MW and Andrews ML. Prophylactic implantation of a defibrillator in patients with myocardial infarction and reduced ejection fraction. New England Journal of Medicine.
2002;346:877-883.
4.Kotecha D and Piccini JP. Atrial fibrillation in heart failure: what should we do?
European heart journal. 2015:ehv513.
5.Lubitz SA, Benjamin EJ and Ellinor PT. Atrial fibrillation in congestive heart failure.
Heart failure clinics. 2010;6:187-200.
6.Koneru JN, Swerdlow CD, Wood MA and Ellenbogen KA. Minimizing inappropriate or
“unnecessary” implantable cardioverter-defibrillator shocks. Circulation: Arrhythmia and Electrophysiology. 2011;4:778-790.
7.Theuns DA, Klootwijk APJ, Simoons ML and Jordaens LJ. Clinical variables predicting inappropriate use of implantable cardioverter-defibrillator in patients with coronary heart disease or nonischemic dilated cardiomyopathy. The American journal of cardiology. 2005;95:271-274.
8.Alter P, Waldhans S, Plachta E, Moosdorf R and Grimm W. Complications of implantable cardioverter defibrillator therapy in 440 consecutive patients. Pacing and Clinical Electrophysiology. 2005;28:926-932.
9.van Rees JB, Borleffs CJW, de Bie MK, Stijnen T, van Erven L, Bax JJ and Schalij MJ. Inappropriate implantable cardioverter-defibrillator shocks: incidence, predictors, and impact on mortality. Journal of the American College of Cardiology. 2011;57:556-562.
10.Daubert JP, Zareba W, Cannom DS, McNitt S, Rosero SZ, Wang P, Schuger C, Steinberg JS, Higgins SL and Wilber DJ. Inappropriate implantable cardioverter-defibrillator shocks in MADIT II: frequency, mechanisms, predictors, and survival impact. Journal of the American College of Cardiology. 2008;51:1357-1365.
11.Poole JE, Johnson GW, Hellkamp AS, Anderson J, Callans DJ, Raitt MH, Reddy RK, Marchlinski FE, Yee R and Guarnieri T. Prognostic importance of defibrillator shocks in patients with heart failure. New England Journal of Medicine. 2008;359:1009-1017.
This article is protected by copyright. All rights reserved.
15

12.Cevik C, Perez-Verdia A and Nugent K. Implantable cardioverter defibrillators and their role in heart failure progression. Europace. 2009;11:710-715.
13.Deyell MW, Qi A, Chakrabarti S, Yeung-Lai-Wah JA-F, Tung S, Khoo C, Bennett MT, Qian H and Kerr CR. Prognostic impact of inappropriate defibrillator shocks in a population cohort. Heart. 2013:heartjnl-2012-303407.
14.Hreybe H, Ezzeddine R, Barrington W, Bazaz R, Jain S, Ngwu O and Saba S. Relation of advanced heart failure symptoms to risk of inappropriate defibrillator shocks. The American journal of cardiology. 2006;97:544-546.
15.Nanthakumar K, Dorian P, Paquette M, Greene M, Edwards J, Heng D, Noble J and Newman D. Is inappropriate implantable defibrillator shock therapy predictable? Journal of interventional cardiac electrophysiology. 2003;8:215-220.
16.Gasparini M, Proclemer A, Klersy C, Kloppe A, Lunati M, Ferrer JBM, Hersi A, Gulaj M, Wijfels MC and Santi E. Effect of long-detection interval vs standard-detection interval for implantable cardioverter-defibrillators on antitachycardia pacing and shock delivery: the ADVANCE III randomized clinical trial. Jama. 2013;309:1903-1911.
17.Moss AJ, Schuger C, Beck CA, Brown MW, Cannom DS, Daubert JP, Estes III NM, Greenberg H, Hall WJ and Huang DT. Reduction in inappropriate therapy and mortality through ICD programming. New England Journal of Medicine. 2012;367:2275-2283.
18.Wilkoff BL, Williamson BD, Stern RS, Moore SL, Lu F, Lee SW, Birgersdotter-Green UM, Wathen MS, Van Gelder IC and Heubner BM. Strategic programming of detection and therapy parameters in implantable cardioverter-defibrillators reduces shocks in primary prevention patients: results from the PREPARE (Primary Prevention Parameters Evaluation) study. Journal of the American College of Cardiology. 2008;52:541-550.
19.Schuger C, Daubert JP, Brown MW, Cannom D, Estes N, Hall WJ, Kayser T, Klein H, Olshansky B and Power KA. Multicenter Automatic Defibrillator Implantation Trial: Reduce Inappropriate Therapy (MADIT RIT): Background, Rationale, and Clinical Protocol. Annals of Noninvasive Electrocardiology. 2012;17:176-185.
20.Epstein AE, DiMarco JP, Ellenbogen KA, Estes NM, Freedman RA, Gettes LS, Gillinov AM, Gregoratos G, Hammill SC and Hayes DL. ACC/AHA/HRS 2008 guidelines for device-based therapy of cardiac rhythm abnormalities: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the ACC/AHA/NASPE 2002 Guideline Update for Implantation of Cardiac Pacemakers and Antiarrhythmia Devices) developed in collaboration with the American Association for Thoracic Surgery and Society of Thoracic Surgeons. Journal of the American College of Cardiology. 2008;51:e1-e62.
This article is protected by copyright. All rights reserved.
16

21.Brenyo A, Link MS, Barsheshet A, Moss AJ, Zareba W, Wang PJ, McNitt S, Huang D, Foster E and Estes M. Cardiac resynchronization therapy reduces left atrial volume and the risk of atrial tachyarrhythmias in MADIT-CRT (Multicenter Automatic Defibrillator Implantation Trial with Cardiac Resynchronization Therapy). Journal of the American College of Cardiology. 2011;58:1682-1689.
22.Kutyifa V, Daubert JP, Schuger C, Goldenberg I, Klein H, Aktas MK, McNitt S, Stockburger M, Merkely B and Zareba W. Novel ICD Programming and Inappropriate ICD Therapy in CRT-D Versus ICD Patients. Circulation: Arrhythmia and Electrophysiology. 2016;9:e001965.
23.Kutyifa V, Daubert JP, Olshansky B, Huang DT, Zhang C, Ruwald A-CH, McNitt S, Zareba W, Moss AJ and Schuger C. Characterization and predictors of first and subsequent inappropriate ICD therapy by heart rate ranges: Result of the MADIT-RIT efficacy analysis. Heart Rhythm. 2015;12:2030-2037.
24.Varma N, Jones P, Wold N and Stein K. How well do results from large randomized clinical trials diffuse into clinical practice? Impact of MADIT-RIT in a large cohort of implantable cardioverter defibrillator patients (ALTITUDE). European Heart Journal. 2014;35:49-49.
25.Proclemer A, Arenal A, Lunati M, Ferrer J, Hersi A, Manotta L and Gasparini M. Association of long vs standard detection intervals for implantable cardioverter-defibrillators with hospitalizations and costs. JAMA. 2014;312:555.
FIGURE LEGENDS
This article is protected by copyright. All rights reserved.
17
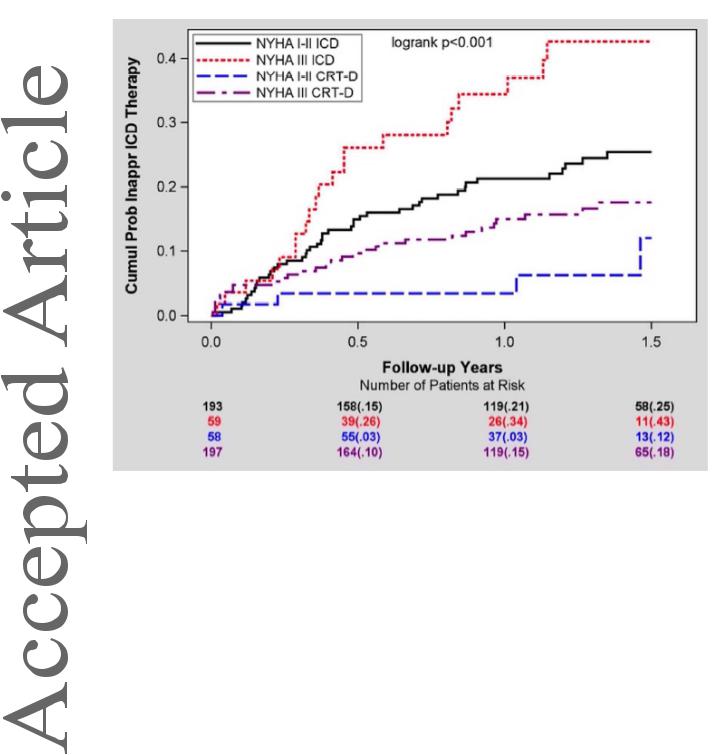
Figure 1: Cumulative probability of all inappropriate therapy by NYHA class and device type
in patients from Arm A
This article is protected by copyright. All rights reserved.
18
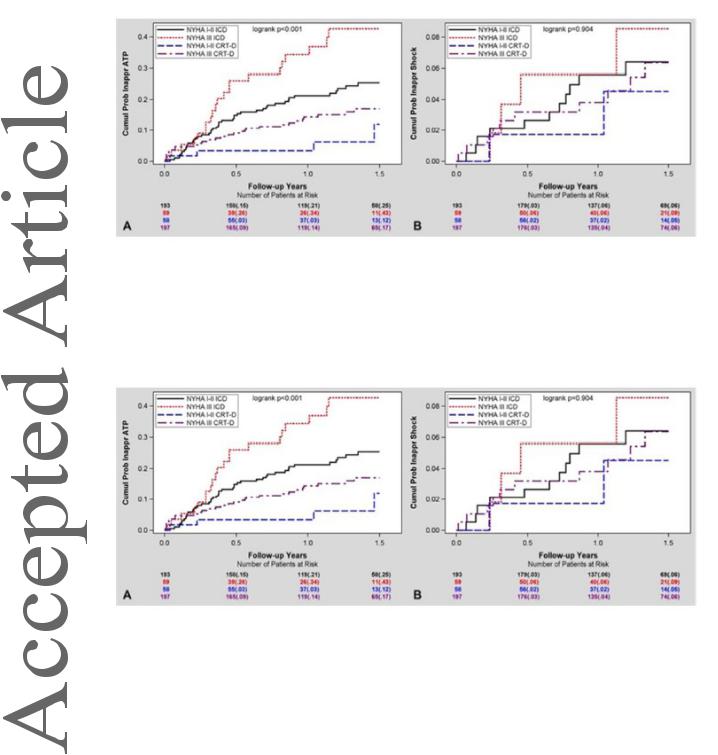
Figure 2: Cumulative probability of (A) inappropriate ATP and (B) inappropriate shock by NYHA class and device type in patients from Arm A
Figure 3: Cumulative probability of (A) inappropriate therapy for HR < 200 bpm and (B) inappropriate therapy for HR ≥ 200 by NYHA class and device type in patients from Arm A
This article is protected by copyright. All rights reserved. 19

Figure 4: Cumulative probability of all inappropriate therapy with novel vs. conventional ICD programming in (A) NYHA Class III and (B) NYHA Class I-II patients
This article is protected by copyright. All rights reserved. 20
