
clavien_atlas_of_upper_gastrointestinal_and_hepato-pancreato-biliary_surgery2007-10-01_3540200045_springer
.pdf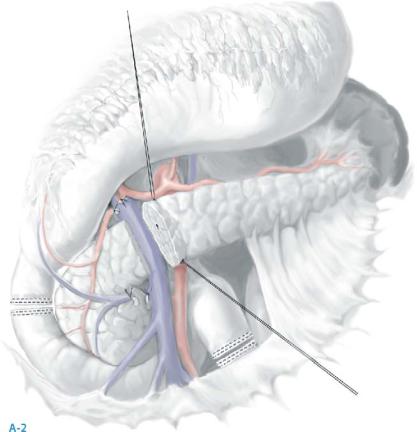
852 |
SECTION 6 |
Pancreas |
|
|
|
STEP 1 (continued) |
Incision and mobilization, duodenum, pylorus, antrum (A-1, A-2) |
|
|
|
|
After placing stay-sutures along the superior and inferior edges of the neck of the pancreas, a plane is developed carefully behind the neck of the pancreas, but anterior to the superiormesenteric portal venous confluence. The neck of the pancreas is then divided carefully. In score patients with severe chronic inflammation, this maneuver may be very difficult.

Chronic Pancreatitis |
853 |
|
|
STEP 2 |
Excision of pancreatic head, remaining duodenum, and distal common bile duct |
|
This resection is no different than resection for cancer except that nodal tissue along |
|
|
|
the right side of the superior mesenteric artery is not necessarily removed with the |
|
specimen. The uncinate process can be clamped on its surface to separate it from the |
|
SMV and the first jejunal vein that enters this area. To decrease blood loss, the surgeon |
|
on the left side of the patient compresses the pancreatic head and uncinate process |
|
between the fingers of the left hand to control vessels in lymphatic attachments to |
|
the superior mesenteric artery behind the portal vein. |
|
Electrocautery is avoided when dividing the main pancreatic duct over the portal |
|
vein; cautery or harmonic scalpel (Ethicon Endosurgery, Cincinnati, OH) is useful in |
|
dividing the parenchyma. |


Chronic Pancreatitis |
855 |
|
|
STEP 4 |
Reconstruction – pancreatic anastomosis |
|
Pancreatic and biliary anastomoses are retrocolic; the duodenojejunostomy is antecolic; |
|
|
|
anastomoses are positioned to isolate potential leakage of bile and pancreatic anasto- |
|
moses from the duodenojejunostomy to minimize delayed gastric emptying (8% in my |
|
last 215 resections). |
|
The stump of the proximal jejunum is delivered into the supracolic space through |
|
a retrocolic defect in the mesocolon; the stomach with the preserved pylorus and |
|
duodenal bulb is brought antecolic over the left transverse colon, allowing for an |
|
anatomically remote duodenojejunostomy. |
|
Patients with a normal 2- to 3-mm duct in the pancreatic remnant are more prone |
|
to anastomotic leak at the pancreaticojejunostomy. |


Chronic Pancreatitis |
857 |
|
|
STEP 6 |
Biliary anastomosis |
|
A single layer, end choledocho-to-side jejunal anastomosis is performed with inter- |
|
|
|
rupted 5-0 polydioxone with knots tied on the outside (to prevent stone formation |
|
on knots of delayed absorbable suture); no tube choledochostomy is needed. |
|
The jejunal limb is tacked to the exit site through the transverse mesocolon with |
|
3/0 silk sutures. |

858 |
SECTION 6 |
Pancreas |
|
|
|
STEP 7 |
Antecolic duodenojejunostomy |
|
|
|
|
The intact stomach, first part of the duodenum, and omentum are brought over the left side of the transverse colon. The jejunal limb (after it exits the transverse mesocolon downstream from the biliary and pancreatic anastomoses) is brought up to the end of the stapled duodenum, and an end duodenal-to-side jejunal anastomosis is performed in two layers 10cm distal to the exit site of the jejunum from the transverse mesocolon. An inner layer of running 3-0 polyglycolic acid and an outer layer of interrupted 3-0 silk are put in place.
A 15-Fr. drainage catheter is placed under the biliary and pancreatic anastomoses from the right upper quadrant.
The midline fascia is closed with an interrupted figure-of-eight 0 polyglyconate suture.
Chronic Pancreatitis |
859 |
|
|
Postoperative Care
■The NG tube is removed 1–3days postoperatively.
■Drains are removed when drainage volume is <30–50ml/day with low amylase activity.
■Oral intake is allowed when tolerated.
■Early:
–Intra-abdominal hemorrhage– examine specifically ligatures of named arteries for pseudoaneurysms and pancreatic remnant
–GI hemorrhage – either from pancreaticojejunostomy or duodenojejunostomy
–Delayed gastric emptying
–Anastomotic leak – most likely at pancreaticojejunostomy but possible at choledochojejunostomy and duodenojejunostomy
–Intra-abdominal abscess, usually related to transient or persistent anastomotic leak
–Wound infection
–Intestinal obstruction – exclude internal hernia
■Late:
–Recurrent epigastric pain
–Extrahepatic jaundice secondary to stricture at choledochojejunostomy
–Pancreatic insufficiency either from progression of disease (chronic pancreatitis) or stricture at pancreaticojejunostomy
–Adhesive intestinal obstruction
–Stomal or duodenal ulcer at or near duodenojejunostomy
–Pancreatic adenocarcinoma, estimated as high as up to 1% risk per year

860 |
SECTION 6 |
Pancreas |
|
|
|
|
Tricks of the Senior Surgeon |
|
■The key to pain relief for chronic pancreatitis is pancreatic resection performed when the strict anatomic selection criteria described in this section are met.
■Excess blood loss results in increased morbidity. To accomplish this, all named vessels are triply ligated with non-absorbable suture. The ultrasonic scissors are utilized for dividing small veins and particularly those around the right gastroepiploic and supraduodenal vessels. This technique is also handy when separating the mesenteric vascular attachments to the proximal jejunum removed with the specimen in the area of the ligament of Treitz.
■The left hand of the surgeon standing on the left side of the patient can minimize blood loss during division of the attachments of the vascular lymphatics from the dorsal head of the pancreas to the area around the superior mesenteric artery.
Pedicles of tissue are divided as the dissection proceeds along the superior mesenteric artery. Only one clamp is used for each pedicle on the patient side of the divided pedicle; the specimen side is not clamped and is compressed by the left hand.
■Preserve all of the greater omentum as this “watchdog” of the abdomen decreases postoperative infection.
■Use intraoperative fluoroscopic pancreatography to ensure that the pancreatic remnant is adequately drained. I use a cholangiocatheter with a balloon tip.
■When a small pancreatic duct is used for the pancreaticojejunostomy, the anastomosis is best done with magnification to avoid crossing the sutures. The duct-to- mucosa anastomoses can be done in a more exact fashion by seeing the needle pass in and out of a small pancreatic duct. I find the surgical microscope at 12.5 power useful to minimize pancreaticojejunostomy leak.
■The choledochojejunostomy should have all of the absorbable knots tied on the outside, and no absorbable suture should be exposed to bile flow.
■I use a single closed suction drain made of silicone rubber.
■An antecolic duodenojejunostomy has a marked decrease in delayed gastric emptying compared to the retrocolic method.

Chronic Pancreatitis |
861 |
|
|
Non-Anatomic Resections:
The Frey and Beger Procedures
Charles F. Frey, Kathrin Mayer, Hans G. Beger, Bettina Rau, Wolfgang Schlosser
Introduction
Local (non-anatomic) resections of the head of the pancreas with longitudinal pancreaticojejunostomy (LR-LPY or Frey procedure) and the duodenum-preserving (anatomic) subtotal head resection (Beger procedure) share similar goals, i.e., relief of pain and management of local pancreatic complications (biliary, duodenal, or venous obstruction, provision of pancreatic ductal drainage, subtotal resection of inflammatory mass in head of pancreas). The rationale for this approach is that the pain of chronic pancreatitis is believed to arise from either a ductal or pancreatic parenchymal hypertensive “compartment” syndrome and/or from inflammatory neural “irritation”. The head of the pancreas is thought to be the driver or “pacemaker” of the pain. Pancreatic subtotal resections can accomplish removal of the “pain pacemaker” region of the gland with a lesser operative morbidity as well as preserve gastroduodenal continuity.
Indications and Contraindications
Indications |
■ |
Incapacitating abdominal pain, usually of a continuous nature, and in selected |
|
|
patients also when intermittent and frequent or associated with recurrent attacks |
|
|
of acute pancreatitis |
|
■ |
Resolution of pancreatic and extrapancreatic structural complications associated |
|
|
with chronic pancreatitis |
|
|
– Extrapancreatic – common bile duct obstruction, duodenal obstruction, selected |
|
|
patients with compression of portal and/or superior mesenteric veins |
|
|
– Pancreatic |
|
|
– Parenchymal: scarring, multiple fibrous strictures of duct (“chain of lakes”) |
|
|
with calcification, ductal hypertension, retention cysts, ductal stones |
|
|
– Ductal disruptions: contained – pseudocyst; uncontained – ascites; fistula – |
|
|
pleural or pericardial |
|
■ |
Inadequate pain relief after ductal drainage procedure or distal pancreatectomy |
|
■ |
Pancreas divisum causing chronic pancreatitis |
