
clavien_atlas_of_upper_gastrointestinal_and_hepato-pancreato-biliary_surgery2007-10-01_3540200045_springer
.pdf
632 SECTION 4 Biliary Tract and Gallbladder
Timing of Repair
Factors favoring immediate repair are: (1) early referral, (2) lack of right upper quadrant bile collection, (3) simple injuries, (4) no vascular injury and (5) a stable patient. Factors favoring delayed repair are: (1) late (less than 1week after injury) referral, (2) complex injuries (types E4, E5), (3) thermal etiology and (4) concomitant ischemic injury.
Preoperative Investigation and Preparation for the Procedure
■Communication with previous surgeon
■Previous surgical report
■Laboratory tests: bilirubin, alkaline phosphatase, ALT, AST, albumin, coagulation parameters, white blood cell count
Principles of Repair
■Anastomosis should be tension free, with good blood supply, mucosa to mucosa and of adequate caliber.
■Hepaticojejunostomy should be used in preference to either choledochocholedocotomy or choledochoduodenostomy.
■An anterior longitudinal opening in the bile duct with a long side-to-side anastomosis is preferred.
■Dissection behind the ducts should be minimized in order to minimize devascularization of the duct.
Use of Postoperative Stents
■There is no evidence that they are helpful if a large caliber mucosa-to-mucosa anastomosis has been achieved.
■We use them when very small ducts have been anastomosed.
■Transhepatic tubes can be left through the anastomosis in order to perform postoperative cholangiography.
More Radical Solutions
■When ductal reconstruction to a part of the liver is impossible, then resection should be performed.
■Occasionally prior failure of reconstruction leads to secondary biliary cirrhosis, end-stage liver failure, and a need for liver transplantation.
Reconstruction of Bile Duct Injuries |
633 |
|
|
Procedure
Incision
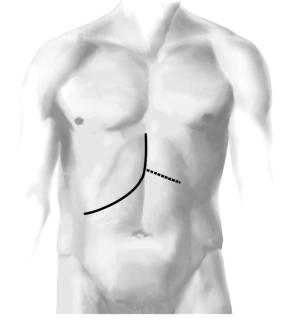
The usual incision is a J-shaped right upper quadrant incision shown as a solid line. The vertical length of the incision should be at least 6 cm. The incision can be extended to the left (dotted line for increased exposure in large individuals). A midline incision may be suitable for thin persons. A large ring retractor is placed after clearing adhesions to the anterior abdominal wall.

Reconstruction of Bile Duct Injuries |
635 |
|
|
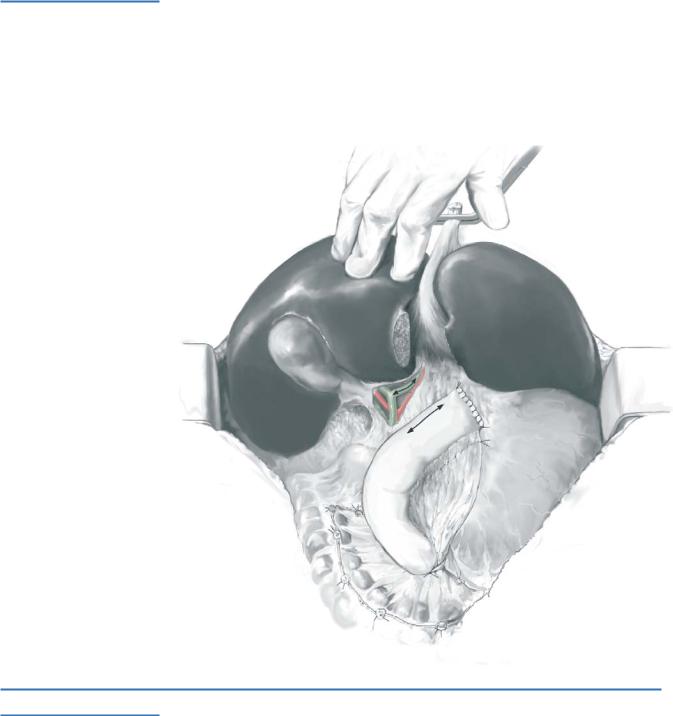
STEP 2
At this point a stent in the left duct can be palpated and the duct opened on its anterior surface. A 2-cm opening is adequate. Care should be taken not to extend the incision too far to the left, as the hepatic artery to segment 4 may be injured. Segment 4 is pulled up, the liver plate divided and the left hepatic duct identified. A Roux-en-Y loop has been prepared. The loop is laid up as shown. The double-headed arrows indicate the sites of openings that are made in the duct and the bowel.
STEP 3
The anastomosis is performed with synthetic absorbable interrupted sutures (5-0 sutures are preferred by the author). The anterior row in the bile duct is placed first, then the posterior row in both structures is placed and tied, and finally the anterior row is placed in the bowel and tied (see chapter on biliary-enteric anastomosis: pages). A single suction drain is left. Stents are used only when the bile ducts are very small
2 mm or less; this is very uncommon.
636 SECTION 4 Biliary Tract and Gallbladder
Cases of Isolated Right Hepatic Duct
In types E4 and E5 and B and C injuries the Hepp-Couinaud approach alone will not suffice, as there is an isolated portion of the biliary tree on the right side. The key to dissection is based on the fact that the main right and left bile ducts lie in the same coronal plane, invested in fibrous Wallerian sheaths. Also of importance is that the gallbladder plate, a layer of fibrous tissue on which the gallbladder normally rests, attaches to the anterior surface of the sheath of the main right portal pedicle. To find the bile duct within the sheath of the pedicle the cystic plate must be detached from the anterior surface of the sheath of the right portal pedicle.
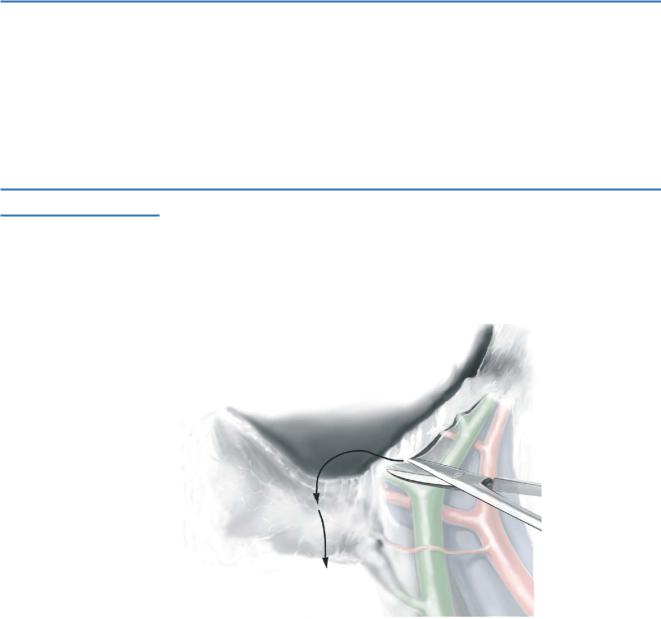
STEP 1
The liver capsule is divided toward the right until the cystic plate is met where it attaches to the sheath of the right portal pedicle. It is a stout ribbon of fibrous tissue about 2mm in thickness and 5–8mm in breadth.
Reconstruction of Bile Duct Injuries |
637 |
|
|
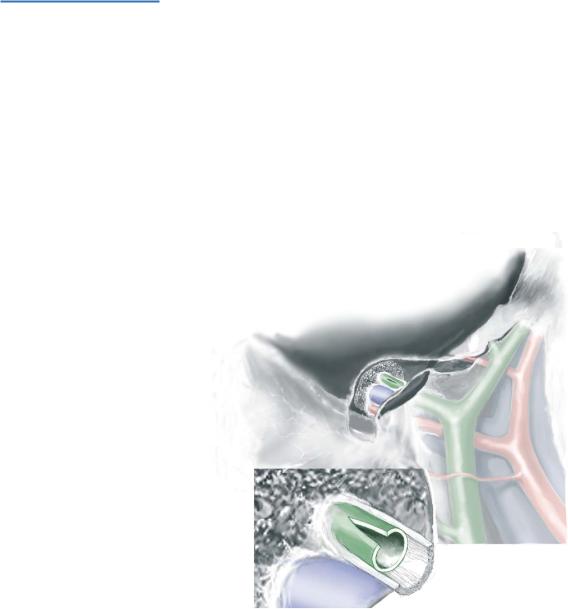
STEP 2
After dividing the cystic plate the liver lifts off the right portal pedicle. The division of the liver capsule is carried about 1cm beyond the cystic plate. Now the liver (segment 5) may be dissected off the portal pedicle, by lifting and coring the base of segment 5. This exposes the anterior surface of the sheath of the right portal pedicle. The position of the right duct(s) in the pedicle is evident from the position of the stent (not shown). To prepare the right bile duct for anastomosis it is opened on the anterior surface (inset). Ideally, the duct(s) is opened 1cm. The entire anastomosis is then performed to the anterior surface of the duct as described above for the left duct. When performing two (or more) anastomoses the anterior row in the bile ducts should be placed first and then the posterior row placed and tied, completing all anastomoses together by placement
of the anterior row sutures in the bowel and tying of all anterior row sutures.
638 SECTION 4 Biliary Tract and Gallbladder
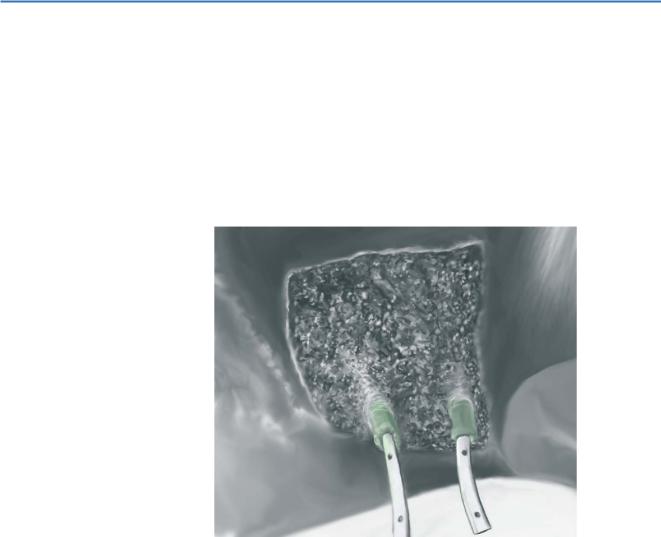
Access to Intrahepatic Ducts Provided by Partial Hepatectomy
In some cases, especially those in which there have been repeated bouts of cholangitis and the liver has become swollen and fibrotic, a condition most frequently seen after failed hepaticojejunostomy, segment 4 may overhang the upper bile ducts. In these cases resection or coring of segment 4 is also a useful adjunct. Resection provides excellent access to the upper part of the porta hepatis without relying on forceful retraction on the liver and provides room for the bowel to rest when the hepaticojejunostomy is performed. This maneuver is not restricted only to operations in which a portion of
the right biliary tree has been isolated. It is also useful for types E3 and some E2 injuries. Bile ducts with stents may be seen at the bottom of the picture.
Reconstruction of Bile Duct Injuries |
639 |
|
|
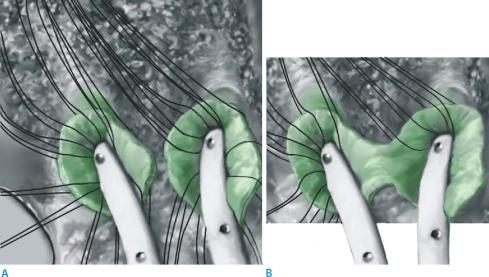
Close-up of bile ducts. Type E4 injury in which the right bile ducts have been exposed by dividing the gallbladder plate as described and segment 4 has been partially resected. Preoperatively placed stents are emanating from the ducts, and the ducts have been incised on their anterior surfaces for 1.5cm. Sutures have been placed in the anterior row of the proposed anastomosis along with a few in the posterior row (A).
In figure B it was chosen to do a “cloacal” anastomosis rather than a double-barreled anastomosis because the ducts were close and the intervening scar small. Although the center of the anastomosis may scar, the long lateral horns are mucosa to mucosa and effectively a double-barreled anastomosis results.
642 |
SECTION 4 |
Biliary Tract and Gallbladder |
|
|
|
|
|
|
Indications and Contraindications |
|
|
|
|
Symptoms (jaundice, pain, cholangitis) |
|
Indications |
■ |
|
|
|
■ |
Suspected or established malignancy |
|
|
■ |
Type I choledochal cyst |
|
|
■ |
Type II choledochal cyst |
|
|
■ |
Type IV choledochal cyst |
|
|
■ |
Previous cyst-enterostomy |
|
|
|
Severe liver disease (e.g., Child-Pugh C cirrhosis) |
|
Contraindications |
■ |
|
|
|
■ |
Severe portal hypertension |
|
|
■ |
Coagulopathy |
|
Investigation/Preparation
Clinical: |
Chronic liver disease |
Laboratory tests: |
Bilirubin, alkaline phosphatase, ALT, albumin, prothrombin |
|
time, platelets |
Radiologic tests: |
Non-invasive; ultrasound, abdominal CT scan, invasive MRCP; |
|
ERCP if intrahepatic ducts are not visualized on MRCP |
Operative preparation: |
Antibiotics to cover biliary pathogens |
