clavien_atlas_of_upper_gastrointestinal_and_hepato-pancreato-biliary_surgery2007-10-01_3540200045_springer
.pdf750 |
SECTION 6 |
Pancreas |
|
|
|
|
Postoperative Tests |
|
Thoracoscopic Splanchnicectomy
■Surveillance in an intermediate care unit with oxygen saturation monitoring
■Routine chest radiograph to exclude residual pneumothorax
Local Postoperative Complications
Intraoperative Splanchnicectomy
■Short term:
–Intra-arterial injection of neurolytic agent – this can be prevented by aspirating the syringe containing the neurolytic agent before injecting
–Retroperitoneal bleeding – unusual, minimized by applying topical pressure after instillation of neurolytic agent
–Transient orthostatic hypotension – unusual, lasts only 1–2days
–Very rare, anecdotal case reports of paraplegia secondary to intrathecal injection of neurolytic agent – this is preventable with careful technique
■Long term:
–Recurrent pain
Thoracoscopic Splanchnicectomy
■Short term:
–Pulmonary: pneumothorax, hemothorax, and hemo-pneumothorax – treat by closed intercostal chest drainage. Less common is chylothorax, requiring ligation of the thoracic duct.
–Transient ileus – managed conservatively.
–Inadvertent injury or transection of sympathetic chain may predispose to retrograde ejaculation.
■Long term:
–Recurrence of pain
Denervation: Pain Management |
751 |
|
|
Tricks of the Senior Surgeon
Intraoperative splanchnicectomy:
■Use a 20-gauge spinal needle (longer than a regular needle).
■Use of a smaller volume syringe allows the surgeon to hold the needle/syringe in one hand.
■Do not disrupt the peritoneum overlying the retroperitoneum in the region of the celiac plexus.
■Two minutes of topical pressure will prevent hematomas.
Thoracoscopic splanchnicectomy:
■Meticulous positioning of the ports aids visibility of the entire sympathetic chain.
■Total collapse of the lung is unnecessary; an 8-cm water pressure pneumothorax is also usually adequate to identify the splanchnic nerves.
■The proximal contribution to the GSN is identified by tracing the sympathetic chain distally as it courses over the necks of the proximal ribs.
■Gentle traction on the sympathetic chain brings the splanchnic branches into profile.
■Troublesome bleeding from an intercostal vein can be controlled with pressure, cautery, or clip.
■Accurate placement of ports in the intercostal spaces avoids postoperative intercostal neuralgia.
Enteric Ductal Drainage for Chronic Pancreatitis
William H. Nealon
Introduction
The concept of draining an apparently obstructed main pancreatic duct was first addressed by opening either the proximal end of the pancreatic duct at the ampulla by doing a sphincterotomy or at the distal end of the pancreatic duct by removing the tail (Duval procedure). Puestow is credited with the concept of a longitudinal incision along the main pancreatic duct through the body and the head of the pancreas. This procedure was first described as a modification of a Duval procedure and therefore included resection of the pancreatic tail. Partington and Rochelle determined that a tail resection was unnecessary and carried out only a side-to-side lateral pancreaticojejunostomy. The principle of the procedure is to decompress an apparently obstructed main pancreatic duct (and maybe to also decompress the pancreatic parenchyma – the pancreatic compartment syndrome suggested by Reber). This assumption is based on the fact that the pancreatic duct is markedly dilated, suggesting a restriction to flow.
Indications and Contraindications
Indications |
■ |
Chronic persistent pain |
|
■ |
To prevent episodes of acute exacerbations in chronic pancreatitis |
|
■ |
To facilitate resolution of symptomatic pancreatic pseudocyst |
|
■ |
To prevent further loss of pancreatic exocrine and endocrine function |
|
|
“Small duct” (<5mm) chronic pancreatitis |
Contraindications |
■ |
|
|
■ |
Extrahepatic venous obstruction, because of the risk of hemorrhage |
|
■ |
Suspicion of malignancy |
|
■ |
Advanced cirrhosis |
754 |
SECTION 6 |
Pancreas |
|
|
|
|
Preoperative Investigations and Preparation for Procedure |
|
|
History: |
History of chronic, unremitting epigastric abdominal pain |
|
|
or acute exacerbations of typical pancreatic pain, history |
|
|
of ethanol abuse or other possible causes of chronic pancre- |
|
|
atitis |
|
Clinical evaluation: |
Establish presence or absence of narcotic usage and require- |
|
|
ment (if narcotic addicted, entertain the concept of postopera- |
|
|
tive detoxification), frequency of hospitalizations, nutritional |
|
|
status, pancreatic functional status (endocrine and exocrine), |
|
|
ASA risk status |
|
Laboratory tests: |
Serum amylase and/or lipase, albumin, alkaline phosphatase, |
|
|
GGT, bilirubin coagulation parameters, CA 19–9, glucose |
|
Imaging: |
CT or MRI/ MRCP, ERCP if indicated |
|
Preparation for surgery: |
Maximize endocrine status (insulin), maximize exocrine |
status (enzyme replacement), bowel preparation if necessary, perioperative prophylactic antibiotics

Enteric Ductal Drainage for Chronic Pancreatitis |
755 |
|
|
|
Procedure: Lateral Pancreaticojejunostomy |
|
(Modified Puestow Procedure) |
|
|
STEP 1 |
Exposure and exploration are facilitated by insertion of a retractor (Thompson) |
|
First, the lesser sac is entered by separating the attachments between the gastrocolic |
|
|
|
omentum and the transverse colon. |
|
Any “congenital” or acquired adhesions between the posterior surface of the stomach |
|
and the anterior surface of the pancreas are transected widely, exposing the anterior |
|
surface of the pancreas, including the head of the pancreas – take care to identify and |
|
exclude the right gastroepiploic artery and vein, which are situated between the head |
|
of the pancreas and the pylorus. |

756 |
SECTION 6 |
Pancreas |
|
|
|
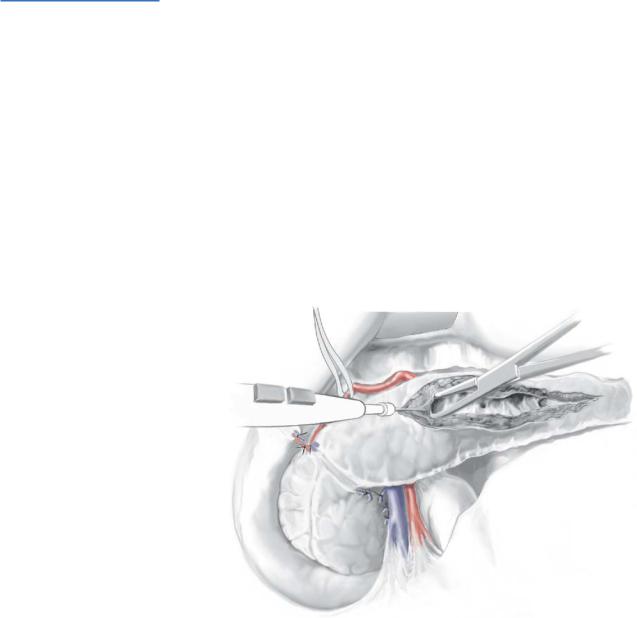
STEP 2 |
Mobilize the inferior border of the body of the pancreas |
|
|
|
|
Identify and avoid the inferior mesenteric vein to the left of the spine.
Extend the dissection from the body toward the head of the pancreas. This facilitates bimanual examination and palpation of the anterior surface of the gland.
Place a broad curved retractor beneath the posterior wall of the stomach and retract superiorly.
Palpate and determine the location of the main pancreatic duct.
Enteric Ductal Drainage for Chronic Pancreatitis |
757 |
|
|
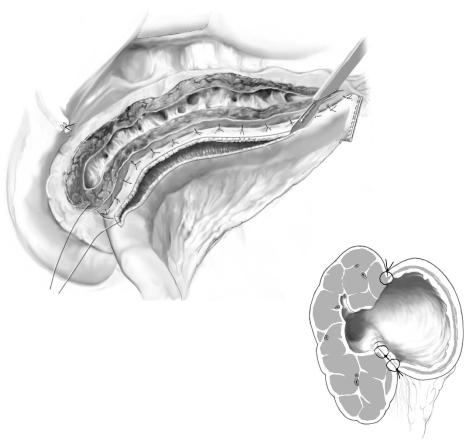
STEP 3
The pancreas should be easily appreciated because of its hard, fibrotic texture.
The dilated main pancreatic duct feels a bit like a large vein on the arm with a ballotable texture and a definite “trough.”
The superior and inferior borders of this softer area feel like a canyon or a cliff and this represents the fibrotic pancreas on both sides.
Once the palpation is conclusive, a 22-gauge needle is passed through the anterior surface of the pancreas and into the pancreatic duct; on removing the needle, you should see clear fluid return, confirming that the main pancreatic duct has been accessed. The purpose of this maneuver is to avoid incising into the splenic vein or another structure mistaken for the main pancreatic duct.
Once pancreatic juice is determined, then electrocautery is utilized to incise the anterior surface of the body of the pancreas into the pancreatic duct parallel and adjacent to the needle, which is left in the pancreatic duct as a guide.
758 |
SECTION 6 |
Pancreas |
|
|
|
STEP 4
A right angle clamp will facilitate using the electric cautery to open widely the duct out to the tail of the pancreas laterally and toward the head of the pancreas. As you reach the genu of the main pancreatic duct it is important to extend the incision through the genu and toward the ampulla. This maneuver requires not only turning the incision inferiorly but also considerably increasing the depth of incision through the parenchyma of the pancreas in the head of the gland because the duct goes more posteriorly. This area also has a rich blood supply, and some amount of hemorrhage may be encountered during this incision. Success rates are thought to depend on in great part on an adequate drainage into the head of the pancreas in this manner. There appears to be less significance to the extent of drainage into the tail of the pancreas except in patients who have more localized disease in the tail of the pancreas.
Once adequate space is established, a Seurat clamp may be utilized. All stones encountered should be removed from the duct; any secondary ductular stones should also be removed.
Enteric Ductal Drainage for Chronic Pancreatitis |
759 |
|
|
|
|
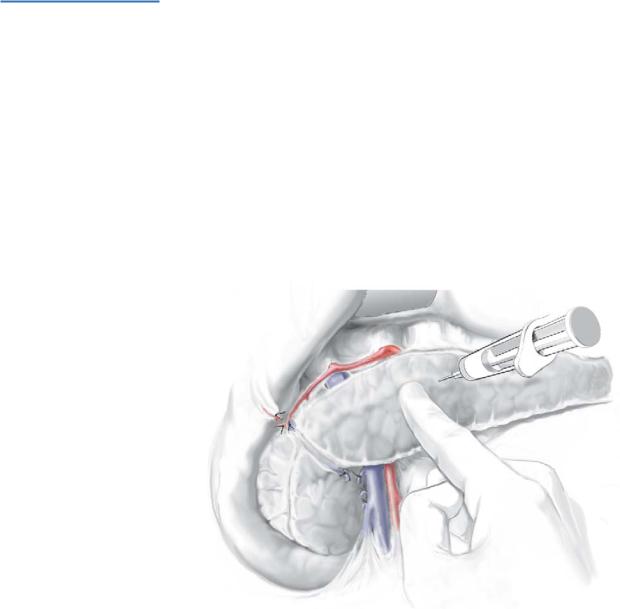
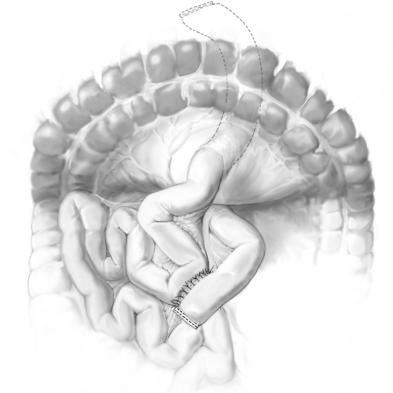
STEP 5 |
Roux-en-Y jejunal preparation |
|
|
|
|
An area is chosen approximately 15cm distal to the ligament of Treitz in a position which will facilitate easy performance of the jejunojejunostomy. The mesenteric attachments are divided between clamps to mobilize the Roux limb. A GIA stapling device is utilized to divide the jejunum at this site.
The avascular area is then chosen in the left transverse mesocolon. A window is created through which the distal divided end of jejunum may be brought. It is important to avoid undue tension at the mesentery; at times, it is necessary to divide the truncal branches of the jejunal mesenteric vessels below the arcade to permit a flexible limb. The divided end of jejunum is aligned toward the head of the pancreas, and a side- to-side approach is established.