
clavien_atlas_of_upper_gastrointestinal_and_hepato-pancreato-biliary_surgery2007-10-01_3540200045_springer
.pdf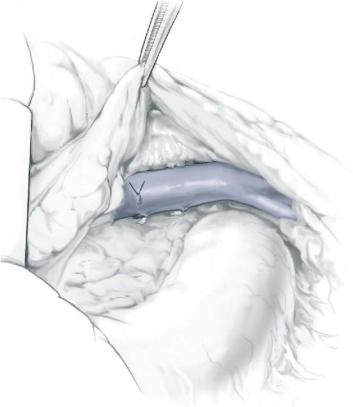
666 |
SECTION 5 |
Portal Hypertension |
|
|
|
|
Procedure |
|
|
|
|
STEP 1 |
Access and mobilization |
|
|
The abdomen is entered through a large median or transverse incision, to obtain |
|
|
||
|
adequate exposure of the whole cavity. A retractor (Thompson, Omni-Tract) is placed |
|
|
with blades that expose the root of the mesentery in the inframesocolic compartment. |
|
|
Traction of the transverse colon up and forward of the mesentery (caudal) exposes the |
|
|
third portion of the duodenum. The peritoneum is incised, in a semicircular fashion, |
|
from the root of the mesocolon to the ligament of Treitz. Only lax adhesions are usually found with occasional small veins that need electrocoagulation. The duodenum is freed completely.
The peritoneum is cut at the root of the mesentery, exposing the lymphatics (usually dilated and hypertrophied) that surround the mesenteric vessels. Chronic lymphatic hypertension produces fibrosis that makes dissection difficult. It is necessary to ligate all these structures in order to avoid postoperative lymph leakage. Also, small dilated veins can be found.
Complete dissection of the anterior and right lateral aspect of the superior mesenteric vein is done. All the vessels from the uncinate process of the pancreas (variable in length, diameter and distribution) are carefully dissected and ligated. The dissection is continued cephalad to the neck of the pancreas. The middle colic vein is ligated.
Caudally, the dissection is continued down to the confluence of the ileocolic branch (which in many instances can be preserved). In some instances the ileocolic artery crosses over at this level; it can usually be retracted, but if necessary it can be ligated. It is necessary to dissect free the mesenteric vein 4–5cm in length. Also, it is important to dissect the whole circumference of the vessel in order to comfortably place the vascular clamp.
Low-Diameter Mesocaval Shunt |
667 |
|
|
STEP 2 |
Preparation of the inferior vena cava |
|
The infrarenal IVC is dissected free, after removing the lax areolar tissue that surrounds |
|
|
|
it. Some small veins are found that have to be suture ligated. It is not necessary to dissect |
|
the vessel in its whole circumference since it is easy to place the vascular clamp on the |
|
anterior wall of the IVC due to its width and low intravascular pressure. |
668 |
SECTION 5 |
Portal Hypertension |
|
|
|
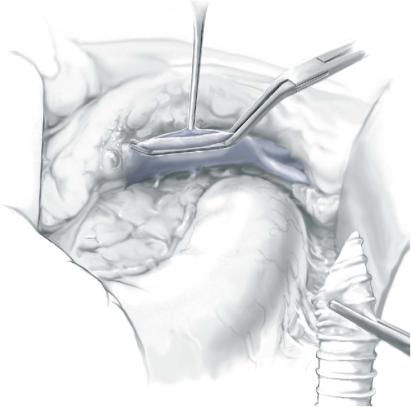
STEP 3 |
Venotomy of the vena cava |
|
|
|
|
Retractors are placed to separate the duodenum (cephalad), the right colon (lateral) and the small intestine (caudal). Lymph nodes around the aorta can be observed; this is the limit of the medial dissection.
A Satinsky clamp is placed and a longitudinal venotomy is done approximately 12–14mm in length using DeBakey scissors, in order to obtain an oval venotomy.
Low-Diameter Mesocaval Shunt |
669 |
|
|
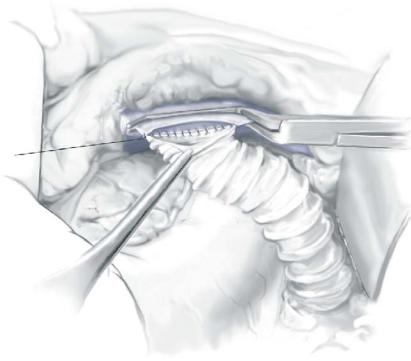
STEP 4 |
Suture on the caval side |
|
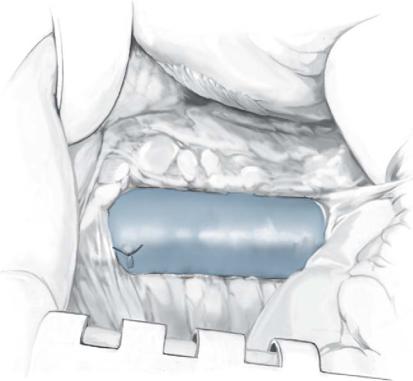
A ring reinforced polytetrafluoroethylene (PTFE) 10-mm graft is cut in tangential |
|
|
|
fashion in order to obtain a 12 - to 14-mm opening for anastomosis. If the decision to |
|
place a wider graft has been made, a wider venotomy must be performed. |
|
Using a 5-0 vascular Prolene suture placed at each angle, the graft is sewn with a |
|
running suture (Figure 4). The suture is placed from outside. An everted suture is |
|
advised at this point in order to minimize exposure of rough areas in the vascular |
|
lumen. |
|
When the suture is completed, the graft is filled with heparinized saline. |
670 |
SECTION 5 |
Portal Hypertension |
|
|
|
STEP 5 |
Preparation and suture on the mesenteric side |
|
|
|
|
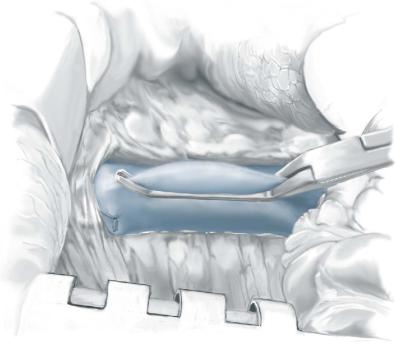
A Satinsky clamp is placed on the superior mesenteric vein and a semicircular cut of the vein is done with Potts scissors (Figure 5). This incision favors the position of the graft in the right and slightly posterior aspect of the vein. Using a 5-0 Prolene suture, each angle is placed and the PTFE graft is approximated close to the vein. The length of the graft has to be cut according to the position of the duodenum.
Low-Diameter Mesocaval Shunt |
671 |
|
|
STEP 6 |
Completing the suture |
|
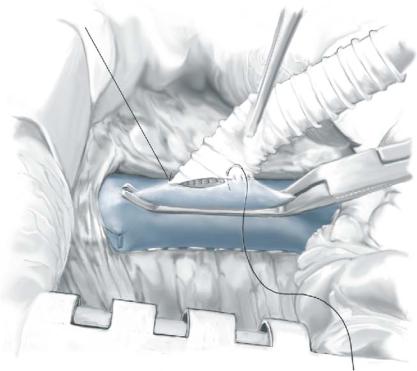
The anastomosis is completed using a continuous suture. The posterior layer is done |
|
|
|
from within the lumen, so that the first stitch places the needle inside the lumen |
|
(Figure 6). When the posterior aspect is completed, the needle is brought outside |
|
and then the anterior layer of the anastomosis is done. An everted suture is advised. |
672 |
SECTION 5 |
Portal Hypertension |
|
|
|
STEP 7 |
Release of the clamps |
|
|
When the suture is complete, the vascular clamp in the inferior vena cava is released first |
|
|
||
|
followed by the vascular clamp in the mesenteric vein. Usually a small amount of |
|
|
bleeding at the suture line is observed. This resolves spontaneously with the application |
|
|
of dehydrated cellulose and mild pressure. |
|
|
|
|
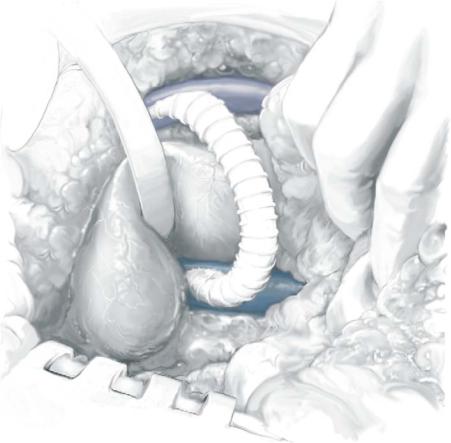
STEP 8 |
Final position |
|
|
The final position of the graft. The duodenum is allowed to rest over the graft and the |
|
|
||
|
peritoneum is closed over the graft. No drainage is left and the abdominal wall is closed |
|
|
in standard fashion. |
|
Low-Diameter Mesocaval Shunt |
673 |
|
|
Postoperative Tests
■Daily laboratory studies
■Shunt study prior to discharge
–Ultrasound
–Possible angiography
Postoperative Complications
■Early:
–Liver failure
–Shunt thrombosis
■Late:
–Liver decompensation
–Encephalopathy
–Shunt thrombosis
Tricks of the Senior Surgeon
■Injection of water around the vessels, through a small orifice when the vessel is identified, allows separation of dissection planes, making the dissection easier.
■Circumferential dissection of the mesenteric vein permits an easier mobilization of the vessel. Fixed segments of the wall can produce small tears of the vessel at the time of clamping and when traction to the vessel is done.
■When the posterior face of the mesenteric anastomosis is performed, it is important to maintain the graft close to the vein. Traction to the graft when the first stitches are placed can produce tears in the vein wall and loss of substance.
■When bleeding is observed at the anastomotic suture line, it is better to wait until it stops spontaneously. Placing new stitches can be troublesome because the wall is under tension and a larger hole can be made.

8MM Interposition Portacaval Shunt
Alexander S. Rosemurgy II, Dimitris P. Korkolis
Indications and Contraindications
Indications |
■ |
Control of acute hemorrhage from esophageal varices not amenable to or failing |
|
|
medical therapy, e.g., pharmacotherapy, balloon tamponade, endoscopic variceal |
|
|
sclerotherapy, in patients with liver cirrhosis and portal hypertension |
|
■ |
Control of bleeding gastric or intestinal varices |
|
■ |
Prevention of recurrent variceal bleeding after initial control |
|
■ |
Complicated Budd-Chiari syndrome |
|
|
Portal vein thrombosis, even with recanalization (cavernomatous transformation) |
Contraindications |
■ |
|
|
■ |
Inferior vena cava thrombosis |
|
■ |
Extensive adhesions from previous operative procedures in the right upper quadrant |
|
|
(relative contraindication) |
|
■ |
Severe medical comorbidities (e.g., mitral regurgitation, severe aortic stenosis, etc.) |
Preoperative Investigation and Preparation for the Procedure
History: |
Alcohol consumption and alcohol withdrawal syndromes, |
|
hepatitis and hepatotoxic medications |
Clinical evaluation: |
Variceal bleeding, ascites, hypersplenism, hepatic |
|
encephalopathy, jaundice, nutritional status, signs of portal |
|
hypertension (e.g., caput medusa) |
Laboratory tests: |
ALT, AST, bilirubin, alkaline phosphatase, albumin, coagula- |
|
tion profile (PT, INR, platelets), tumor markers and serologies |
|
(e.g., hepatitis), when indicated. Electrolyte and acid-base |
|
profile |
Color-flow Doppler |
Assessment of portasplanchnic patency, as well as patency |
ultrasound and |
of the inferior vena cava |
visceral angiography: Determination of Child-Pugh score
676 |
SECTION 5 |
Portal Hypertension |
|
|
|
|
Procedure |
|
|
Positioning, Access and Mobilization |
|
|
Initially, the patient is positioned supine on the operating table. A nasogastric tube is |
|
|
placed only if gastric distension requires it. Neither vasopressin nor octreotide need to |
|
|
be given perioperatively, unless active bleeding is occurring. Otherwise, the operation |
|
|
can be undertaken with minimal blood loss and almost always without blood transfu- |
|
|
sion. The patient is then rolled into a 30-degree left lateral decubitus position by means |
|
|
of a bed sheet rolled tightly and placed just to the right of the spine. |
|
|
The patient is operated on through a right transverse upper abdominal incision. |
|
|
The exact placement of this incision depends on the size of the liver, which is often |
|
|
palpable below the right costal margin. The incision is placed over the liver edge. |
|
|
It does not generally cross the midline and includes only a small portion of the muscu- |
|
|
lature lateral to the rectus muscle. |
|
|
If the falciform ligament is divided during the incision, it should be divided carefully, |
|
|
as it may contain large collateral vessels. Suture ligation of the falciform ligament at the |
|
|
time of the division is usually undertaken. |
|
|
|
|
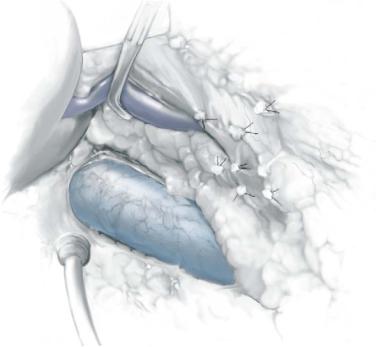
STEP 1 |
Kocherization and preparation of the vena cava |
|
|
Optimum exposure of the right upper quadrant of the peritoneal cavity should be |
|
|
||
achieved, with as little dissection as possible. The foramen of Winslow is the key landmark. A limited Kocher maneuver is undertaken, always maintaining orientation with the foramen of Winslow. Visible venous collaterals, as well as large lymphatic channels, should be ligated before division. Cautery is liberally applied. The Kocher maneuver does not need to be extensive but just enough to adequately expose 5cm of the subhepatic inferior vena cava and enable the placement of a side-biting vascular clamp.
The exposed segment of the inferior vena cava should include the portion that forms the dorsal border of the foramen of Winslow. The cephalad area of this segment of
the cava may lie dorsal to the inferior tip of the caudate lobe of the liver. If necessary, this portion of the caudate lobe should be excised with electrocautery.
