
clavien_atlas_of_upper_gastrointestinal_and_hepato-pancreato-biliary_surgery2007-10-01_3540200045_springer
.pdf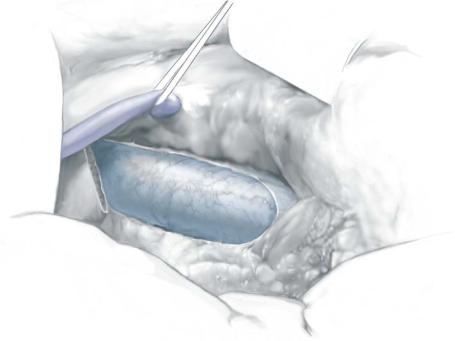
8MM Interposition Portacaval Shunt |
677 |
|
|
|
|
STEP 2 |
Exposure of portal vein |
|
|
|
It is very important that the inferior vena cava is well exposed medially and laterally so |
|
|
|
|
|
a vascular clamp can be placed. Exposure of at least one-half circumference of the 4- to |
|
|
5-cm segment of the inferior vena cava is usually necessary to facilitate secure clamp |
|
|
placement and anastomosis. After the inferior vena cava is adequately exposed, one or |
|
|
two traction sutures are placed into the loose tissue adjacent to the right side of the cava. |
|
|
These sutures are further placed into the lateral abdominal wall to retract laterally and |
|
|
optimize exposure. |
|
|
The gallbladder is retracted toward the patient’s left shoulder. This lifts and rotates |
|
|
the gallbladder and the common bile duct ventrally and medially. The hepatoduodenal |
|
|
ligament is then dissected posteriorly and laterally, along its whole length with attention |
|
|
to minimize chances of duct injury, as well as injury to an accessory or replaced right |
|
|
hepatic artery, if present. The common bile duct should be retracted ventrally and |
|
|
medially with a vein retractor to facilitate exposure of the portal vein. As the portal |
|
|
vein comes into view, a Russian forceps is used to grasp it and a plastic Yankauer sucker |
|
|
is utilized for circumferential dissection of the vein. The portal vein is then controlled |
|
|
by a vessel loop. This vessel loop may be helpful if bleeding develops because it can |
|
|
provide secure control of the portal vein. |
678 |
SECTION 5 |
Portal Hypertension |
|
|
|
STEP 3 |
Caval anastomosis |
|
|
|
|
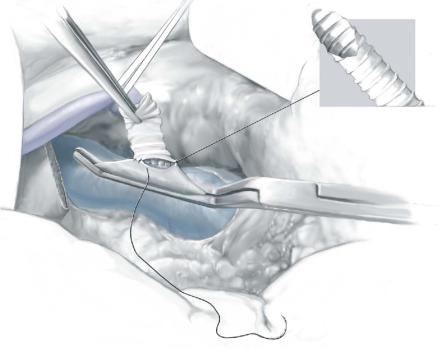
A segment of 8mm externally reinforced polytetrafluoroethylene (PTFE) graft is used for the portacaval shunt. The graft is 3cm long from toe to toe and 1.5cm from heel to heel. The bevels of the graft are oriented at 90degrees to each other because the portal vein is not parallel to but rather oriented approximately 60degrees to the inferior vena cava.
The graft is placed in heparinized saline and negative pressure is applied in order to remove any air bubbles. A side-biting Satinsky clamp is then securely placed on the anterior surface of the vena cava. Hypotension is virtually never a problem because of this clamping. A window must then be cut in the vena cava so that outflow from the graft is adequate; merely opening the cava is not sufficient. When the vena cava is opened, the ex vivo portion of the vein should be approximately 4mm long and 1–2mm wide. This will provide an adequate opening in the vena cava.
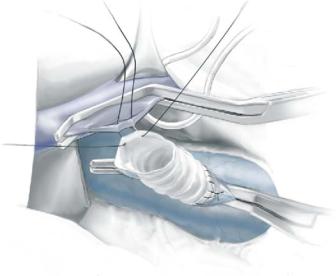
The graft is placed on the vena cava so that its bevel allows it to lean cephalad. The anastomosis is undertaken with 5-0Prolene in a running fashion. This anastomosis is initiated with a horizontal mattress suture so that sewing is always from “inside-out” on the vein and “outside-in” on the graft (Figure 3). The back wall is completed first. Before the knot is tied, a suture is reversed so that the knot is secured across the anastomosis.
8MM Interposition Portacaval Shunt |
679 |
|
|
|
|
STEP 4 |
Testing the caval anastomosis |
|
|
|
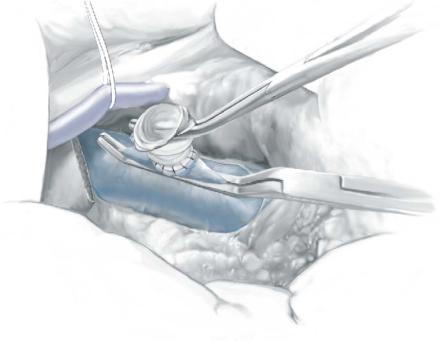
Once the anastomosis has been completed and the knot tied, a right-angled clamp is |
|
|
|
|
|
placed across the graft, and the side-biting clamp is removed. This tests the anastomosis; |
|
|
it should not leak and it should only bleed at needle holes and then only minimally |
|
|
(Figure 4). The Satinsky clamp is repositioned on the vena cava and the right-angled |
|
|
clamp removed from the graft. The graft is then vigorously irrigated with heparinized |
|
|
saline through an 18-gauge angiocatheter. |

680 |
SECTION 5 |
Portal Hypertension |
|
|
|
STEP 5 |
Exposure of the portal vein |
|
|
|
|
The portal vein anastomosis is now constructed. The common bile duct and accessory right hepatic artery, if present, are retracted ventrally and medially, exposing the dissected portal vein. The bevel of the portal vein end of the graft is at 90° to the IVC level as shown here.
8MM Interposition Portacaval Shunt |
681 |
|
|
|
|
STEP 6 |
Preparation of the portal anastomosis |
|
|
|
A right-angled side-biting clamp is then placed across the portal vein. This clamp does |
|
|
|
|
|
not have to occlude all the portal flow, but it must be placed securely enough to prevent |
|
|
bleeding once the vein is opened. Once the Satinsky clamp is placed, the posterolateral |
|
|
surface of the portal vein is incised with a No. 11 knife blade. Potts scissors are then used |
|
|
to lengthen the opening in order to accommodate the placement of the graft. In contrast |
|
|
to the inferior vena cava, a window does not usually need to be cut in the portal vein. |
|
|
A 5-0 Prolene suture is placed in the ventral edge of the opening in the portal vein to act |
|
|
as a retraction suture, so as to “open up” the hole in the vein. |
682 |
SECTION 5 |
Portal Hypertension |
|
|
|
STEP 7 |
Portal anastomosis |
|
|
|
|
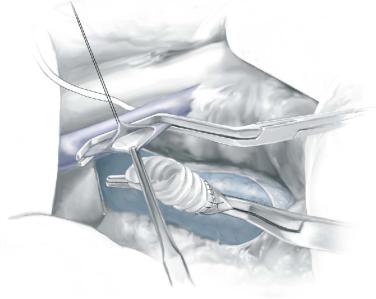
With this exposure, the posterior wall of the portal vein is then sewn to the graft with a 5-0 Prolene suture. The anastomosis is initiated by placing a horizontal mattress suture in the midportion of the posterior wall of the portal vein. Thereafter, all sewing of this anastomosis is “inside-out” on the portal vein and “outside-in” on the graft. As sewing is carried around both the cephalad and caudad corners of the anastomosis, the sutures along the back wall are drawn taut with a nerve hook. As the sewing continues toward the middle of the anterior portion of the anastomosis, the clamp on the portal vein
is momentarily opened so that clot and debris within the vein will be blown out. Heparinized saline is again applied liberally through the anterior defect of the anastomosis into the graft.

8MM Interposition Portacaval Shunt |
683 |
|
|
|
|
STEP 8 |
Completing the anastomosis |
|
|
|
The anastomosis is then completed, with one of the sutures reversed so that the knot is |
|
|
|
|
|
tied across the anastomosis. The clamp on the vena cava is released first, and then the |
|
|
clamp on the portal vein is removed. There should be a thrill in the vena cava, just |
|
|
cephalad to the anastomosis. |
684 |
SECTION 5 |
Portal Hypertension |
|
|
|
|
|
|
Postoperative Tests |
|
|
|
■ |
Postoperative surveillance in an appropriate hospital setting. |
|
|
■ |
Remove nasogastric tube, if present, as soon as possible. |
|
|
■ |
Attention should be given to avoid dehydration. Low urinary output during the first |
|
|
|
24–48h predisposes to graft thrombosis. |
|
|
|
If hypovolemia is diagnosed, rehydration with normal saline and use of intravenous |
|
|
|
mannitol are recommended. |
|
|
■ |
Liver function tests (including SGOT), coagulation parameters, and hemoglobin |
|
|
|
should be checked for at least 48h, postoperatively. |
|
|
■ |
Daily assessment of clinical signs of liver failure, such as jaundice and |
|
|
|
encephalopathy. |
|
|
■ |
Ascites can be controlled with fluid and salt restriction, as well as with judicious use |
|
|
|
of diuretics. |
|
|
■ |
The shunt should be evaluated with transfemoral cannulation, in order to document |
|
|
|
patency and to measure the portal vein-inferior vena cava pressure gradients at |
|
|
|
3–6days postoperatively. |
|
Complications
■Intra-abdominal bleeding
■Recurrence of gastrointestinal hemorrhage due to shunt thrombosis
■Hepatic failure
■Changes in cardiopulmonary dynamics (increased cardiac index)
■Ascites
■Portal-systemic encephalopathy
■Bile duct injury
■Injury to an accessory right hepatic artery
■Wound infection
■Shunt failure
Summary
Pressures within the portal vein and inferior vena cava are measured early in the operation, before the vessels are clamped. These pressures can be recorded with a 25-gauge needle and a pressure-transducing setup. A portal-caval pressure gradient is determined. On completion of the shunt, pressures are measured again. In a satisfactorily completed shunting, we look for a decrease in portal pressure of ≥10mmHg and a gradient between the portal vein and the inferior vena cava of less than 10mmHg.
The vena cava-graft anastomosis is marked with large Hemoclips placed on tissue adherent to the cava and secured both cephalad and caudad to the anastomosis. These clips allow the radiologist to identify and cannulate the inferior vena cava-graft anastomosis during the routine postoperative assessment of the shunt.
After copious irrigation of the operative field, the wound is closed along anatomic layers using #2 Prolene suture. The skin is reapproximated with a running nylon suture, in order to minimize any postoperative ascitic leak.
8MM Interposition Portacaval Shunt |
685 |
|
|
Tricks of the Senior Surgeon
■Identify the foramen of Winslow. The Kocher maneuver should be limited.
■Cut a window in the inferior vena cava.
■Begin each anastomosis with a horizontal mattress suture.
■Check the graft-inferior vena cava anastomosis before proceeding with the portal vein-graft anastomosis.
■If there is significant bleeding when a portion of the caudate lobe is removed, apply pressure and most of the bleeding will drop within minutes.
■Bleeding from either anastomosis is generally best managed by using a figure- of-eight technique.

Portacaval Shunts: Side-To-Side and End-To-Side
Marshall J. Orloff, Mark S. Orloff, Susan L. Orloff
Indications and Contraindications
Indications |
■ |
Bleeding esophageal or gastric varices (BEV or BGV) due to portal hypertension |
|
|
caused by cirrhosis, or, much less commonly, caused by other liver diseases |
|
|
(e.g., schistosomiasis) |
|
■ |
Bleeding from portal hypertensive gastropathy unresponsive to pharmacologic |
|
|
therapy |
|
■ |
Budd-Chiari syndrome with patent inferior vena cava |
|
■ |
Intractable ascites unresponsive to nonsurgical therapy |
|
■ |
Failed transjugular intrahepatic portasystemic shunt (TIPS) |
|
|
Thrombosis of the portal vein without liver disease (extrahepatic portal |
Contraindications |
■ |
|
|
|
hypertension) |
|
■ |
In patients with liver disease, thrombosis of the portal vein that is long-standing |
|
|
and not amenable to venous thrombectomy |
|
■ |
Occlusion of the hepatic artery (e.g., due to hepatic arterial infusion chemotherapy) |
Timing Considerations
■Prophylactive portacaval shunt in patients with esophageal or gastric varices that have never bled – practiced by some surgeons but not recommended by the authors
■Elective therapeutic portacaval shunt in patients who have recovered from an episode of BEV or BGV. This is the most widely used form of portacaval shunt
■Emergency portacaval shunt within 48h of the onset of BEV or BGV, strongly advocated by the authors
Diagnosis of BEV or BGV
■History and physical examination to confirm diagnosis
■Blood studies for complete evaluation
■Esophagogastroduodenoscopy
■Doppler ultrasonography to determine portal vein patency and absence of gross liver tumors
■Other studies occasionally necessary:
a)Visceral arteriography with indirect portography and inferior vena cavography with pressure measurements – usually not necessary in cirrhosis but essential in extrahepatic portal hypertension and Budd-Chiari syndrome
b)Hepatic vein catheterization with venography and wedged hepatic vein pressure measurements
c)Percutaneous liver biopsy – usually not necessary in cirrhosis but helpful in Budd-Chiari syndrome
