
clavien_atlas_of_upper_gastrointestinal_and_hepato-pancreato-biliary_surgery2007-10-01_3540200045_springer
.pdf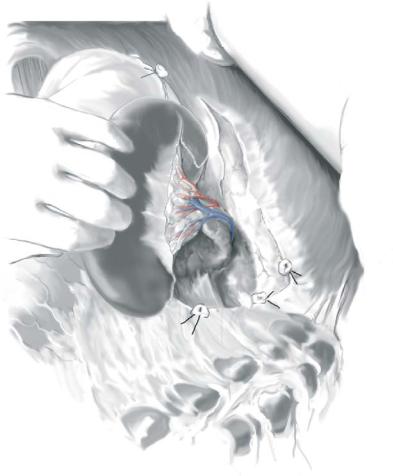
Partial Splenectomy, Open and Laparoscopic |
969 |
|
|
|
|
STEP 2 |
Exposing the entire hilum and ligating appropriate arteries |
|
|
|
|
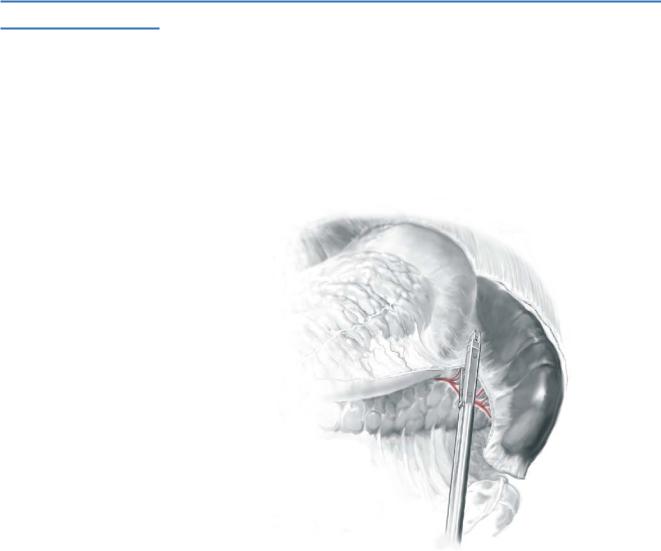
The next step involves exposure of the entire hilum of the spleen close to the parenchyma. The gastrosplenic and splenorenal ligaments need to be separated while preserving the blood supply to both poles. There is a fairly avascular area of this ligament that needs to be opened between the short gastric vessels to the superior pole and the gastroepiploic branches to the lower pole. This will lead to a complete display of the entire splenic blood supply including both poles.
Selected arterial branches then need to be tediously dissected as close to the spleen parenchyma as possible, noting that the veins are situated posteriorly in close proximity. The vessels can be doubly ligated, transfixed or clipped. The long slender laparo-
scopic clip appliers can be used for this step of the procedure. Once the arterial blood supply is controlled, the affected spleen will visibly demarcate rapidly. If the devitalized spleen corresponds to the intended resection, a similar technique is used on the venous side. Access to the venous side can also be achieved from the posterior aspect of the spleen (as indicated in illustration).
970 |
SECTION 7 |
Spleen |
|
|
|
STEP 3 |
Incising the splenic capsule and resection |
|
|
|
|
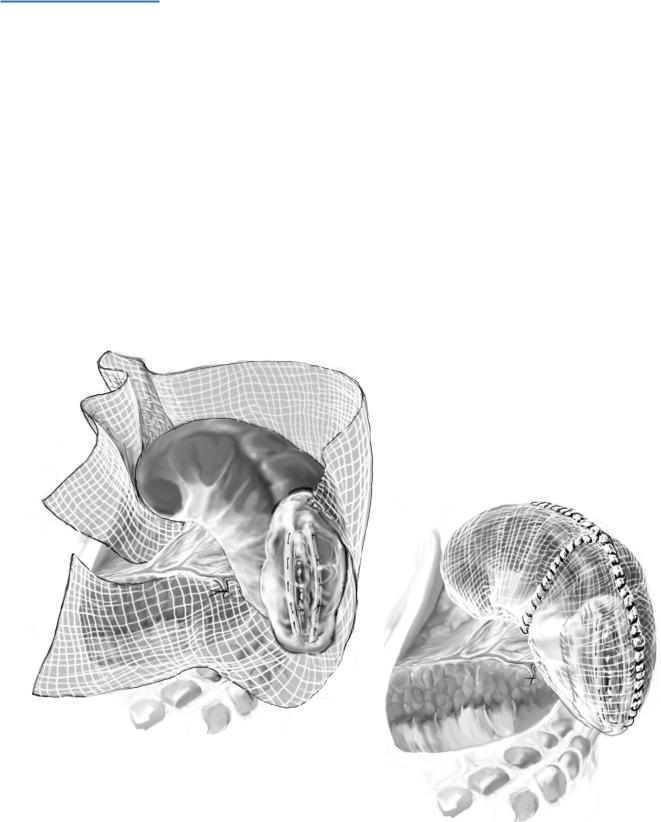
The capsule of the spleen is incised circumferentially with a scalpel or monopolar cautery, making sure to leave 5mm of devitalized tissue in situ. The splenic fragments can be transected with a combination of scalpel, scissors or monopolar cautery. When enough residual devitalized tissue is left behind circumferentially, very little hemostasis is required and it can usually be achieved by simple means and topical agents.
The abdomen is closed, with or without a closed suction drain, after complete hemostasis is achieved.
972 |
SECTION 7 |
Spleen |
|
|
|
|
Tricks of the Senior Surgeon |
|
■Detailed knowledge of splenic anatomy constitutes the single most important factor that will allow the surgeon to consider all the options available to save splenic parenchyma. There are two patterns of terminal artery branching: distributed and bundled or magistral (see STEP 1). Most specimens have two or three terminal branches (superior polar, superior and inferior terminal) determining lobes or segments. Relative avascular planes are identified between lobes and segments. The surgical unit of the spleen is based upon surgically accessible vessels at the hilum.
■The keys to success with partial laparoscopic splenectomy are experience with advanced laparoscopy, case selection, ability to dissect branches of the splenic artery close to the hilum, and foremost the realization that leaving a 5-mm margin of devitalized spleen in situ greatly simplifies homeostasis.
■Specially in the laparoscopic approach, improper use of the cautery can cause iatrogenic injury to the stomach, colon, and pancreas. Structures close to the lower pole in the gastrocolic ligament can be approached aggressively with the cautery, but blind fulguration of fat in the hilum can result in serious bleeding. The instrument should be activated only in proximity to the target organ to avoid arcing and spot necrosis, which may result in delayed perforation and sepsis.
■The role of the assistants is also important in the prevention of complications. In the laparoscopic approach, all instruments, including those handled by assistants, should be moved only under direct vision. Retraction of the liver and stomach and elevation of the spleen require constant concentration to avoid lacerations with subsequent hemorrhage or perforation and jeopardizing the performance of partial splenectomy.

Splenic Preservation and Splenic Trauma
Craig P. Fischer, Frederick A. Moore
Indications and Contraindications
Indications |
■ |
Injuries to the spleen, when patients are hemodynamically stable. |
|
|
Hemodynamic instability |
Contraindications |
■ |
|
|
■ |
Life-threatening concomitant injuries which are likely to cause hemodynamic |
|
|
compromise in the postoperative period, e.g., severe liver injuries or significant |
|
|
pelvic fractures |
|
■ |
Coagulopathy – the most common cause of coagulopathy in this patient group is |
|
|
hypothermia |
|
■ |
Grade V injuries or the pulverized spleen |
Preoperative Investigation and Preparation for the Procedure
Clinical Evaluation
■Hemodynamic status, mechanism of injury, other trauma, co-morbidities, age
■Patients who fail non-operative management of blunt splenic injury are usually good candidates for attempted splenic repair. Splenic salvage may also be appropriate when laparotomy is performed for other indications such as penetrating abdominal injury or bowel injury
CT Scan
■Hemodynamically stable patients should undergo a CAT scan of the abdomen and pelvis with oral and intravenous contrast.
■Two large bore intravenous catheters should be placed as well as an indwelling urinary catheter and nasogastric tube.
974 |
SECTION 7 |
Spleen |
|
|
|
|
Procedure |
|
|
|
|
STEP 1 |
Incision – midline |
|
|
A subcostal incision should not be used in trauma, even if the only suspected injury on |
|
|
||
|
preoperative investigations is a splenic injury. |
|
Exposure
See chapter “Open Splenectomy.”An initial exploratory laparotomy is performed. The left upper quadrant should be initially packed with laparotomy pads, then the
self-retaining retractor adjusted to facilitate exposure of the left upper quadrant. Gentle pressure on the area of splenic injury with a laparotomy pad will help decrease blood loss.
Mobilization
See splenic mobilization in the chapter “Open Splenectomy.”
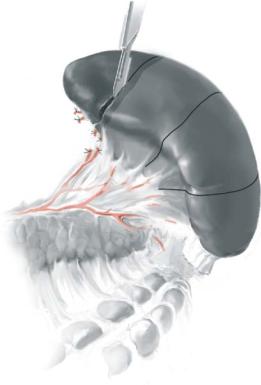
STEP 2
The lesser sac is entered, somewhat to the left along the greater curvature. The use of an endovascular stapling device will facilitate this step as it is long, and capable of angulation. Generally two applications of a 45-mm stapler will allow rapid, wide access to the lesser sac. The splenic artery superior to the pancreas should be identified and may be temporarily clamped if significant bleeding is encountered (see chapter “Open Splenectomy”). Be sure the artery is dissected away from the pancreas and does not contain arteriosclerotic plaque before clamping.
Splenic Preservation and Splenic Trauma |
975 |
|
|
STEP 3
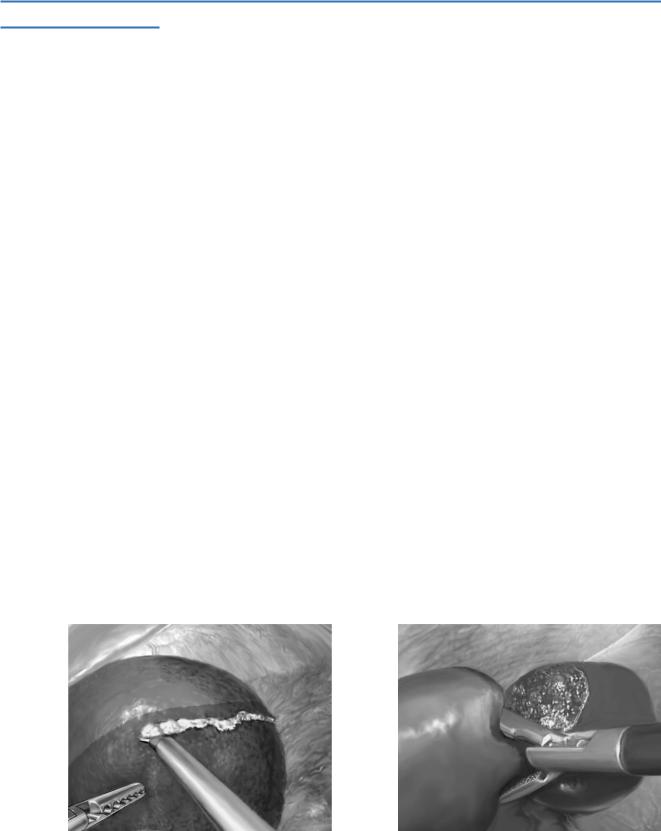
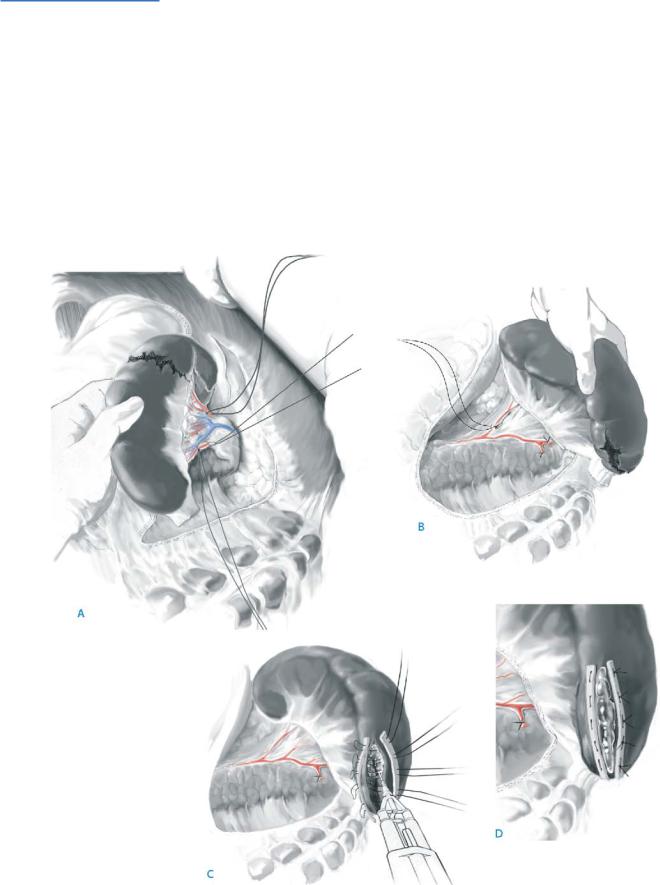
With complete splenic mobilization, the spleen is grasped (A). Again, a laparotomy pad is applied to the area of injury. Initial attempts to control bleeding may include simple hemostatic agents, the use of the argon beam coagulator for surface injuries, and suture ligation for deep parenchymal injuries.
If injury is to a single pole of the spleen, the distal polar branches of the splenic artery may be ligated within the lesser sac, close to the splenic hilum (B). Again, the addition of hemostatic agents and gentle pressure is used.
If initial attempts at hemostasis are unsuccessful, a pledget repair may be used (C, D). The splenic capsule in adults will not hold a stitch – use an appropriate pledget, such as Teflon, felt or autogenous tissue (e.g., posterior rectus sheath). A horizontal mattress technique is used with 3-0 Prolene.
Prior to tying the knots, fibrin glue should be applied to the cleft or site of injury (C). The use of a spray applicator for the application of fibrin glue is recommended, but
not necessary.
Splenic Preservation and Splenic Trauma |
977 |
|
|
Postoperative Tests
See chapter “Open Splenectomy.”
Postoperative Complications
See chapter “Open Splenectomy.”
■Splenic infarction or splenic abscess is uncommon after splenic repair.
■Postoperative bleeding requiring reexploration. If bleeding (or fresh clot) at site of repair, splenectomy is indicated.
Tricks of the Senior Surgeon
■Do not repair a spleen if it is not bleeding.
■When performing splenic repair early in one’s experience, choose the right patient. This generally is a young patient with few other life-threatening injuries.
■Do not accept blood loss while performing the repair – if you cannot quickly stem major hemorrhage, remove the spleen.
■If the patient continues to bleed postoperatively, reoperate promptly.
■When performing ligation of a branch of the splenic artery, or indeed the main artery and splenic vein, do not divide the short gastric vessels.

Laparoscopic Unroofing of Splenic Cysts
Marco Decurtins, Duri Gianom
Indications and Contraindications
Indications |
■ |
Nonparasitic cyst >5cm with and without symptoms |
|
■ |
Nonparasitic cyst <5cm with symptoms |
|
■ |
Parasitic cyst |
|
■ |
Cyst-related complications (spontaneous or traumatic rupture, abscess formation) |
|
■ |
Neoplastic cysts |
Preoperative Investigations/Preparation
■ Serological testing for echinococcus
