
clavien_atlas_of_upper_gastrointestinal_and_hepato-pancreato-biliary_surgery2007-10-01_3540200045_springer
.pdf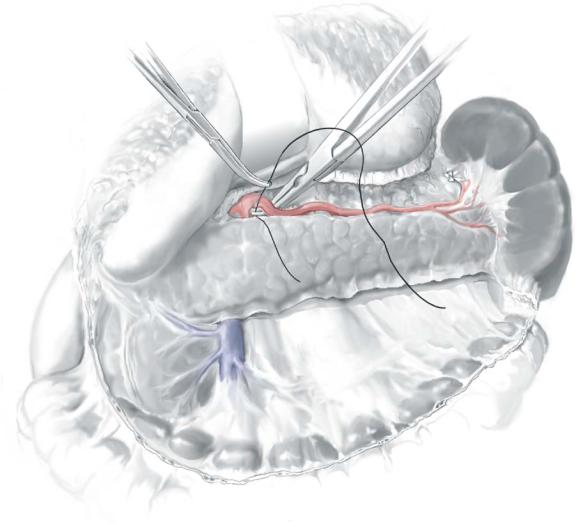
Distal Pancreatectomy |
935 |
|
|
STEP 5 |
Ligation of the splenic artery |
|
Along the upper border of the pancreas, the splenic artery is isolated near its origin |
|
|
|
from the celiac axis before it enters the pancreatic substance; here it is suture-ligated |
|
proximally with 2-0 suture, ligated distally, and divided. Be certain to fully identify |
|
the artery as the splenic artery and to clearly distinguish it from the common hepatic |
|
artery. |


Distal Pancreatectomy |
937 |
|
|
STEP 7 |
Division of the pancreas |
|
The neck of the pancreas is divided over the superior mesenteric–portal vein using |
|
|
|
electrocautery; a large clamp behind the neck of the pancreas protects the vein. |
|
If a neoplasm is suspected, a margin of at least 1cm to the left of any mass must be |
|
maintained and checked with frozen section of the transected margin. |
|
Marginal arteries supplying the pancreas that bleed after the parenchyma is divided |
|
are controlled with suture ligatures. |
|
Once the cut edge of the pancreas is hemostatic, the pancreatic duct orifice is |
|
identified and ligated with 3-0 polypropylene. |
|
The cut edge of the pancreas is closed with a continuous running suture of 3-0 |
|
polypropylene. |
|
Other methods to transed it and “close” the cut edge of the pancreas include using a |
|
linear stapler or techniques of tissue welding. A soft, closed-suction drain is placed adja- |
|
cent to the cut edge of the pancreas and brought out through the left lateral abdominal |
|
wall. |
|
The abdominal wall is closed in layers. |
938 |
SECTION 6 |
Pancreas |
|
|
|
Distal Pancreatectomy with Splenic Preservation
■Preserving the spleen during removal of the body/tail of the pancreas in patients with chronic pancreatitis is difficult; scarring around the splenic vein may make dissection and preservation of the vein difficult and even dangerous.
■If a neoplasm is suspected, the spleen and splenic vessels should not be preserved.
■If the distal pancreatectomy is for pain, there is no suspicion of malignancy, and the splenic vein is patent, an attempt to preserve the spleen is justified.
■The course of the operation is quite different when splenic preservation is the goal.
■After entering the lesser sac, the operation commences with division of the pancreatic neck over the isolated superior mesenteric-portal vein.
■The spleen is not mobilized; the body/tail of the pancreas is dissected from the point of division of the gland toward the spleen by dividing the multiple small branches entering the splenic vein from the pancreatic parenchyma.
■Branches of the splenic artery entering the pancreas are divided individually as dissection progresses to the patient’s left.
■Before proceeding with dissection of the body/tail of the gland from the splenic vessels, it is wise to gain control of both the proximal splenic vein near its entrance to the SMV and the splenic artery near its origin; expeditious vascular control can be obtained if bleeding becomes excessive during subsequent dissection.
■Splenic venous branches are controlled best with fine vascular staples or fine ties of 4-0 or 5-0 silk; these vessels are small, delicate, and easily torn.
■The surgeon decides how much blood loss is acceptable when trying to preserve the spleen and should be willing to abandon this approach if necessary.

Distal Pancreatectomy |
939 |
|
|
|
Laparoscopic Distal Pancreatectomy |
|
Ronald A. Hinder |
|
The advent of minimal access surgery and its technologic advances have made laparo- |
|
scopic distal pancreatectomy a viable option in selected patients with chronic pancre- |
|
atitis and other disorders. |
|
|
STEP 1 |
Peritoneal access |
|
Access to the abdominal cavity is obtained by making an incision below the umbilicus |
|
|
|
in the midline and establishing a 15-mmHg pneumoperitoneum; the laparoscope is |
|
introduced through a 10-mm port |
|
Further ports include right upper and right mid quadrant 5-mm ports in the |
|
mid-clavicular line and a 12-mm port in the left lower mid quadrant. |
|
The abdomen is explored laparoscopically for evidence of metastatic disease on |
|
the peritoneal surface or within the liver; the spleen is also examined. |
|
The adhesions are divided as needed. |

940 |
SECTION 6 |
Pancreas |
|
|
|
STEP 2 |
Entering the lesser sac |
|
|
|
|
The gastrocolic omentum is divided using an ultrasonic dissector (harmonic scalpel), allowing access to the lesser sac behind the stomach.
The stomach is retracted rostrally by the assistant, and the lesser sac and anterior surface of the pancreas are explored laparoscopically.
The lesion in the tail of pancreas may then become obvious.
Should the lesion not be obvious, laparoscopic ultrasonography can help localize the site of the lesion.
Laparoscopic ultrasonography should also be used to explore the liver if the possibility of metastasis from the malignant tumor exists.
The posterior peritoneum along the inferior surface of the pancreas is incised toward the spleen.
The pancreas is mobilized gently by lifting it off the posterior, retroperitoneal soft tissues, and the feasibility of laparoscopic resection is confirmed.

Distal Pancreatectomy |
941 |
|
|
STEP 3 |
Hand-assisted technique |
|
A McBurney incision is made in the right lower quadrant using a muscle-splitting |
|
|
|
technique; the size of the incision (4–5cm) should fit snugly around the surgeon’s wrist. |
|
The surgeon’s hand is introduced into the peritoneum by sliding between the abdom- |
|
inal muscles, keeping a tight fit with the skin around the wrist to prevent leakage of gas; |
|
commercially available seals may facilitate this maneuver. |
|
The abdomen is then explored manually. |
|
The hand further dissects the body/tail bluntly, then grasps the pancreas; the stomach |
|
is retracted with the back of the hand. This technique involves a medial-to-lateral |
|
approach to distal pancreatectomy, with mobilization from the body to tail/spleen, not |
|
vice versa. |
|
An ultrasonic dissector facilitates further dissection. |

942 |
SECTION 6 |
Pancreas |
|
|
|
STEP 4
The pancreas is fully dissected into the splenic hilum.
The spleen is mobilized off the retroperitoneum and from attachments to the diaphragm, kidney, and colon by dividing the lienophrenic, lienorenal, and lienocolic ligaments with the ultrasonic dissector; hand manipulation assists these maneuvers.
A sterile specimen bag or sterilized plastic bowel bag inverted over the surgeon’s left hand is introduced into the right-sided hand incision and the specimen grasped; as the hand is removed slowly, the bag falls over the specimen, keeping the wound from the surface of the specimen.

Distal Pancreatectomy |
943 |
|
|
STEP 5
The splenic vein is identified posterior to the pancreas; when possible, the small veins passing to the posterior surface of the pancreas are divided using the ultrasonic dissector when a spleen-preserving resection is contemplated. If it is not possible to separate the vein from the pancreas or for potentially malignant neoplasms, the vein should be resected with the specimen. The vein is ligated either with an intracorporeal knot or a vascular stapler (A-1).

944 |
SECTION 6 |
Pancreas |
|
|
|
STEP 5 (continued)
The splenic artery is identified; it often takes a serpiginous course along the upper border of the pancreas. If a splenectomy is planned, the splenic artery is isolated and divided using the ultrasonic dissector or ligated using intracorporeal knot tying techniques; others divide the splenic artery with a stapler using a vascular load (A-2).
When the spleen is to be preserved, the pancreas is separated from the intact splenic artery and vein using the ultrasonic dissector until the distal pancreas is completely isolated and free of all attachments.
When the spleen is to be removed with the specimen, dissection should proceed outside of these vessels, leaving the splenic artery and vein attached to the tail of the pancreas.
