
clavien_atlas_of_upper_gastrointestinal_and_hepato-pancreato-biliary_surgery2007-10-01_3540200045_springer
.pdf
Distal Pancreatectomy |
945 |
|
|
STEP 6
An Endo GI stapler is passed through the left-sided 12-mm port and fired across the body of the pancreas medial to the pancreas to be resected. Other techniques such as tissue welding may be used to transect the pancreas and “close” the end of the gland.
946 |
SECTION 6 |
Pancreas |
|
|
|
|
|
|
Postoperative Considerations |
|
|
|
■ |
Admission to a routine postsurgical ward if the patient is stable |
|
|
■ |
Nasogastric suction for 24h is optional, usually not necssary |
|
|
■ |
Liquid diet beginning postoperative day 1; advance as tolerated |
|
|
■ |
Watch for pancreatic fistula (amylase-rich fluid from drain) |
|
|
■ |
Discharge 5–6days postoperatively |
|
Local Postoperative Complications
■Short term:
–Pancreatic leak/fistula from proximal pancreatic remnant
–Left subphrenic abscess (rule out pancreatic ductal leak)
–Thrombocytosis secondary to splenectomy
–Intra-abdominal hemorrhage (especially if splenic vein thrombosis with sinistral portal hypertension is present preoperatively)
■Long term:
–Diabetes mellitus
–Maldigestion/malabsorption/steatorrhea or malnutrition from development of exocrine insufficiency secondary to pancreatic parenchymal resection with diseased remaining pancreas

Distal Pancreatectomy |
947 |
|
|
Tricks of the Senior Surgeon
Open Distal Pancreatectomy
■The major intraoperative problems that occur during distal pancreatectomy are injuries to the major veins from excessive traction or incorrect dissection. Early identification of the superior mesenteric vein and development of the tunnel where the superior mesenteric vein passes beneath the pancreas is an important maneuver to be sure of the location of this major venous structure as the dissection proceeds. This allows for rapid division of the pancreatic parenchyma over the vein if necessary to achieve vascular control.
■Because of the risk of vascular injury during distal pancreatectomy, an assortment of vascular clamps should be readily available on the back table; the surgeon should familiarize himself or herself with the selection of clamps before the operation begins.
■Sometimes, a posterior pseudocyst near the tail of the gland close to the splenic hilum or severe chronic inflammation will make it essentially impossible or inadvisable to mobilize the spleen safely from lateral to medial as suggested. In this case, it is sometimes more prudent to try to enter the retropancreatic space more medially, closer to the superior mesenteric vein. If possible, one can establish the proper plane of dissection there and move from medial to lateral behind the pancreas, remembering that the renal vein is at potential risk if the dissection goes too deep. It is important to stay close to the back of the pancreas.
■The spleen is sometimes injured during its mobilization, and it can be tempting to remove the spleen to reduce annoying bleeding. However, the spleen makes a nice “handle” for the distal pancreas and it is best to leave it in situ for the remainder of the dissection. Bleeding can often be controlled with a laparotomy pad on the spleen and manual pressure. Another option is to locate and ligate the proximal splenic artery to diminish splenic arterial inflow.
Laparoscopic Distal Pancreatectomy
■Laparoscopic surgery on solid abdominal organs is facilitated greatly by introducing the hand into the abdomen (hand-assisted technique).
■Hand-assisted laparoscopy allows:
–Manipulation of large organs (colon, stomach, liver, spleen, and pancreas)
–Control of hemostasis should a vessel bleed significantly during dissection; during distal pancreatectomy, branches of the splenic vein can cause considerable bleeding, controlled easily by pressure of the thumb and not easily controlled by a laparoscopic instrument.
–Use of proprietary abdominal wall sealing devices is available for handassisted laparoscopy but are not mandatory. If the incision in the abdominal wall and muscles is made small enough, introduction of the hand through a small incision easily maintains the pneumoperitoneum. In addition, the abdominal wall can be lifted with the forearm to create extra working space in the abdomen.

SECTION 7
Spleen
Robert Padbury

Introduction
Robert Padbury
Total splenectomy has been considered the appropriate management for splenic trauma, diseases, or disease processes that could be modified by splenectomy. This surgical truism has been supported by the belief that the spleen is not essential to life, that mortality is almost universal in non-operated splenic injury and that delayed rupture
is a significant danger.
The policy for total splenectomy has been progressively modified by a number of important observations; first, that splenectomy increases the risk of significant septic events and, second, that partial splenectomy or even splenic preservation is possible with low risk to the patient. Major advances in abdominal imaging have contributed significantly to the surgical developments.
Progress has continued with the development of laparoscopic surgery. Initially laparoscopic total splenectomy became a relatively standard procedure, particularly in the non-trauma patient. More recently the concept of partial splenectomy has been successfully used using laparoscopic access. As with other organ systems, laparoscopic surgery served as a stimulus for equipment development, and the benefits of this have been realised in both open and laparoscopic procedures. Particularly valuable in splenic surgery are the endovascular stapling devices.
When considering a patient for splenectomy, decisions regarding the choice of access should take into account the experience and training of the surgeon, as well as the suitability of the patient. The size of the spleen, the nature of the problem and previous abdominal surgery will be factors in the decision. Clearly, appropriate and specific informed consent is mandatory, including a discussion of total splenectomy when a partial procedure is planned.
In this section of the atlas a range of techniques for splenectomy, open and laparoscopic, total and partial, are discussed. Techniques for splenic preservation are described and finally some approaches for splenic cysts are presented.

Open Splenectomy
Scott F. Gallagher, Larry C. Carey, Michel M. Murr
Indications and Contraindications
Indications |
■ |
Trauma |
|
|
|
■ |
Blood dyscrasias, e.g., idiopathic thrombocytopenic purpura |
|
|
■ |
Symptomatic relief, e.g., Gaucher’s disease, chronic myeloid or lymphatic leukemia |
|
|
■ |
Splenic cysts and tumors |
|
|
|
No absolute contraindications for splenectomy |
Contraindications |
■ |
||
|
|
■ |
Limited life expectancy and prohibitive operative risk |
|
|
|
Previous open upper abdominal surgery |
Contraindications to |
■ |
||
Laparoscopic Splenectomy |
■ |
Uncontrolled coagulation disorder |
|
|
|
■ |
Very low platelet count (<20,000/100ml) |
|
|
■ |
Massive splenic enlargement, i.e., spleen greater four times normal size |
|
|
|
or larger |
|
|
■ |
Portal hypertension |
Preoperative Investigation and Preparation
■Imaging studies to estimate the size of the spleen or extent of splenic injury and other abdominal injuries in trauma cases
■Interpretation of bone marrow biopsy, peripheral blood smear, and ferrokinetics in coordination with a hematologist
■Discontinue anticoagulants (such as aspirin, warfarin, clopidogrel and vitamin E)
■Patients routinely given polyvalent pneumococcal vaccine, Haemophilus influenzae b conjugate vaccines and meningococcal vaccines on the same day at least 10–14days prior to splenectomy (given postoperatively in trauma cases)
■Prophylactic antibiotics (cefazolin or cefotetan)
■Perioperative DVT prophylaxis
■Perioperative steroids should be administered to patients on long-term steroid therapy

954 |
SECTION 7 |
Spleen |
|
|
|
|
Procedure |
|
STEP 1
The standard supine position is employed with an optional small roll/bump under the left flank.
The patient should be well secured to the operating table should it become necessary to tilt the table to improve visualization of the operative field.
Mechanical retractors greatly enhance exposure and the primary surgeon should stand on the right side of the patient; the first assistant opposite the surgeon on the left side of the patient.
There are two standard incisions for open splenectomy: a supraumbilical midline or left subcostal with or without midline extension. A midline incision is usually employed in trauma cases.
Examine each patient following induction of anesthesia to estimate the location of the splenic hilum and the tip of the spleen, so the incision location optimizes exposure. The principle of retraction is that of moving the incision over the operative field.
Two points of retraction include one retractor to gently hold the colon in the lower abdomen and counterretraction to lift the left portion of the incision superiorly and out of the operative field.
The standard order of steps is arranged to minimize blood loss, minimize the size of the spleen and maintain adequate exposure while performing the deepest and most challenging dissection.
Identify the splenic artery near its origin from the celiac axis, which is accessed through the gastrohepatic ligament (A, B).

Open Splenectomy |
955 |
|
|
STEP 2
Upon entering the peritoneal cavity and again before closing, a thorough search for accessory spleens should be conducted, especially if the indication for splenectomy is hematological.
Open the gastrosplenic ligament through an avascular area and then proceed to dissect the short gastric vessels. These may be secured with hemoclips or ligatures.
The last several vessels in the gastrosplenic ligament are of particular note. These branches are often quite short, so care must be taken to utilize adequate tissue
for hemostasis without injuring the greater curvature of the stomach. The LigaSure (R) device, the harmonic/ultrasonic scalpel or a linear stapler can also be utilized for dividing the gastrosplenic ligament as is employed during laparoscopic splenectomy.

Open Splenectomy |
957 |
|
|
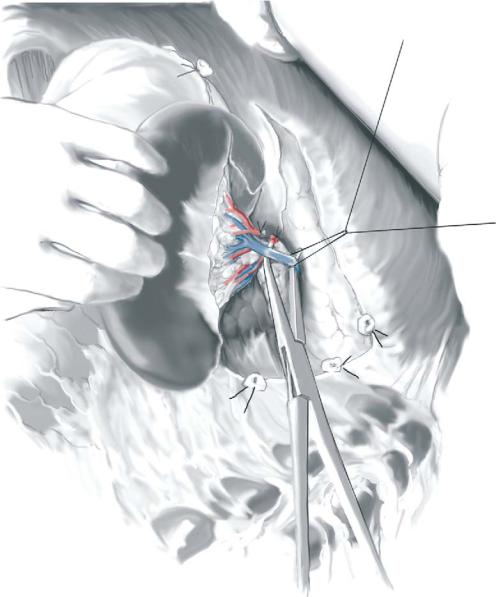
STEP 4 |
Control of the splenic hilum |
|
Once all of the splenic attachments have been divided the splenic hilum can be |
|
|
|
addressed definitively. Lift the spleen up and out of the retroperitoneum. This maneuver |
|
serves to clearly identify and separate the splenic vessels from the tail of the pancreas as |
|
shown. Laparotomy pads packed into the retroperitoneum can assist with elevating the |
|
spleen into the incision while controlling oozing in the retroperitoneum. With the assis- |
|
tant holding the spleen, the surgeon can separate the tail of the pancreas from the |
|
splenic vessels in order to protect the tail of the pancreas prior to dissecting and |
|
applying curved clamps. The surgeon divides the splenic artery and vein proximal to |
|
their bifurcation between clamps and applies a suture ligature to each after removing |
|
the spleen. We first clamp the artery, which is typically anterior to the splenic vein, and |
|
then squeeze the spleen in order to promote autotransfusion of splenic blood prior to |
|
clamping the vein. |
|
Once the spleen is removed and all of the named vessels have been doubly ligated, |
|
the operative field can be inspected for hemostasis. The abdomen is closed with or |
|
without a closed suction drain. |
