
clavien_atlas_of_upper_gastrointestinal_and_hepato-pancreato-biliary_surgery2007-10-01_3540200045_springer
.pdf688 |
SECTION 5 |
Portal Hypertension |
|
|
|
|
|
|
Preoperative Preparation During Acute Bleeding |
|
|
|
■ |
Temporary hemostasis with intravenous infusion of octreotide (50mcg/h) or |
|
|
|
vasopressin (0.2–0.4units/min) |
|
|
■ |
Temporary hemostasis during endoscopy by injection sclerotherapy or banding |
|
|
|
of esophageal varices |
|
|
■ |
Restoration of blood volume by transfusion of packed red blood cells and fresh |
|
|
|
frozen plasma through large-bore intravenous catheters |
|
|
■ |
Prevention of portasystemic encephalopathy by instillation via nasogastric tube |
|
|
|
of neomycin (4g), lactulose (30ml), and cathartics (60ml magnesium sulfate) |
|
|
■ |
Correction of hypokalemia and metabolic alkalosis by intravenous administration |
|
|
|
of large quantities of potassium chloride |
|
|
■ |
Intravenous administration of hypertonic glucose solution containing therapeutic |
|
|
|
doses of vitamins K, B, and C |
|
|
■ |
Preoperative administration of antibiotics |
|
|
■ |
Frequent monitoring of vital functions by an arterial catheter for blood pressure, |
|
|
|
a central venous catheter, and a urinary bladder catheter. Serial measurements |
|
|
|
of hematocrit, arterial pH and blood gases, and rate of blood loss by continuous |
|
|
|
suction through a nasogastric tube |
|
Portacaval Shunts: Side-To-Side and End-To-Side |
689 |
|
|
|
|
|
Procedure |
|
|
|
|
STEP 1 |
Position of patient |
|
|
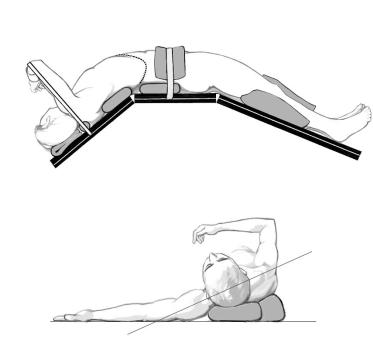
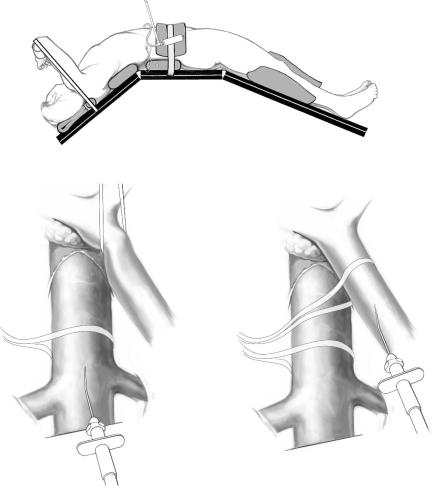
The patient is placed on the operating table with the right side elevated at an angle of 30° |
|
|
||
|
to the table by two sandbags placed underneath the right posterior trunk. The costal |
|
|
margin is at the level of the flexion break of the table, the right arm is suspended from |
|
|
an ether screen with towels, and the left arm is extended on an arm board cephalad to |
|
|
the ether screen. The table is “broken” at the level of the costal margin and at the knees |
|
so as to widen the space between the right costal margin and right iliac crest, and to make it possible to perform the operation easily through a right subcostal incision (A1, A-2). The incision extends from the xiphoid to well into the flank and is made two
finger breadths below the costal margin. The skin is incised superficially with the scalpel and the other layers with the electrocautery, which greatly reduces the blood loss and shortens the operating time. When the electrocautery is used, it is usually unnecessary to clamp any blood vessels with hemostats. The right rectus abdominis, external oblique, and transverse abdominis muscles are completely divided and the medial 3–4cm of the latissimus dorsi muscle is incised. The peritoneum often contains many collateral veins and is incised with the electrocautery to obtain immediate hemostasis.
A-1
A-2
690 |
SECTION 5 |
Portal Hypertension |
|
|
|
STEP 2 |
Exposure of operative field |
|
|
|
|
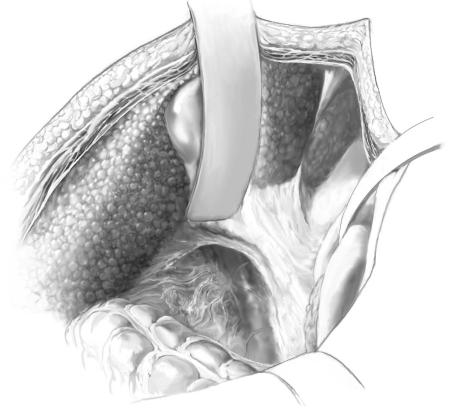
The operative field is exposed by retraction of the viscera with three Deaver retractors positioned at right angles to each other. The inferior one retracts the hepatic flexure of the colon toward the feet, the medial one displaces the descending duodenum medially and the superior retractor retracts the liver and gallbladder toward the head. Alternatively, a self-retaining retractor may be used to accomplish the same exposure. The posterior peritoneum is often intensely “stained” with portasystemic collateral veins.

Portacaval Shunts: Side-To-Side and End-To-Side |
691 |
|
|
|
|
STEP 3 |
Isolation of inferior vena cava |
|
|
|
|
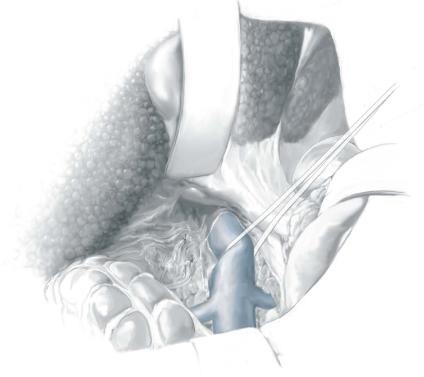
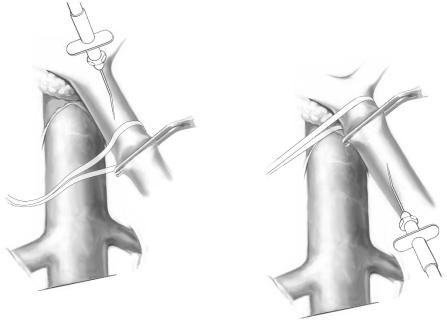
The inferior vena cava (IVC) lies behind the descending duodenum. The posterior peritoneum overlying the IVC is incised with the electrocautery by an extended Kocher maneuver just lateral to the descending duodenum, and the retractors are repositioned to retract the head of the pancreas medially and the right kidney caudally. The peritoneum is often greatly thickened and contains many collateral veins. Bleeding usually can be controlled with the electrocautery but sometimes requires suture ligatures.
The anterior surface of the IVC is cleared of fibroareolar tissue, and the IVC is isolated around its entire circumference by blunt and sharp dissection from the entrance of the right and left renal veins, below, to the point where it disappears behind the liver, above. The IVC is encircled with an umbilical tape. To accomplish the isolation, several tributaries must be ligated in continuity with fine silk ligatures and then divided. These tributaries often include the right adrenal vein, one or two pairs of lumbar veins that enter on the posterior surface, and the caudal pair of small hepatic veins from the caudate lobe of the liver that enter on the anterior surface of the IVC directly from the liver.
692 |
SECTION 5 |
Portal Hypertension |
|
|
|
STEP 4 |
Testing adequacy of IVC mobilization |
|
|
|
|
When the IVC has been mobilized completely, it can be lifted up toward the portal vein. Failure to isolate the IVC circumferentially is one major reason for the erroneous claim that the side-to-side portacaval shunt often cannot be performed because the portal vein and IVC are too widely separated.
Portacaval Shunts: Side-To-Side and End-To-Side |
693 |
|
|
|
|
STEP 5 |
Isolation of portal vein |
|
|
|
|
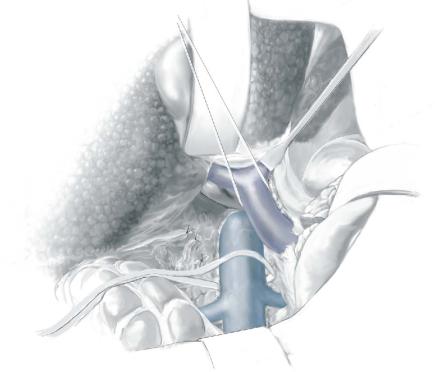
The superior retractor is repositioned medially so that it retracts the liver at the point of entrance of the portal triad. The portal vein is located in the posterolateral aspect of the portal triad and is approached from behind. The fibrofatty tissue on the posterolateral aspect of the portal triad, which contains nerves, lymphatics, and lymph nodes, is divided by blunt and sharp dissection. This technique is a safe maneuver because there are no portal venous tributaries on this aspect of the portal triad. As soon as the surface of the portal vein is exposed, a vein retractor or Gilbernet retractor is inserted to retract the common bile duct medially. The portal vein is mobilized circumferentially at its midportion and is encircled with an umbilical tape. It then is isolated up to its bifurcation in the liver hilum. Several tributaries on the medial aspect are ligated in continuity with fine silk and divided.
694 |
SECTION 5 |
Portal Hypertension |
|
|
|
STEP 6 |
Mobilization of portal vein behind pancreas |
|
|
|
|
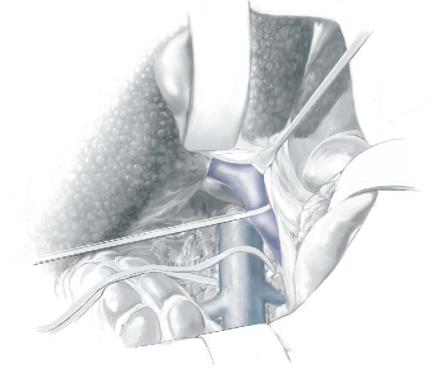
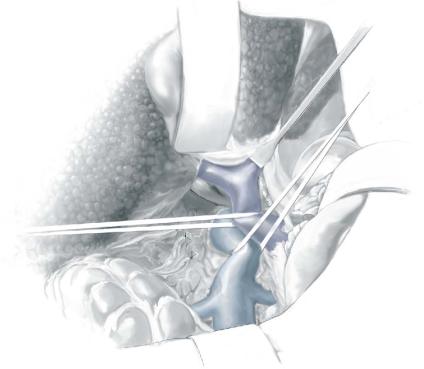
Using the umbilical tape to pull the portal vein out of its bed, the portal vein is cleared to the point where it disappears behind the pancreas. The tough fibrofatty tissue that binds the portal vein to the pancreas must be divided. Several tributaries that enter the medial aspect of the portal vein and one tributary that enters the posterolateral aspect are divided. It is usually not necessary to divide the splenic vein. Wide mobilization of the portal vein is essential for performance of a side-to-side portacaval anastomosis. Failure to mobilize the portal vein behind the pancreas is a second major reason for difficulty in accomplishing the side-to-side shunt. In some patients, it is necessary to divide a bit of the head of the pancreas between right-angled clamps to obtain adequate mobilization of the portal vein. Bleeding from the edges of the divided pancreas is controlled with suture ligatures. Division of a small amount of the pancreas is a very helpful maneuver and we have never observed postoperative complications, such as pancreatitis, from its performance. Before incising the pancreas, the surgeon should insert his or her index finger into the tunnel between the portal vein and the pancreas to determine by palpation if there is a replaced common hepatic or right hepatic artery arising from the superior mesenteric artery and crossing the portal vein. Since the portal venous blood flow to the liver is diverted through the portacaval shunt, ligation of the hepatic arterial blood supply may be lethal.
Portacaval Shunts: Side-To-Side and End-To-Side |
695 |
|
|
|
|
STEP 7 |
Testing adequacy of mobilization of portal vein and IVC |
|
|
|
|
To determine the adequacy of mobilization of portal vein and IVC, the two vessels are brought together by traction on the umbilical tapes that surround them . It is essential to determine that the two vessels can be brought together without excessive tension.
If this cannot be done, it is almost always because the vessels have not been adequately mobilized, and further dissection of the vessels should be undertaken. Resection of part of an enlarged caudate lobe of the cirrhotic liver, recommended by some surgeons to facilitate bringing the vessels together, is associated with some difficulties and, in our opinion, is neither necessary nor advisable.
Portacaval Shunts: Side-To-Side and End-To-Side |
697 |
|
|
|
|
STEP 8 (continued) |
Measurement of venous pressures |
|
|
|
|
A-4
A-5
