
clavien_atlas_of_upper_gastrointestinal_and_hepato-pancreato-biliary_surgery2007-10-01_3540200045_springer
.pdf
Resection for Neoplasms of the Pancreas |
781 |
|
|
Central Resection
Sergio Pedrazzoli, Claudio Pasquali, Cosimo Sperti
Introduction
In 1959, Letton and Wilson reported the first non-resective treatment of traumatic rupture of the neck of the pancreas. The right stump of the pancreatic head was oversewn, and a Roux-en-Y loop of jejunum was anastomosed to the left body/tail of the pancreas. In 1984, Dagradi and Serio reported the first central pancreatectomy for an insulinoma, and in 1988, Fagniez, Kracht, and Rotman reported two central pancreatectomies performed for an insulinoma and a serous cystadenoma. At least 150 central pancreatectomies have been reported so far without mortality. Central pancreatectomy involves anatomic removal of benign or borderline lesions of the neck and/or proximal body of the pancreas together with 1cm of normal tissue on both sides. The goal is to preserve at least 5cm of the normal pancreatic tissue of the body/tail of the pancreas that would otherwise be removed with a complete left pancreatectomy.
Indications and Contraindications
Indications |
■ |
Small, centrally located lesions (<5cm in diameter) not amenable to enucleation |
|
■ |
Traumatic transection of the neck of the pancreas |
|
■ |
Benign, borderline, or low grade malignant lesions (selected neuroendocrine |
|
|
neoplasms, serous or mucinous cysticneoplasms, solid pseudopapillary neoplasms, |
|
|
branch type intraductal papillary mucinous neoplasms, solitary true cysts, parasitic |
|
|
cysts, etc.) |
|
■ |
Maintenance of a distal pancreatic stump of at least 5cm in length |
|
|
Malignant pancreatic lesions |
Contraindications |
■ |
|
|
■ |
Involvement of the pancreas by contiguous malignant neoplasms |
|
■ |
Insulin-dependent diabetes |
|
|
Advanced age (>70years) |
Relative Contraindications |
■ |
|
|
■ |
High-risk patient |
|
■ |
Non-insulin-dependent diabetes (NIDD) |
782 |
SECTION 6 |
Pancreas |
|
|
|
|
Preoperative Investigations and Preparation for the Procedure |
|
|
History: |
Endocrine syndrome (hypoglycemia, acute pancreatitis, |
|
|
upper abdominal pain) |
|
Clinical evaluation: |
Exclude diarrhea secondary to exocrine insufficiency, |
|
|
diabetes, and signs of portal hypertension |
|
Laboratory tests: |
Amylase, lipase, and/or peptide hormones (insulin, gastrin, |
|
|
glucagon, vasoactive intestinal polypeptide, pancreatic |
|
|
polypeptide, somatostatin, chromogranin A), tumor markers |
|
|
(CA 19–9, CEA, MCA, etc.). If an endocrine neoplasm is |
|
|
suspected, store a preoperative sample of serum and/or |
|
|
plasma for specific assays based on histologic and immuno- |
|
|
histochemical characterization of the resected lesion |
|
Imaging: |
Differential diagnosis and assessment of resectability based |
|
|
on ultrasonography, computed tomography, magnetic reso- |
nance imaging, or endoscopic ultrasonography
– 111In-pentetreotide scintigraphy (OctreoScan): endocrine neoplasms
– Positron emission tomography (PET): differentiates between benign and malignant lesions
Preoperative preparation: – Somatostatin analogues: no specific study on central pancreatectomy
– Perioperative antibiotics: as for any clean-contaminated operation
Resection for Neoplasms of the Pancreas |
783 |
|
|
|
|
|
Procedure: Central Pancreatectomy |
|
|
|
|
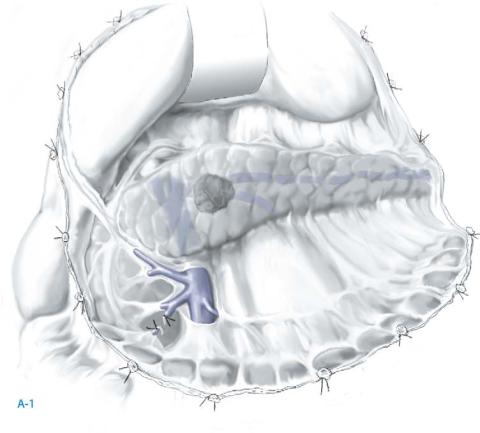
STEP 1 |
Exposure of central part of pancreas |
|
|
Optimal access is via a midline incision |
|
|
|
|
The pancreas is exposed by detaching the greater omentum from the transverse colon and freeing the superior aspect of the middle colic vessels until the anterior aspect of the pancreas is exposed completely; stomach is retracted rostrally.
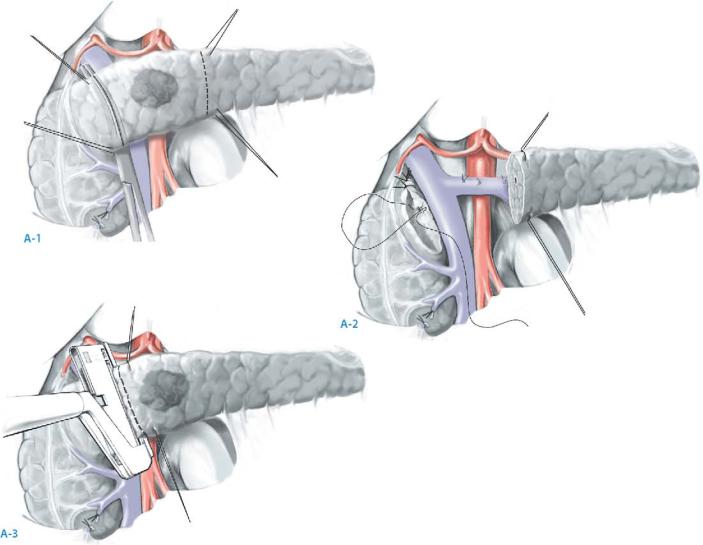
The superior mesenteric vein is identified, and its anterior surface cleared below the neck of the pancreas; care must be taken not to injure venous tributaries; occasionally a middle colic branch of the superior mesenteric vein requires division, especially if it joins in a V-shaped way with the right gastroepiploic vein. Gastroepiploic vessels are preserved, unless the lesion reaches the right border of the superior mesenteric-portal vein (A-1).
784 |
SECTION 6 |
Pancreas |
|
|
|
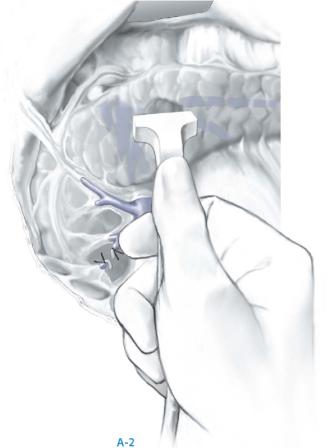
STEP 1 (continued) |
Exposure of central part of pancreas |
|
|
|
|
Evaluate the extent of the lesion by intraoperative ultrasonography (IOUS); this technique is particularly useful for small, deeply located lesions. Mark with electrocautery the exact extent of the planned central pancreatectomy including 1cm of normal pancreatic tissue on both sides (A-2).
Resection for Neoplasms of the Pancreas |
785 |
|
|
|
|
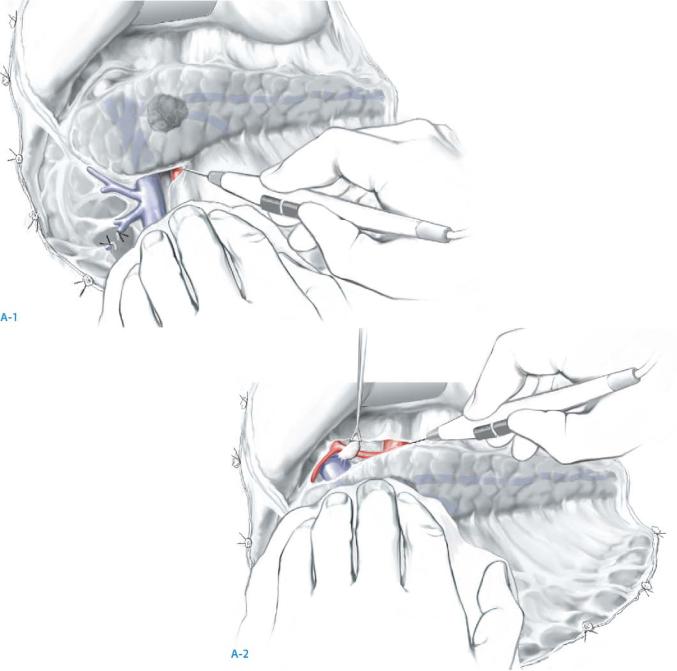
STEP 2 |
Mobilizing pancreas to be resected |
|
|
The posterior peritoneum is incised with electrocautery along the inferior border of the |
|
|
||
|
part of the pancreas to be removed until the splenic vein is visualized. Attention should |
|
|
be paid to ligate and divide an often present, small artery and vein that lies between the |
|
|
left side of the superior mesenteric vein and the inferior border of the pancreas (A-1). |
|
|
Lymph node(s) anterior to the common hepatic artery are removed, and the common |
|
|
hepatic artery is detached from the superior border of the pancreas extending from the |
|
|
celiac axis to the gastroduodenal artery. |
|
|
The hepatic artery is retracted rostrally |
(A-2). |
|
When the tumor extends to the left of the origin of splenic artery, the splenic artery |
|
|
should first be mobilized and retracted rostrally, taking care to divide the dorsal artery. |
|
786 |
SECTION 6 |
Pancreas |
|
|
|
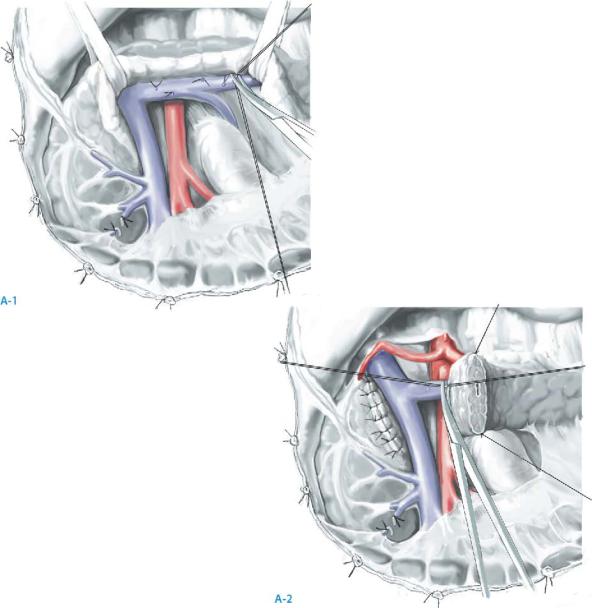
STEP 3 |
Mobilization of superior mesenteric and splenic vein |
|
|
The plane between the superior mesenteric/portal vein and the neck of pancreas is |
|
|
||
|
gently teased apart; usually no veins transgress this space. In the rare event of a pancre- |
|
|
atic vein joining the anterior surface of the portal vein, the pancreas can be transected |
|
|
progressively from below, until the vein is exposed allowing division of the vein between |
|
|
ties. |
|
|
The pancreas is encircled with a tape and retracted anterorostrally, allowing visuali- |
|
|
zation and ligation of the veins from the posterior pancreas (to be resected) entering the |
|
|
splenic vein |
(A-1). |
|
The splenic vein is then separated carefully from the pancreas to be resected. |
|
|
Transection of the proximal pancreas (right side) begins 1cm proximal to the lesion; |
|
|
anterior retraction of the left pancreas may allow better visualization and ligation of the |
|
|
veins from the posterior pancreas to the splenic vein (A-2). |
|
Resection for Neoplasms of the Pancreas |
787 |
|
|
|
|
STEP 4 |
Removal of central pancreas |
|
|
|
|
Transection of pancreas: Stay sutures are placed on the superior and inferior pancreatic margins just to the right and left of the proximal and distal lines of division to occlude the superior and inferior pancreatic vessels running transversely in the parenchyma.
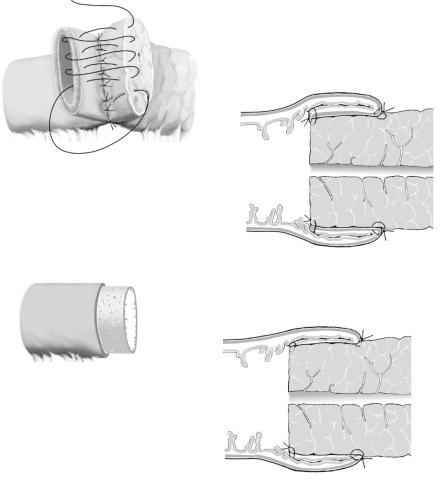
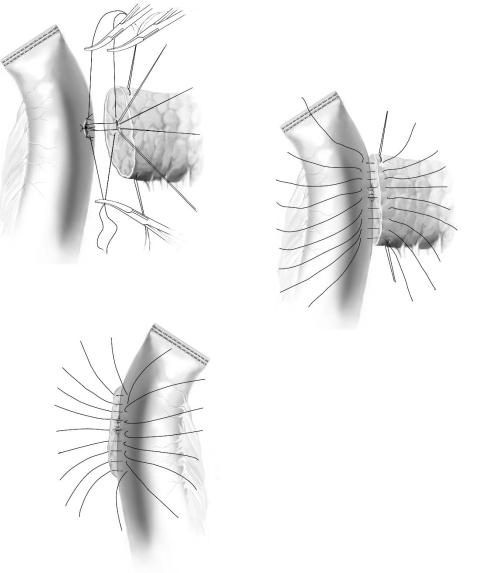
The pancreas is divided by scalpel using a V-shaped incision on the right side of the tumor to facilitate closure in a fish-mouth fashion; the pancreas is transected 1cm to the left of the tumor with suture ligation of the larger arterial bleeders in the cut edge (A-1). The pancreatic duct in the right side of the remnant gland is suture-ligated with 5-0 non-absorbable monofilament, and the pancreatic tissue closed in a fish-mouth fashion
with interrupted 3-0 synthetic absorbable sutures (A-2).
A very thin neck of pancreas can also be closed with a stapler and bleeding from small arteries controlled with absorbable synthetic stitches; the pancreatic duct is still identified and suture-ligated individually with 5-0 non-absorbable monofilament (A-3). The right-sided limit of a central pancreatectomy is the left side of the gastroduo-
denal artery; transecting the pancreas to the right of the gastroduodenal artery can injure the common bile duct.
The specimen is sent to the pathologist for frozen section examination and for checking the right and left resection margins. A stitch on one margin will orient the specimen for the pathologist.
790 |
SECTION 6 |
Pancreas |
|
|
|
|
|
|
Postoperative Care and Tests |
|
|
|
■ |
Postoperative surveillance in an intensive care unit |
|
|
■ |
Serum amylase and/or lipase activity |
|
|
■ |
Check for amylase and lipase activity in drain fluids |
|
Local Postoperative Complications
■Short term:
–Anastomotic disruption
–Pancreatic fistula
–Peripancreatic abscess
–Intra-abdominal bleeding
–Acute pancreatitis
–Subdiaphragmatic abscess
–Splenic-portal vein thrombosis
–Pleural effusion
■Long term:
–Pancreatic pseudocyst
–Pancreatic ascites
–Pancreatitis
–Diabetes
Tricks of the Senior Surgeon
■If the approach to the superior mesenteric portal trunk is difficult, Kocherization of the head of the pancreas is advisable; control of bleeding will be easier.
■If the superior mesenteric/portal trunk or one of its branches is injured, do not panic and use instruments blindly! Compress the venous trunk between the fingers inserted posteriorly (after the Kocher maneuver) behind the head of the pancreas and the thumb on the anterior aspect of the pancreas; suture the tear with 5-0 polypropylene.
■If the pancreas is too large for an invagination/dunking pancreatojejunostomy, choose either a duct-to-mucosal anastomosis or a pancreaticogastrostomy. Closure of the left pancreatic stump is followed by gland fibrosis that compromises endocrine secretion, nullifying the long term benefits of the central resection.
