
clavien_atlas_of_upper_gastrointestinal_and_hepato-pancreato-biliary_surgery2007-10-01_3540200045_springer
.pdf
872 |
SECTION 6 |
Pancreas |
|
|
|
STEP 8 |
Thumb-index measurement for depth |
|
|
|
|
The duct of Wirsung guides the proper depth of excavation/resection, ducts of Wirsung and the uncinate process are adjacent to the posterior capsule and are opened (decompressed); the duct of Santorini is excised.
A limited cuff of pancreatic tissue may be left between the cored-out head of
the pancreas and duodenum. Sufficient pancreatic tissue usually remains to preserve the important pancreatoduodenal arcade, which maintains the viability of the mid-duodenum.
Chronic Pancreatitis |
873 |
|
|
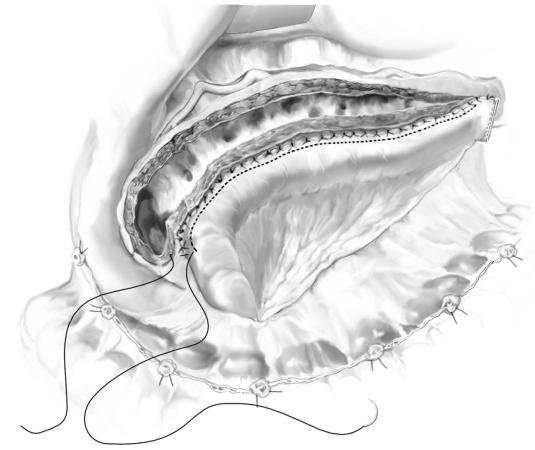
STEP 9 |
Reconstruction with Roux-en-Y drainage of the head of the pancreas |
|
with pancreaticojejunostomy – the outer layer of the anastomosis |
|
|
|
The Roux limb is brought through the transverse mesocolon to lie over the entire |
|
pancreas. |
|
A two-layer pancreaticojejunostomy is performed with an outer layer of interrupted, |
|
Lembert 3-0 silk sutures, approximating the jejunal serosa to the capsule of the |
|
pancreas; the wall of the duodenum may be included with the pancreas in this layer. |
|
Inflammation and edema may render distinction between the duodenum and the |
|
pancreas less well-defined. |
874 |
SECTION 6 |
Pancreas |
|
|
|
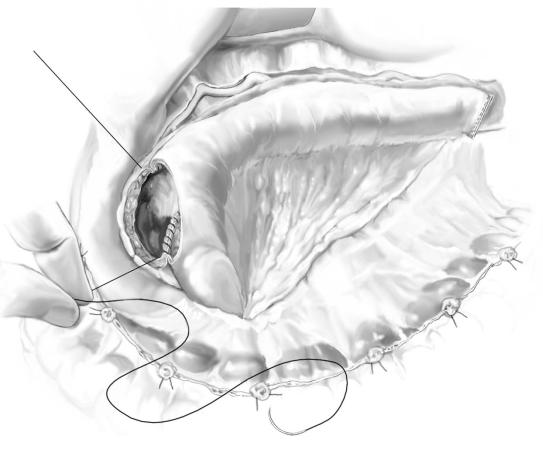
STEP 10 |
Pancreaticojejunostomy – inner layer of anastomosis |
|
|
|
|
A running, 3-0 absorbable suture attaches the full thickness of the jejunum to the cut surface of the pancreas along the capsule, continuing along the cored-out head of pancreas; a formal pancreatic duct-to-jejunal anastomosis is not necessary.
Sewing the jejunum to the capsule of pancreas rather than to the pancreatic duct allows decompression of the ducts as small as 2–3mm in diameter (relief of the pancreatic compartment syndrome).
If only the pancreatic head is diseased or if the patient has had a distal pancreatectomy, then only a coring out of the head is necessary with the head drained into the Roux limb.
The jejunal Roux limb is anchored to the transverse mesocolon to prevent internal herniation.
Continuity of the GI tract is reestablished by end-to-side jejunojejunostomy 60–70cm distal to the pancreaticojejunostomy; all mesenteric defects are closed.
No drain is needed unless a choledochotomy has been performed.

Chronic Pancreatitis |
875 |
|
|
Procedure: Non-Anatomic Duodenum-Preserving Head Resection
(The Beger Procedure)
Duodenum-preserving pancreatic head resection was first described by Beger in 1979. The aim of the operation is a subtotal resection of the pancreatic head with removal of the inflammatory mass while preserving the duodenum, extrahepatic common bile duct, gallbladder, and stomach, as well as preserving a portion of the pancreatic parenchyma of the head of the gland.
STEP 1
The head of the pancreas is exposed by dividing the gastrocolic ligament, with care taken to avoid injury to the gastroepiploic vessels. The duodenocolic ligament is transected and the transverse colon handled carefully. Subsequently, a Kocher maneuver is performed. Exposure of the portal vein and the superior mesenteric veins at the inferior margin of the pancreas follows.

876 |
SECTION 6 |
Pancreas |
|
|
|
STEP 2 |
Ligation of feeding vessels |
|
|
|
|
The gastroduodenal artery is ligated at the upper margin of the body of the pancreas. The common hepatic artery is prepared and banded with a loop. The common bile duct is exposed circumferentially at the upper margin of the pancreas in the hepatoduodenal ligament. Next, the plane between the anterior surface of the portal vein and the posterior aspect of the pancreatic head is developed either from above the neck of the gland starting at the portal vein or more commonly starting from below the neck of the gland at the superior mesenteric vein. This maneuver can be quite difficult, especially in cases of inflammatory and edematous reaction in the head of the pancreas.

Chronic Pancreatitis |
877 |
|
|
STEP 3 |
Transection of the neck of the pancreas |
|
The subtotal resection of the pancreatic head is begun by transecting the neck of the |
|
|
|
gland, starting near the duodenal edge of the portal vein in a sagittal plane as shown. |
|
At the cut surface of the left pancreas, meticulous hemostasis using non-absorbable |
|
5-0 or 6-0 monofilament sutures is mandatory. |
878 |
SECTION 6 |
Pancreas |
|
|
|
STEP 4 |
Subtotal excision of the head of gland |
|
|
|
|
The head of the pancreas is rotated ventroinferiorly. This can be achieved by bluntly freeing the head of the pancreas from the portal vein. Small branches entering the portal vein directly must be ligated and divided. The head of the pancreas is released from the retroportal region with little technical difficulty as long as individual dissection of the vessels entering into the portal vein proceeds meticulously. Also, the pancreatic parenchyma is transected along the left lateral wall of the intrapancreatic portion of the distal common bile duct toward the papilla.

Chronic Pancreatitis |
879 |
|
|
STEP 5
Subtotal resection of the pancreatic head is completed by including the tissue of the uncinate process. It is not necessary to preserve the gastroduodenal artery for adequate blood supply to the duodenum because the supraduodenal vessels, as well as duodenal vessels arising from the superior mesenteric artery, maintain sufficient perfusion of the duodenal wall. In most patients it is not difficult to dissect the pancreatic tissue along the wall of the intrapancreatic portion of the common bile duct towards the papilla and further down including the uncinate process. Removal of fibrotic tissue along the common bile duct results in decompression of the duct in most patients. In patients with inflammation in the wall of the common bile duct, the duct is opened by an incision in the lateral wall for an internal biliary bypass. After subtotal resection of the pancreatic head, a 5- to 8-mm shell-like remnant of the pancreatic head between the common bile duct and the duodenal wall remains.

880 |
SECTION 6 |
Pancreas |
|
|
|
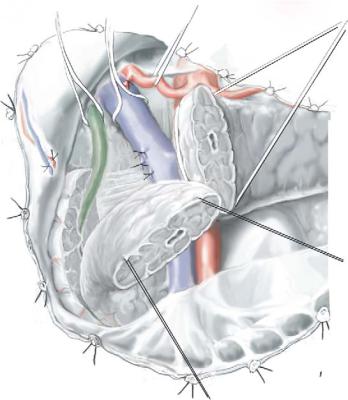
STEP 6 |
Pancreaticojejunostomy |
|
|
|
|
Reconstruction after subtotal resection of the head of the pancreas is initiated by transecting the upper jejunum 40cm distal to the ligament of Treitz. The Roux-en-Y jejunal limb is brought through a retrocolic mesenteric defect. An end-to-side anastomosis between the left pancreas and jejunum is performed (Warren-Cattell). In this instance, a duct-to-mucosa anastomosis between the pancreatic duct and the jejunal mucosa is performed first. The anastomosis is completed with a single-layer seromuscular suture between the jejunum and the capsule of the left pancreas.
A side-to-side anastomosis is made between the jejunal limb and the remnant of the pancreatic head for 5–8cm. The jejunal incision for this anastomosis is 4–8cm long.
A single-layer anastomosis between the jejunum and the pancreas along the incision line serves as the inner layer; the outer layer is performed between the pancreatic capsule and the seromuscularis of the jejunum. For restoration of intestinal continuity, an enteroenterostomy is carried out 40cm distal to the pancreaticojejunal anastomosis.

Chronic Pancreatitis |
881 |
|
|
STEP 7 |
Choledochojejunostomy |
|
For patients with a wide distal pancreatic body/tail remnant, an end-to-side pancreato- |
|
|
|
jejunostomy may be better. Similarly, the intrapancreatic protion of the common bile |
|
duct can be opened in the proximal pancreatic head remnant and included in the prox- |
|
imal side-to-side pancreatojejunostomy. |
|
An additional anastomosis between the suprastenotic portion of the common bile |
|
duct and the jejunal limb is can be carried out in patients in whom the subtotal resec- |
|
tion of the head of the pancreas has not resulted in complete decompression of the |
|
intrapancreatic common bile duct and also when intraoperative examination reveals |
|
fibrotic involvement of the common bile duct proximal to the papilla. The side-to-side |
|
anastomosis between the common bile duct and the jejunum is sutured using a single- |
|
layer technique. In these patients, cholecystectomy is strongly suggested. |
