
clavien_atlas_of_upper_gastrointestinal_and_hepato-pancreato-biliary_surgery2007-10-01_3540200045_springer
.pdf730 |
SECTION 6 |
Pancreas |
|
|
|
|
Preoperative Investigations and Preparation for the Procedure |
|
|
History: |
Vague abdominal or back pain after an attack of acute |
|
|
pancreatitis, nausea, vomiting, and weight loss |
|
Clinical: |
Fullness or mass in the epigastrium |
|
Laboratory tests: |
Persistent increase in serum amylase after attack of acute |
|
|
pancreatitis |
|
Diagnostic imaging: |
CT can identify one or more pseudocysts in the pancreas and |
|
|
may help to differentiate a cystic neoplasm from a pseudocyst |
|
ERCP |
Rarely used but can differentiate a pseudocyst that communi- |
|
|
cates with the main pancreatic duct from a cystic neoplasm, |
|
|
which should not occur unless it is an IPMN (intraductal |
|
|
papillary mucinous neoplasm) |
|
Preoperative preparation: NPO two to four hours before operation. A perioperative |
|
|
|
prophylactic I.V. antibiotic is repeated depending on the |
|
|
duration of operation |

Drainage of Pancreatic Pseudocysts |
731 |
|
|
Procedures
|
Open Cystogastrostomy |
|
|
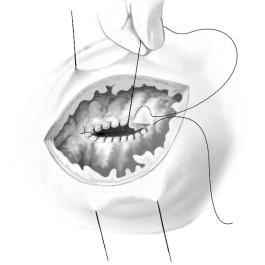
STEP 1 |
Exposure of pseudocyst |
|
A bilateral subcostal incision is preferred; alternatively, a midline incision may be used. |
|
|
|
After routine abdominal exploration, a mechanical ring retractor is placed to retract |
|
the liver and abdominal wall. |
|
The pseudocyst adherent to the posterior gastric wall is visualized or palpated |
|
transgastrically. |
|
Seromuscular stay sutures are placed in the anterior gastric wall over the cyst. |
|
A long gastrotomy is made, and the anterior gastric wall is retracted using stay |
|
sutures. |

Drainage of Pancreatic Pseudocysts |
733 |
|
|
|
|
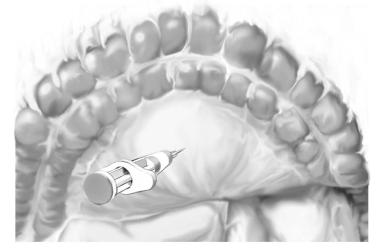
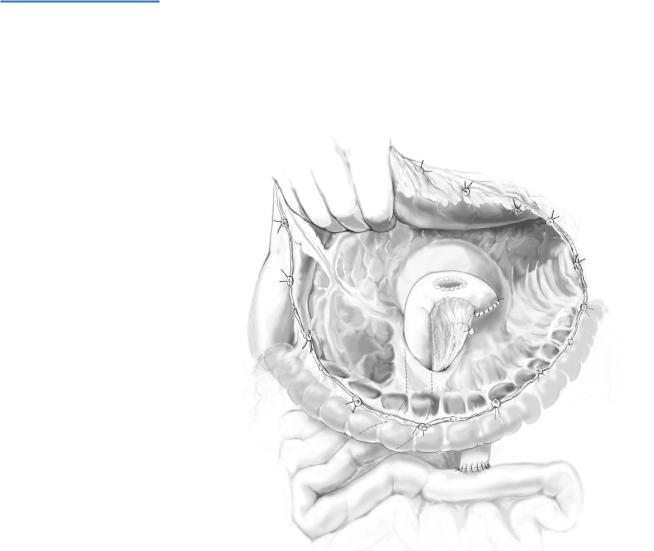
STEP 3 |
Oversewing of cystogastrostomy |
|
|
|
The posterior common cyst/gastric wall is oversewn (“reefed”) with running 3-0 silk |
|
|
|
|
|
suture. One suture is run from 3o’clock to 9o’clock and tied, the other suture is run from |
|
|
9o’clock to 3o’clock; this avoids a “pursestring” effect on the opening and allows the cyst |
|
|
to communicate freely with the stomach. |
|
|
The gastrotomy is closed in two layers; the inner, running 3-0 polyglyconate suture is |
|
|
placed in a Connell fashion to invert the mucosa and obtain hemostasis; the outer layer |
|
|
consists of interrupted 3-0 silk seromuscular sutures. |
|
|
The abdomen is closed without drainage using running 1-0 polydioxanon for the |
|
|
anterior and posterior rectus fasciae for a subcostal incision and 1-0 polyglycolic acid |
|
|
for a midline incision. |
|
|
The skin incision is closed with staples. |

734 SECTION 6 Pancreas
Open Cystoduodenostomy
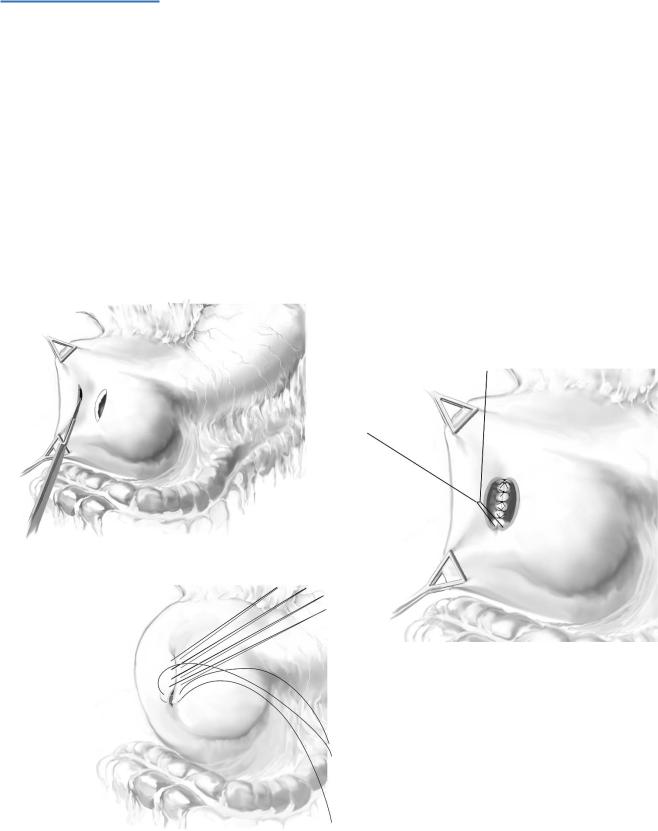
STEP 1
Specific indications include a pseudocyst in the head of the pancreas anatomically placed so that only a cystoduodenostomy is possible.
The same approach/setup as for cystogastrostomy above. The pseudocyst is visualized and palpated.
The cyst is aspirated with a 22-gauge needle.
A clear, opalescent, or brownish fluid should be obtained; mucoid fluid suggests a cystic neoplasm.
The syringe is removed from the needle, and a #11 blade knife is used to enter the cyst along the needle.
A right-angled clamp is inserted to elevate the cyst wall, for enlarging the opening to at least 2–3cm of longer; a biopsy is taken of the cyst wall.
736 |
SECTION 6 |
Pancreas |
|
|
|
|
Open Cystojejunostomy |
|
|
|
|
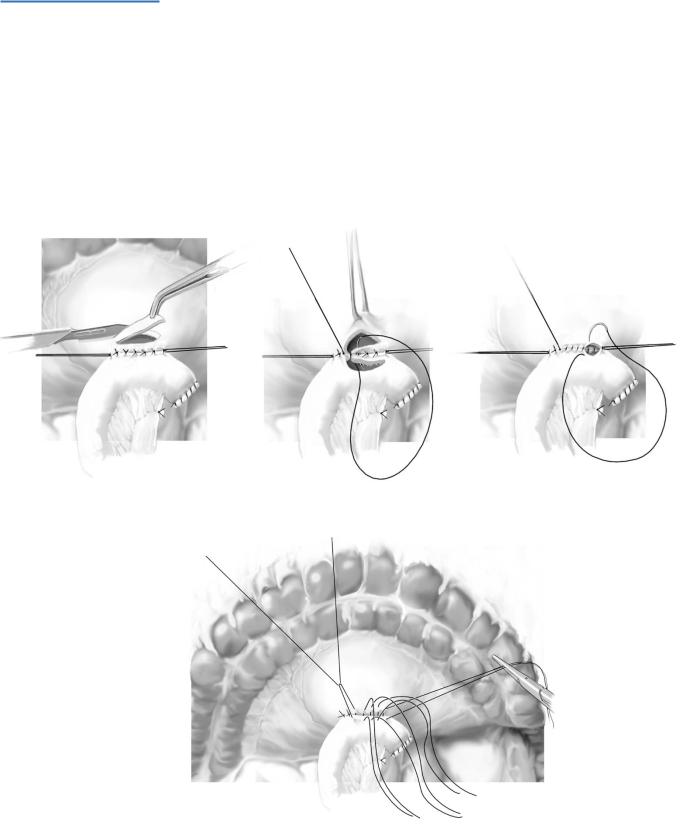
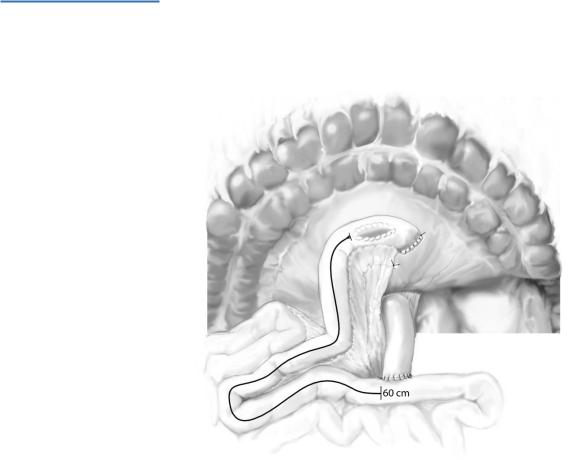
STEP 1 |
Exposure of pseudocyst |
|
|
Specific indications include a pseudocyst not adhering to the posterior gastric wall |
|
|
||
|
in any location in the pancreas – head, body, or tail and those pseudocysts that bulge |
|
|
through the transverse mesocolon. |
|
We prefer a bilateral subcostal incision with a mechanical ring retractor.
The pseudocyst is intimate with the transverse mesocolon.
Aspirate the cyst with a 22-gauge needle.
738 |
SECTION 6 |
Pancreas |
|
|
|
STEP 3
The proximal jejunum is anastomosed to the Roux limb 60cm distally.
Drainage of Pancreatic Pseudocysts |
739 |
|
|
STEP 4
When the pseudocyst does not bulge through the mesocolon and is not adherent to the stomach or duodenum, the gastrocolic ligament is taken down to enter the lesser sac.
The Roux limb is brought retrocolic either to the right or left of the mesocolic vessels. The anastomosis of the pseudocyst is done as in Step 2.
