
clavien_atlas_of_upper_gastrointestinal_and_hepato-pancreato-biliary_surgery2007-10-01_3540200045_springer
.pdf958 |
SECTION 7 |
Spleen |
|
|
|
|
|
|
Postoperative Tests |
|
|
|
■ |
Monitor in high dependency unit |
|
|
■ |
Monitor platelets and hemoglobin |
|
Complications
■Bleeding
■Pancreatitis
■Pancreatic fistula
■Colonic or gastric perforation
■Subphrenic abscess
■Wound infection
■Atelectasis
■Left pleural effusion
■Postsplenectomy sepsis
■Thrombocytosis
Open Splenectomy |
959 |
|
|
Tricks of the Senior Surgeon
■If bleeding is excessive and control of the splenic artery has not already been secured, or is not immediately feasible, the splenic artery and veins are easily controlled by gentle pressure applied between the second and third fingers of the surgeon’s right hand.
■Control of the splenic artery is most easily accomplished near its origin through the gastrohepatic ligament posterior to the lesser curvature of the stomach
(see STEP 1), which is particularly useful during splenorrhaphy.
■Another approach to the splenic hilum is anteriorly which carries increased risk as the splenic vein is immediately posterior to the splenic artery near the hilum and the tail of the pancreas is also intimately associated to the splenic hilum.
■A linear stapler, as with laparoscopic splenectomy, is particularly useful when expeditious division of the hilum is necessary to control hemorrhage.
■For patients in whom difficulty gaining vascular control is anticipated, for those with enormous splenomegaly or those with portal hypertension, splenic artery embolization done immediately prior to the operation can reduce splenic sequestration, congestion and bleeding.
■Early ligation of the splenic artery diminishes blood loss, maximizes the amount of blood in the spleen returning to the patient, decreases the size of the spleen, improves ease of handling, facilitates removal and improves transfusion efficiency of blood products sooner rather than later during the procedure,
if necessary.
■Make a thorough search for accessory spleens before and after the spleen is removed, especially when operating for hematological indications. Accessory spleens are found in 15–35% of patients undergoing splenectomy and higher in those with hematological diseases. In order of decreasing frequency, accessory spleens are found in the splenic hilum, the splenorenal ligament, the greater omentum, the retroperitoneum near the tail of the pancreas, and the splenocolic ligament. Less commonly, accessory spleens are found in the mesentery of the small and large intestine, as well as the pelvis, in particular the left ureter and left adnexa, and left gonads.
■Mobilize the splenic flexure and the rest of the colon whenever necessary. Be just as careful protecting the colon and the stomach to prevent injury to either hollow viscus.

962 |
SECTION 7 |
Spleen |
|
|
|
STEP 2 |
Exposure |
|
|
|
|
No retractors are required. In the lateral position gravity enhances exposure of the posterior splenic attachments. A blunt ended 5-mm-diameter grasping instrument is placed through the most medial port is used to manipulate the spleen, lifting it upwards to expose the hilum, or rotating it towards the midline to expose the posterior attachments. A search for accessory spleens (see “Open Splenectomy,”“Tricks of the Senior Surgeon”) should be made before commencing dissection of the spleen, as accessory spleens are more easily identified at this stage, and they should be removed as soon as they have been found. Removal later in the procedure can be more difficult.
With the spleen rotated towards the midline, the posterior peritoneal attachments are divided 5–10mm away from the splenic capsule using a diathermy hook or ultrasonic shears. The spleen is progressively mobilized towards the midline, exposing the “splenic mesentery,” which contains the main splenic vessels inferiorly, the short gastric vessels superiorly, and the tail of the pancreas. For adequate mobilization it is necessary to divide the posterior splenic attachments up to the left side of the oesophageal diaphragmatic hiatus superiorly (see “Open Splenectomy,” STEP 3). A combination
of gravity and rotation of the spleen displays an avascular fascial plane behind the splenic mesentery.
It is important to avoid damage to the tail of the pancreas during this dissection. If bleeding occurs during this step, then dissection is in an incorrect tissue plane.

Laparoscopic Splenectomy |
963 |
|
|
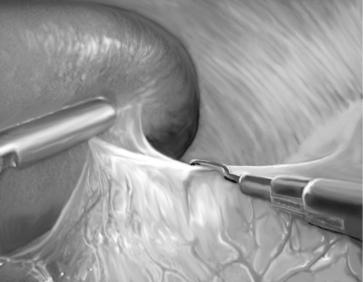
STEP 3 |
The vascular attachments are divided next using a 30or 45-mm endoscopic linear |
|
cutting stapler (white cartridge) |
|
|
|
This is applied sequentially across the splenic mesentery commencing inferiorly, and |
|
multiple applications of the stapler are required (usually three to five). The stapler is |
|
placed adjacent to the splenic capsule at the hilum, to minimize the risk of damaging the |
|
pancreatic tail. When applying the stapler, the spleen is lifted up by a blunt instrument |
|
passed through the most medial port. With this technique, dissection of individual |
|
splenic vessels is not necessary. Furthermore, attempts to dissect individual vessels may |
|
result in vessel damage and hemorrhage. If, when sequentially applying the stapler, |
|
it becomes apparent that the spleen has not been adequately mobilized superiorly, |
|
additional division of the posterior attachments to the upper spleen is then completed |
|
to enable final division of the short gastric blood vessels, and complete separation of |
|
the spleen from its remaining attachments. |
964 |
SECTION 7 |
Spleen |
|
|
|
STEP 4 |
The spleen is next placed in a large specimen retrieval bag |
|
|
|
|
An AutoSuture Endocatch II retrieval bag (U.S. Surgical, Norwalk, CT, USA) is positioned underneath the spleen, and then opened so that the spleen drops directly into the bag as the bag is opened. Other specimen bags require additional manipulation to get the spleen into the retrieval bag and are more difficult to use. The neck of the bag is then pulled out through the lateral 12-mm port wound.

Laparoscopic Splenectomy |
965 |
|
|
STEP 5 |
Morcellation of the spleen |
|
The surgeon’s index finger is placed inside the bag and through the port wound, to break |
|
|
|
the spleen into pieces. This is done bimanually with the left hand pushing against the |
|
abdominal wall, and the right index finger pushing the spleen against the abdominal |
|
wall. Blood released from the broken spleen is then aspirated and an empty sponge |
|
holding forceps is used to remove the spleen in pieces. The surgeon must be careful |
|
to avoid spillage of splenic material into the abdominal cavity, which can occur if the |
|
specimen bag is broken. An alternative method for spleen removal is to remove the |
|
spleen intact through a muscle-splitting abdominal incision, usually in the left lower |
|
quadrant. |
966 |
SECTION 7 |
Spleen |
|
|
|
|
Tricks of the Senior Surgeon |
|
■This procedure is most suitable for spleens which are normal in size or only mildly enlarged. The size of the spleen is best assessed before surgery with patients in the lateral position. If the spleen is easily palpable then it may be too big for laparoscopic dissection of the hilum in the lateral position.
Partial Splenectomy, Open and Laparoscopic
Eric C. Poulin, Christopher M. Schlachta, Joseph Mamazza
Indications and Contraindications
Indications |
Trauma |
|
|
■ |
Selected Class II–III–IV splenic injury with the following: |
|
■ |
Hemodynamic stability |
|
■ |
No evidence of other intra-abdominal organ injury |
|
■ |
No associated head injury |
|
■ |
No coagulopathy |
|
■ |
CT confirmation of isolated splenic injury |
Elective
■Resection of non-parasitic cysts
■Hamartomas and other benign splenic tumors
■Inflammatory pseudotumor of the spleen, Type J Gaucher’s disease
■Cholesteryl ester storage disease, chronic myelogenous leukemia
■Thalassemia major, spherocytosis, staging of Hodgkin’s disease in children
Contraindications |
■ |
Inadequate exposure |
|
■ |
Inability to mobilize the spleen and tail of pancreas to the midline |
|
■ |
Inability to leave >25% of splenic mass for complete splenic function |
|
Still being defined. |
|
Indications for |
||
Laparoscopic Partial |
|
|
Splenectomy |
|
|
Preoperative Investigation and Preparation for the Procedure
See chapter “Open Splenectomy.”
968 |
SECTION 7 |
Spleen |
|
|
|
|
Procedure |
|
|
|
|
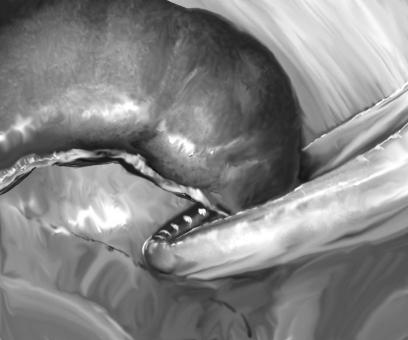
STEP 1 |
Planning the partial splenectomy |
|
|
Assuming that the spleen is appropriately placed for full evaluation and that hemostasis |
|
|
||
|
is adequate, the planning for partial splenectomy can start. In trauma cases, it will be |
|
|
dictated by the extent of the injury and in elective cases by the nature of the underlying |
|
|
pathology. |
|
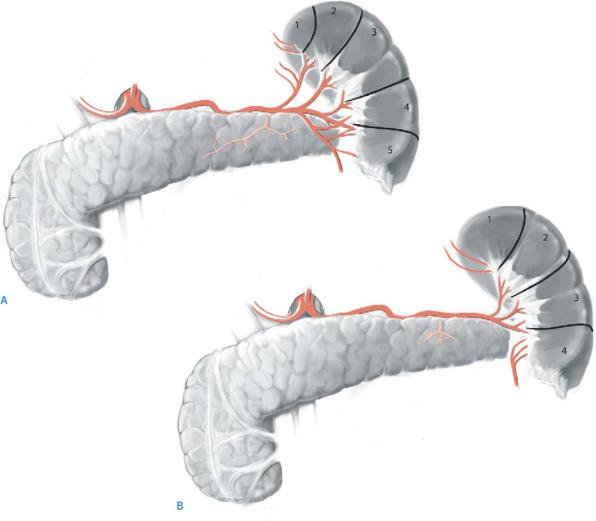
The spleen in the majority of cases can be divided into independent lobes or segments, each with its own terminal blood supply (A, B). The superior pole is supplied by the short gastric vessels and the lower pole by branches of the gastroepiploic artery (up to five) known to anastomose with the inferior polar artery. In addition, most patients, despite possible variations, have two or three major vessels entering the hilum. Therefore there are usually four or five regions or lobes available for partial splenectomy. It is also important to understand that these vessels lie in different supportive ligaments. Vessels to the superior pole (short gastrics) and inferior pole (gastroepiploic branches) rest in the gastrosplenic ligament, whereas the splenic branches proper lie in the splenorenal ligament with the tail of the pancreas.
