
clavien_atlas_of_upper_gastrointestinal_and_hepato-pancreato-biliary_surgery2007-10-01_3540200045_springer
.pdf862 |
SECTION 6 |
Pancreas |
|
|
|
|
|
|
|
Absolute contraindications: |
|
Contraindications |
■ |
|
|
|
|
– Findings which raise concern of potential malignancy are absence of history of |
|
|
|
alcoholism, hyperlipidemia, hyperparathyroidism, recent history of onset of pain, |
|
|
|
and increased serum CA 19–9 level |
|
|
|
– If cancer cannot be excluded, a resective operation is suggested, i.e., pancreato |
|
|
|
duodenectomy or distal pancreatectomy |
|
|
|
– Complete thrombosis of superior mesenteric/portal venous junction with |
|
|
|
peripancreatic varices |
|
|
■ |
Relative contraindications: |
|
|
|
– Disease limited to the body and tail of gland (infrequent) |
|
|
|
– Unrelenting narcotic addition or when the patient refuses the concept of |
|
|
|
postoperative detoxification |
|
|
|
– Inability to manage possible postoperative diabetes mellitus due to anticipated |
|
|
|
poor compliance |
|
|
|
– Obstruction of superior mesenteric/portal vein junction with mild to moderate |
|
|
|
portal hypertension |
|
|
|
The “small” pancreatic duct (<3–4mm) in the head, body, or tail of the pancreas is |
|
Other Considerations |
■ |
||
not |
|
|
|
|
|
a contraindication. |
|
|
■ |
Ducts in the pancreatic head (body or tail) are either resected or unroofed and |
|
|
|
thereby decompressed; a jejunal Roux limb can be sewn to the pancreatic capsule. |
|
Chronic Pancreatitis |
863 |
|
|
Preoperative Investigations and Preparation for the Procedure
■Exclude non-pancreatic pain.
■Maximize medical treatment including nutrition, enzyme replacement, and cessation of alcohol intake.
■Assess the extent of chemical dependency (narcotics, alcohol).
■Strive for a preoperative commitment to undergo postoperative alcohol and/or drug rehabilitation.
Preoperative Investigation
■History:
–Exclude alcohol or drug addiction, gallstones, pancreatitis-inducing medications, hyperparathyroidism, hypercalcemia, and hyperlipidemia
–Evaluate for steatorrhea and diabetes mellitus (glucose intolerance), especially the need for insulin
–Severity of pain (Likert visual analog pain scale completed by patient)
–Psychosocial stability
–Quality of life survey (optional)
–European Organization for Research and Treatment of Cancer QLQ-C30 (EORTC)
–Medical Outcomes Trust Short-Form 36 (MOS SF-36)
–Impact of pain on employment, family support, daily activities
■Clinical evaluation:
–Jaundice, ascites, nutritional status, weight, physiologic health, co-morbidities
–Baseline pancreatic exocrine and endocrine function if indicated
■Laboratory tests:
–CA 19–9 (most useful if common bile duct patent), LFTs, HbAIC, glucose tolerance test
–Fecal fat and secretin studies are only required rarely
–Imaging
–Triphasic helical CT to evaluate for:
–Pancreatic masses
–Portal and left-sided hypertension or thrombosis of the splenic vein
–Involvement of adjacent organs
–Extrapancreatic causes of pancreatitis (cholelithiasis)
–ERCP to evaluate pancreatic and biliary ductal systems and esophagogastroduodenoscopy to exclude peptic ulcer disease
–Endoscopic or intraoperative ultrasonography to evaluate for vascular involvement and biopsy if indicated
Preparation for the Procedure
■Broad spectrum, perioperative prophylactic antibiotics
■Full bowel preparation
864 SECTION 6 Pancreas
|
Procedure: Local Resection of the Head of the Pancreas |
|
with Longitudinal Pancreaticojejunostomy (The Frey Procedure) |
|
|
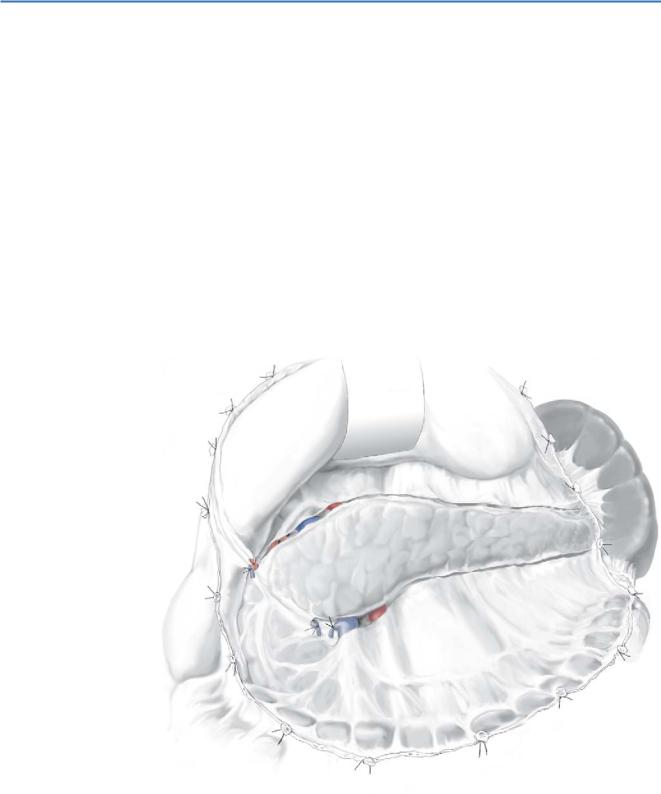
STEP 1 |
Exposure and exploration; assessment and mobilization of pancreas; |
|
entering the lesser sac |
|
|
|
A bilateral subcostal incision is suitable for most patients; a midline incision from |
|
xiphoid to umbilicus is better for patients with vertically oriented costal arches. |
|
Dividing the gastrocolic ligament between hepatic and splenic flexures exposes the |
|
lesser sac. |
|
The right gastroepiploic artery and vein are ligated and divided to expose the ante- |
|
rior surface of the head and neck of the pancreas. |
|
Cephalad retraction of the stomach and caudad retraction of the transverse colon |
|
expose the body and tail of the pancreas. |
|
The inferior border of the body and tail of the pancreas are mobilized to completely |
|
expose the anterior surface of the pancreas. |
Chronic Pancreatitis |
865 |
|
|
STEP 2 |
Exposure of the head of pancreas |
|
The duodenum and head of pancreas are mobilized by an extended Kocher maneuver; |
|
|
|
this maneuver allows manual palpation of both sides of the pancreatic head to deter- |
|
mine the thickness and consistency and to rule out a pancreatic mass. |
|
The gastroduodenal artery may be encircled with a vessel loop should ligation be |
|
necessary for hemostasis (rare) during resection of the head of the gland. |

866 |
SECTION 6 |
Pancreas |
|
|
|
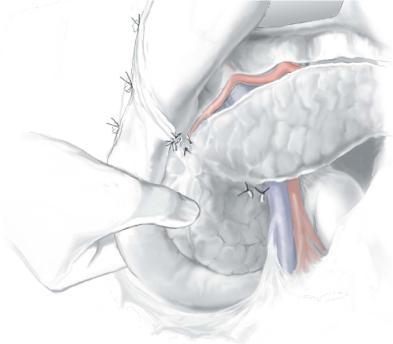
STEP 3 |
Exposure of the SMV alongside the head of the pancreas |
|
|
|
|
Importantly, it is not necessary to free the portal vein beneath the neck of the pancreas. The SMV should be exposed adjacent to the head and uncinate process of the
pancreas to provide optimal exposure.
Exposing the head and uncinate process is important not only for the coring out process, but also to provide an adequate rim of pancreatic tissue to which the Roux-en-Y jejunal limb is to be sewn.
Free up the small veins and arteries from the head side of the SMV (arteriovenous tributaries).
Divide the venous tributaries to the SMV from the third portion of the duodenum inferiorly; note that the inferior pancreatoduodenal artery on occasion may run anterior rather than posterior to the SMV.

Chronic Pancreatitis |
867 |
|
|
STEP 4 |
Locating the main pancreatic duct (A-1, A-2) |
|
To find the pancreatic duct, the main duct in the body of pancreas is usually located |
|
|
|
eccentrically, closer to the superior border and deeper toward the posterior surface of |
|
the gland. |
|
If large, the duct may bulge from the anterior aspect of the gland or, if smaller, |
|
palpated or balloted as a “groove” along the long axis of the gland. |
|
To identify a small duct, we connect a 10-ml syringe to a 23-gauge butterfly needle |
|
aiming obliquely and posteriorly in the suspected direction of the duct; avoid the neck |
|
of the pancreas when searching/aspirating to minimize injury to the underlying SMV; |
|
aspiration of clear fluid is an indication the duct has been located. |
|
Measure duct pressure by connecting the needle to the manometer; in our experi- |
|
ence, average pancreatic ductal pressure in chronic pancreatitis patients is 33cmH2O |
|
(range: 20–47cmH2O), in contrast to a normal ductal pressure of ~10cmH2O. |
|
Leave the needle in the duct. |
|
The duct of Wirsung in the neck of the pancreas is usually eccentric and slightly |
|
superior and posterior (closer to the SMV/portal vein). |
A-1

868 |
SECTION 6 |
Pancreas |
|
|
|
STEP 5 |
Opening the pancreatic ductal system |
|
|
|
|
The anterior capsule of the pancreas is incised directly over the guide needle using electrocautery; a right-angle clamp is used to probe and define the direction of the duct.
The anterior aspect of the duct is opened to within 1.5cm of the tail of the gland; the duct is opened in the opposite direction toward the duodenal wall, along the duct of Wirsung, and extended to within 0.5–1cm of the ampulla of Vater (A-1).
The duct, after it crosses the portal vein, plunges posteriorly and then inferiorlaterally, coursing in the head close to the posterior capsule of the gland.
The duct to the uncinate process from the duct of Wirsung (mid-head) also runs close to the posterior capsule of the gland and is opened using a right angle clamp to define the direction of the duct (A-2).
Pancreatic calculi in side branches are searched for, and all encountered in any ductal systems are removed.
To assess ampullary patency and the adequacy of head resection, the surgeon places a probe (a 2–3mm Bakes dilator or the tip of the curved clamp) in the opened duct of Wirsung and pushes it against a finger indenting the duodenum.

Chronic Pancreatitis |
869 |
|
|
STEP 5 (continued) |
Opening the pancreatic ductal system |
|
The clamp should pass through the ampulla into the duodenum (A-3). |
|
|
|
The pancreatic head containing the ampullary portion of the pancreatic duct |
|
invaginates into the duodenum; looking down from above on the anterior surface of the |
|
gland, the pancreaticoduodenal junction is not a guide to locating the ampulla. |
|
The ampulla is 2–3cm more lateral and posterior due to invagination of the pancre- |
|
atic head into the duodenum. This consideration is important, because failure to the |
|
open main pancreatic duct down to the duodenum will leave a significant portion of the |
|
main pancreatic duct of Wirsung in the head of pancreas undrained along with its tribu- |
|
tary ducts; the thicker the head of pancreas, the longer the undrained portion of pancre- |
|
atic duct. This situation occurs when the anterior surface of the pancreatoduodenal |
|
junction is used as a guide to the position of the ampulla; unexcised small retention |
|
cysts associated with tributary ducts located deep within the fibrotic head of pancreas |
|
may be a source of persistent pain (A-4). |
A-3

870 |
SECTION 6 |
Pancreas |
|
|
|
STEP 6 |
Local resection of the head of the pancreas |
|
|
|
|
Working onward from the opened pancreatic duct, full-thickness slices of pancreatic tissue are excised to remove the anterior capsule of the gland and all intervening parenchyma down to the duct of Wirsung; thickness of the remaining shell of the head of the pancreas is carefully assessed after each slice to determine the amount of tissue that needs to be removed.
The posterior wall of the pancreatic duct of Wirsung in the head of pancreas marks the posterior extension of resection because it is within a few millimeters of the posterior capsule of the gland.
The duct of Santorini and its tributaries are located anteriorly in the pancreatic head; these ducts and tissue anteriorly are excised. In contrast, the duct to the uncinate process and its tributaries and the duct of Wirsung lie posterior; these systems should be unroofed but not excised as the posterior capsule of pancreas might be breached and the retroperitoneum exposed.
Careful palpation of the cored-out head of the pancreas helps identify retention cysts or impacted calculi in tributary ducts that should be removed.
Only a rim of pancreatic tissue should be left anteriorly along the inner aspect of the duodenal curve and a margin of 5–10mm of pancreatic tissue to the right of the SMV to avoid vascular injury; care should be taken to preserve the pancreatoduodenal arcade.
Based on the weight of excised tissue, approximately 4–12g of fibrotic tissue should be removed. This is an underestimate of the total tissue removed; additional tissue is vaporized when taking multiple slices.
Should there be concern about possible malignancy, tissue should be submitted for frozen section, histopathologic examination; if positive, pancreatoduodenectomy should be performed.

Chronic Pancreatitis |
871 |
|
|
STEP 7 |
Managing and avoiding injury to the common bile duct (CBD) – avoiding injury |
|
About 50% of patients with chronic pancreatitis have radiographic evidence of |
|
|
|
anatomic tortuosity, kinking, and narrowing of CBD; with significant stricturing, 10% |
|
of patients undergoing head resection have preoperative findings of CBD obstruction – |
|
biochemical or clinical jaundice. |
|
During the coring out process, it is important to identify and free the intrapancreatic |
|
portion of the CBD from the inflamed, fibrotic periductal tissue. |
|
The position of the CBD in the posterior pancreas is variable and either may be |
|
posterior to the pancreas, indenting the pancreas (on palpation a “groove” may be |
|
discerned), or traversing the pancreatic parenchyma; the latter site is most commonly |
|
associated with stricturing. |
|
In patients with anatomic obstruction, a 3-mm Bakes dilator or biliary Fogarty® |
|
catheter is passed into the CBD to guide and protect the CBD during pancreatic |
|
resection. |
|
If the CBD is injured or strictured or the obstruction is unable to be relieved, |
|
a choledochojejunostomy is an option. |
|
An alternative method for coring out the head of the pancreas is excavation of the |
|
head with total resection of the main and secondary ducts. The ductal system is followed |
|
to the level of the ampulla or to where the pancreatic duct meets the intrapancreatic |
|
CBD; the pancreatic duct is divided; the proximal duct margin is sewn closed with a |
|
4-0 nylon suture. Use of the Cavitron R Ultrasonic Aspirator (CUSA), System 200 |
|
(Valleylab, Norwalk, CT), facilitates conical removal of parenchyma in conjunction |
|
with electrocautery; the high-energy hand-piece at a setting of 70–80% power permits |
|
clear visualization of tissue, ducts, and vessels in the head of pancreas. The proximal |
|
pancreatic duct is removed in total by transecting the dorsal duct at the pancreatic neck. |
