
clavien_atlas_of_upper_gastrointestinal_and_hepato-pancreato-biliary_surgery2007-10-01_3540200045_springer
.pdf698 |
SECTION 5 |
Portal Hypertension |
|
|
|
STEP 9 |
Side-to-side portacaval anastomosis |
|
|
|
|
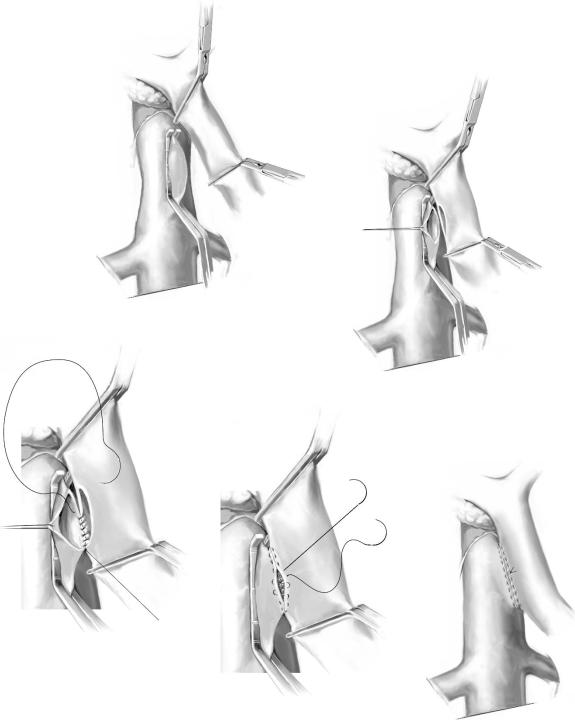
A Satinsky clamp is placed obliquely across a 5-cm segment of the anteromedial wall of the IVC in a direction parallel to the course of the overlying portal vein and the IVC is elevated toward the portal vein (A-1). A 5-cm segment of the portal vein is isolated between two angled vascular clamps and the portal vein is depressed toward the IVC, bringing the two vessels into apposition.
A 2.0- to 2.5-cm-long strip of the IVC and a 2.0- to 2.5-cm-long strip of the portal vein are excised with scissors (A-2). It is important to excise a longitudinal segment of the wall of each vessel rather than simply to make an incision in each vessel. A retraction suture of 5-0 silk is placed in the lateral wall of the IVC opening and is weighted by attachment to a hemostat to keep the IVC orifice open. The clamps on the portal vein are momentarily released to flush out any clots and then the openings in both vessels are irrigated with saline.
The anastomosis is started with a posterior continuous over-and-over suture of 5-0 vascular suture material (A-3). The posterior continuous suture is tied at each end of the anastomosis.
The anterior row of sutures consists of an everting continuous horizontal mattress stitch of 5-0 vascular suture material started at each end of the anastomosis (A-4). The suture started at the inferior end of the anastomosis is discontinued after three or four throws and is deliberately left loose so that the interior surface of the vessels can be visualized as the anastomosis is completed. In this way inadvertent inclusion of the posterior wall in the anterior row of sutures is avoided. The suture started at the superior end of the anastomosis is inserted with continuous tension until the inferior suture, at which point the inferior suture is drawn tight and the two sutures are tied to each other. Before drawing the inferior suture tight, the clamps on the portal vein are momentarily released to flush out any clots, and the anastomosis is thoroughly irrigated with saline (A-5).
Upon completion of the anastomosis, a single interrupted tension suture is placed just beyond each end of the anastomosis to take tension off the anastomotic suture line. The clamp on the IVC is removed first, the clamp on the hepatic side of the portal vein is removed next, and finally the clamp on the intestinal side of the portal vein is removed. Bleeding from the anastomosis infrequently occurs; it can be controlled by one or two well placed interrupted sutures of 5-0 vascular suture material.
Pressures in the portal vein and IVC must be measured after the anastomosis is completed. Usually the postshunt pressures in the portal vein and IVC are identical. A pressure gradient of >50mm saline between the two vessels indicates an obstruction in the anastomosis, even when no obstruction can be palpated. In such circumstances, the anastomosis should be opened to remove any clots and, if necessary, the entire anastomosis should be taken down and redone. It is essential that there be no more than a 50mm saline gradient between the portal vein and IVC to achieve permanently adequate portal decompression and to avoid ultimate thrombosis of the shunt.
Portacaval Shunts: Side-To-Side and End-To-Side |
699 |
|
|
|
|
STEP 9 (continued) |
Side-to-side portacaval anastomosis |
|
|
|
|
A-1
A-2
A-3
A-4
A-5
700 |
SECTION 5 |
Portal Hypertension |
|
|
|
STEP 10 |
Multiple steps in sewing an end-to-side portacaval anastomosis |
|
|
|
|
The end-to-side portacaval anastomosis is a satisfactory alternative to the side-to-side shunt in most cases, and some surgeons believe that it is somewhat less difficult to perform. It is not essential to isolate the IVC around its entire circumference, and it is often not necessary to clear as long a segment of the portal vein as in the lateral anastomosis. The disadvantage is that the liver sinusoids are not decompressed.
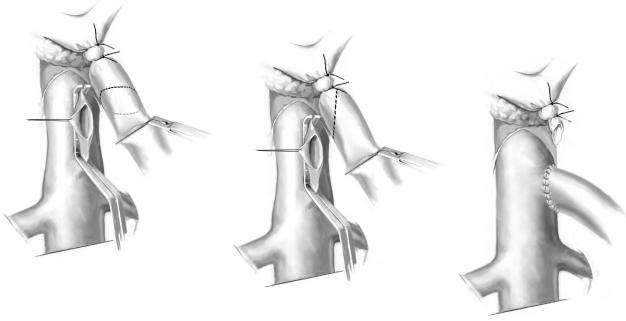
The Satinsky clamp on the IVC is placed obliquely on the anteromedial wall in the direction that will receive the end of the portal vein at an angle of about 45°. A 2-cm- long strip of the IVC is excised and a retraction suture is placed in the lateral wall (A-1). The portal vein is doubly ligated with a free ligature and a suture ligature of 2-0 silk just before its bifurcation in the hilum of the liver. An angled vascular clamp is placed across the portal vein near the pancreas, and the portal vein is divided obliquely just proximal to the ligation site.
In order to maximize the size of the anastomosis, the portal vein is transected tangentially so that the anterior wall is longer than the posterior wall at the transected end (A-2). After transection the clamp on the portal vein is momentarily released to flush out any clots before starting the anastomosis. This maneuver is repeated just before the final sutures in the anterior row of the anastomosis are placed.
The end-to-side anastomosis is performed with a continuous, over-and-over 5-0 vascular suture in the posterior row and a second 5-0 vascular suture in the anterior row (A-3). It is important that the portal vein describes a smooth curve in its descent toward the IVC and that it is attached to the IVC at an oblique angle. Twisting and kinking of the portal vein are the most common causes of a functionally unsatisfactory anastomosis. After the anastomosis is completed, pressure measurements are performed according to the guidelines described for the side-to-side shunt.
A-1
A-2
A-3
Portacaval Shunts: Side-To-Side and End-To-Side |
701 |
|
|
Liver Biopsy
A wedge liver biopsy is always obtained.
Postoperative Care
All patients should be admitted to an intensive care unit with equipment and personnel geared to managing the complicated problems associated with hepatic disease.
Monitoring
Careful monitoring of vital signs, central venous pressure, urine output, arterial pH, arterial and alveolar gases, fluid balance, body weight, and abdominal girth is essential.
Postoperative Complications
■Early:
–Hepatic failure
–Renal failure
–Infection
–Gastric acid hypersecretion
–Delirium tremens
–Ascites
–Gastrointestinal bleeding
■Late:
–Portasystemic encephalopathy (PSE)
–Liver failure
–Shunt thrombosis
–Hepatocellular carcinoma
702 |
SECTION 5 |
Portal Hypertension |
|
|
|
|
Tricks of the Senior Surgeon |
|
■The position of the patient on the operating table is crucial and can make the difference between an easy and difficult operation.
■A long subcostal incision is associated with many fewer postoperative complications than a thoracoabdominal incision and is much to be preferred.
■Use of the electrocautery throughout the operation substantially reduces the operating time and the blood loss.
■Bleeding from the many portasystemic collateral vessels is best managed by pressure with gauze sponge packs, particularly as most of the bleeding stops as soon as the portacaval anastomosis is completed and the portal hypertension is relieved. Attempts to control each of the bleeding collaterals with ligatures and sutures prolong the operation and increase the blood loss. The objective is to decompress the portal system as rapidly as possible.
■Circumferential mobilization of the inferior vena cava between the entrance of the renal veins and the liver is essential for the side-to-side anastomosis and is neither hazardous nor difficult to perform. Apposition of the two vessels is greatly facilitated by elevation of the vena cava toward the portal vein.
■Mobilization of a long segment of portal vein, which includes division of the tough fibrofatty tissue that binds the portal vein to the pancreas and sometimes includes division of a bit of the head of the pancreas, is essential for the side- to-side anastomosis and sometimes for the end-to-side anastomosis.
■Beware of the replaced hepatic artery crossing the portal vein behind the head of the pancreas. Palpate it with the index finger in the funnel between the head of the pancreas and portal vein. Ligation of the hepatic artery may be lethal.
■Resection of an enlarged caudate lobe of the cirrhotic liver to facilitate apposition of the two vessels is hazardous and unnecessary.
■Pressures in the IVC and portal vein should always be measured after completion of the portacaval shunt. A pressure gradient of greater than 50mm saline is unacceptable and requires revision of the anastomosis.
Gastroesophageal Devascularization: Sugiura Type
Procedures
Norihiro Kokudo, Seiji Kawasaki (Thoracoabdominal Approach with Splenectomy), Hector Orozco, Miguel A. Mercado (Complete Porto-azygos Disconnection
with Spleen Preservation),
Markus Selzner, Pierre-Alain Clavien (Abdominal Approach Only with Splenectomy)
Introduction
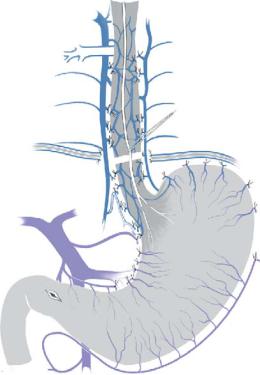
To improve the effect of Walker’s simple esophageal transection, Sugiura and colleagues refined the technique of esophageal transection, adding the extensive paraesophageal devascularization via abdominal and thoracic incisions. The resulting procedure has been known as the Sugiura procedure. Three different approaches will be described including a spleen preserving procedure as well as a procedure with an abdominal approach only (i.e., without thoracotomy).
Indications and Contraindications
Indications |
■ |
Bleeding or risky esophagogastric varices |
|
■ |
Esophagogastric varices resistant to endoscopic treatment |
|
■ |
Child-Turcotte (Pugh) Class A or B patients |
|
|
Child-Turcotte (Pugh) Class C patients |
Contraindications |
■ |
Preoperative Investigation and Preparation for the Procedure
History: |
Alcohol, hepatitis, recent overeating or overdrinking |
Clinical evaluation: |
Hematemesis, melena, encephalopathy, ascites, jaundice, |
|
nutritional status, splenomegaly, bleeding tendency |
Laboratory tests: |
Blood cell count, bilirubin, albumin, ALT, AST, prothrombin time, |
|
ammonia, total bile acid, indocyanine green test |
Endoscopy: |
Assessment of esophagogastric varices and portal hypertensive |
|
gastropathy, searching for the bleeding point |
CT scan, ultrasound, |
Assessment of collateral vessels, portal flow, ascites, searching |
or MRI: |
for hepatoma |
In emergency cases: |
Volume resuscitation, placement of Sengstaken-Blakemore tube, |
|
intratracheal intubation (when indicated) |
704 |
SECTION 5 |
Portal Hypertension |
|
|
|
|
|
|
Postoperative Tests |
|
|
|
■ |
Postoperative surveillance in an intensive or intermediate care unit |
|
|
■ |
Blood cell count, bilirubin, albumin, ALT, AST, and prothrombin time for at least 48h |
|
|
■ |
Check daily for clinical signs of gastrointestinal bleeding, liver failure, or pneumonia |
|
Postoperative Complications
■Short term:
–Liver failure
–Gastrointestinal bleeding
–Anastomotic leakage
–Pleural effusion
–Ascites
–Portal vein thrombosis
–Subphrenic abscess
–Pancreatic leakage
■Long term:
–Esophageal stricture
–Remnant varices
Gastroesophageal Devascularization: Sugiura Type Procedures |
705 |
|
|
Procedure 1:
Thoracoabdominal Approach with Splenectomy
Norihiro Kokudo, Seiji Kawasaki
Outline of the Procedure
Thoracoabdominal esophageal transection: The Sugiura procedure is a transthoraco abdominal esophageal transection, which consists of paraesophageal devascularization, esophageal transection and reanastomosis, splenectomy, and pyloroplasty. These thoracic and abdominal operations are performed in one or two stages depending
on the surgical risk of the patients. The most important and unique feature of this procedure is an extensive devascularization from the level of the left pulmonary vein to the upper half of the stomach 6–7cm along the lesser curvature below the cardia.
706 |
SECTION 5 |
Portal Hypertension |
|
|
|
STEP 1 |
Incision and exposure of the thoracic esophagus |
|
|
|
|
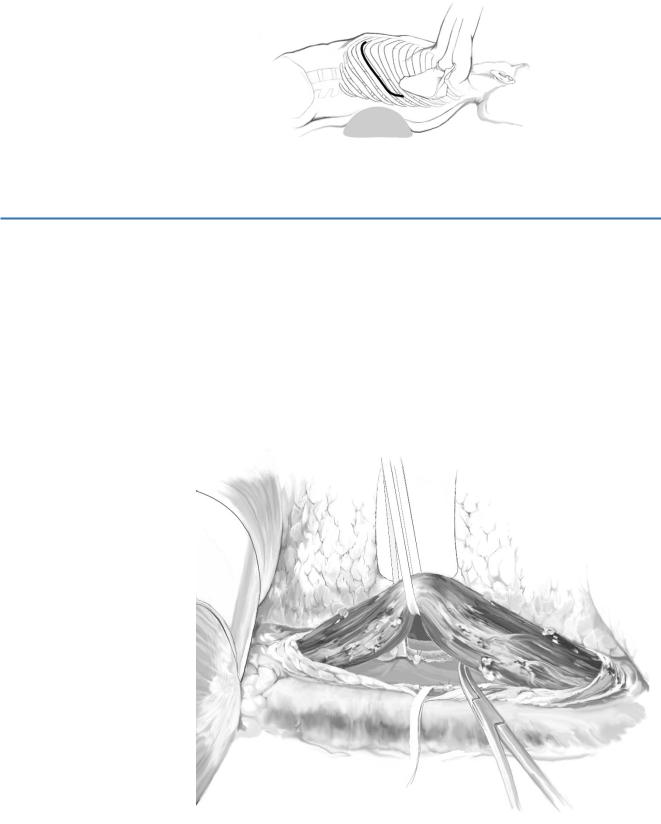
A standard left lateral thoracotomy incision is made, entering via the 7th intercostal space.
The inferior mediastinum is opened at the anterior portion of the descending aorta.
STEP 2 |
Paraesophageal devascularization |
|
Using a curved Kelly forceps, the thoracic esophagus is isolated and taped at a level |
|
|
|
where collateral veins are scant. In emergency cases, lifting of the tape facilitates hemo- |
|
stasis inside the esophagus. Lifting the esophagus, paraesophageal devascularization is |
|
performed. Many dilated collateral veins resembling a vein plexus can be recognized |
|
around the esophagus. They are parallel to the vagus nerves and have many shunts to |
|
the esophagus. All of these shunting veins must be completely ligated and divided, with |
|
care taken not to damage the truncus vagalis and collateral veins. There are usually |
|
about 30–50 shunting veins to be ligated. The length of devascularization of the thoracic |
|
esophagus is about 12–18cm. The upper edge of the devascularization is the inferior |
|
pulmonary vein, and the lower edge is where preperitoneal adipose tissue is exposed . |
Gastroesophageal Devascularization: Sugiura Type Procedures |
707 |
|
|
|
|
STEP 3 |
Esophageal transection 1 |
|
|
|
|
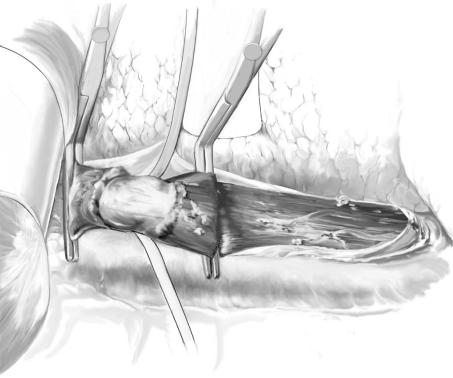
Upon completion of devascularization, the esophagus is doubly clamped with pairs of specially ordered esophageal clamps of the noncrushing, nonslipping type similar to Botallo’s forceps (“Sugiura’s clamp”). The distance between the two clamps is approximately 4cm. The two clamps are jointed with a thumbscrew in the mid-portion.
Esophageal transection is performed at the level of the diaphragm. The anterior muscular layer is divided with a knife and a tape passed around the submucosal layer.
