
clavien_atlas_of_upper_gastrointestinal_and_hepato-pancreato-biliary_surgery2007-10-01_3540200045_springer
.pdf612 |
SECTION 4 |
Biliary Tract and Gallbladder |
|
|
|
|
Investigation and Preparation |
|
Clinical
■Pain in the right upper abdomen
■Weight loss/catabolic state
■Icterus
■Pruritus
■Coagulopathy
■Hepatorenal dysfunction
■Cholangitis
Laboratory Tests
Liver-specific function: Lactate dehydrogenase (LDH), ALT, AST, g–glutamyl transpep-
|
tidase (GGT), and alkaline phosphatase, bilirubin |
Prothrombin time: |
Coagulation test in case of an interrupted enterohepatic circle |
Radiology |
|
Ultrasound: |
Origin, location and type of the obstruction, width of the intra- |
|
and extrahepatic bile ducts and the possibility of relieving the |
|
bile ducts by percutaneous transhepatic drainage |
Three-phase CT scan: |
Extent of the obstructive lesion, local resectability and |
|
relation to the surrounding structures (the portal vein and |
|
the common hepatic artery) |
What We Should Not Do
Preoperatively, one should consider whether the morbidity and mortality of the surgical procedure outweigh the life expectancy of the patient. Often one is confronted with inoperability during exploration. In such situations, biliary bypass can be performed as a palliative measure. However, postoperative stent placement is preferred if life expectancy is short.
If preoperative drainage of the obstruction is required, plastic endoprotheses are the equipment of choice, because they are easier to remove during surgery. The placement of wall stents should be avoided in obstructive bile duct disease.
Preparation Prior to Surgery
■Correction of the coagulopathy through administration of vitamin K
■Preoperative drainage may lead to increased morbidity because of biliary infections. However, preoperative drainage is done in the majority of cases for logistic reasons
■Antibiotic prophylaxis
Choledochojejunostomy and Cholecystojejunostomy |
613 |
|
|
|
|
|
Procedure |
|
|
Access |
|
|
Either a subcostal incision, with the possibility of extending this incision to the left side |
|
|
of the abdomen, or a midline incision may be chosen. If percutaneous transhepatic |
|
|
cholangiography (PTC) is in place, the incision should be chosen to avoid having to |
|
|
remove the PTC perioperatively. |
|
|
|
|
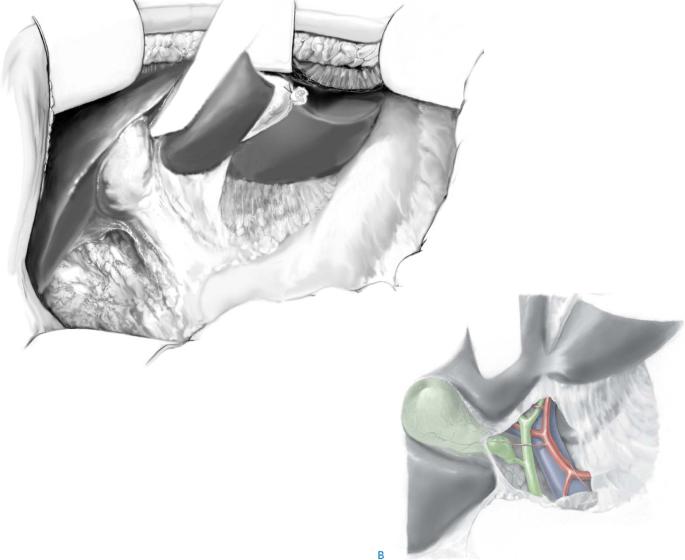
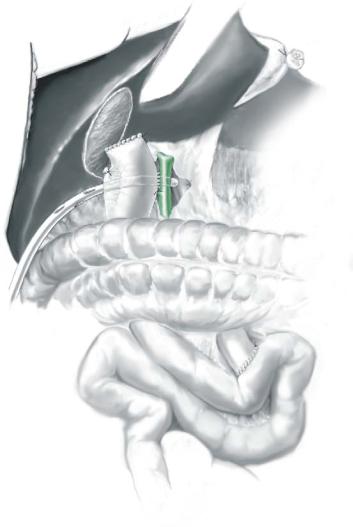
STEP 1 |
Exposure |
|
|
In first-access operations it is usually not necessary to mobilize the flexura hepatica of |
|
|
||
the colon and to mobilize the duodenum by means of a Kocher procedure; however, this may facilitate exposure. In redo operations the preferred method is to carefully perform adhesiolysis and mobilize the liver from the abdominal wall starting at the right subhepatic area. Then by gentle preparation one should follow the edge of the liver dorsally and cranially in order to reach the hilus of the liver. Stay close to the liver! After careful mobilization, a retractor (e.g., Thompson) is installed (A, B).
A
614 |
SECTION 4 |
Biliary Tract and Gallbladder |
|
|
|
STEP 2 |
Opening of the hepatoduodenal ligament |
|
|
|
|
Cholecystectomy is performed as described in the chapter “Laparoscopic Cholecystectomy, Open Cholecystectomy and Cholecystostomy.”
The hepatoduodenal ligament is divided following the cystic duct medially until its entrance in the common hepatic duct. Next is the preparation of a segment of the jejunum, 40cm distal to Treitz’s ligament, where it is divided with the TLC (Ethicon), and again 40cm distal to this point an end-to-side anastomosis is made. The blind end of the jejunum is secured with a suture and brought to the common hepatic duct through a hole made in the mesocolon. Because of the multiplicity of anatomic variations and the consequences of inadvertent injury to vascular structures, it is imperative to identify definitely the exact location of the hepatic duct and common bile duct within the hepatoduodenal ligament before any clamping or incising is done. The purpose of the procedure is to identify healthy bile duct mucosa proximal to the site of obstruction, to prepare a segment of the gastrointestinal tract, usually a Roux-en-Y loop of the jejunum, and to direct mucosa-to-mucosa anastomosis between the bile duct and the gut. A small hole (about 1–1.5cm) is made in the jejunum (usually a puncture with the diathermia is enough) and a stay suture is placed on the left lateral side.
Choledochojejunostomy and Cholecystojejunostomy |
615 |
|
|
|
|
|
Side-to-Side Anastomosis |
|
|
|
|
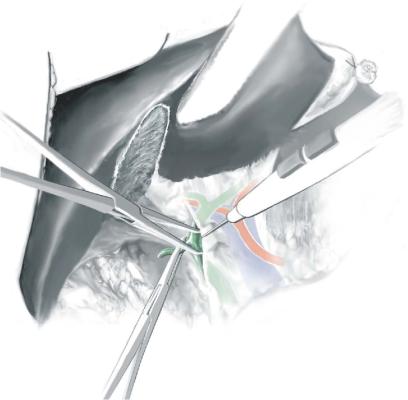
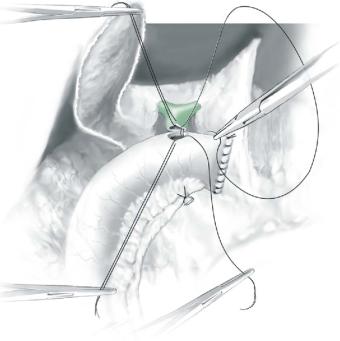
STEP 3 |
Opening of the jejunum and the choledochal duct, placement of stay sutures |
|
|
The common hepatic duct is opened and a stay suture is placed on the median side in |
|
|
|
|
order to provide a good view of both sides of the anastomosis. Then, the anastomosis is started using a long 3-0 or 4-0 PDS suture, with needles on both ends, inside-out in the common hepatic duct and outside-in through the jejunal wall. Both ends should be of equal length and a clamp should be put on one side, and the started suture used to continue suturing the dorsal part of the anastomosis. The first two to three stitches may be placed without traction (as a “parachute”), after which the jejunum is firmly pulled against the ductal wall. The suture should be guided by the assistant operator.
616 |
SECTION 4 |
Biliary Tract and Gallbladder |
|
|
|
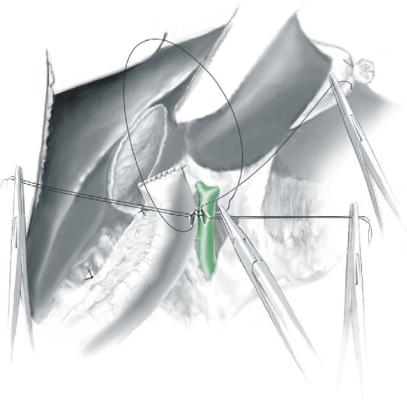
STEP 4 |
Continuous running suture of the dorsal part of the anastomosis |
|
|
|
|
A continuous running suture of the dorsal side is performed using full thickness bites of both the duct and the jejunum. With every stitch, mucosa-to-mucosa contact should be ensured using a forceps while bringing the suture to tension. Intraoperative bile leakage is not a problem. Spill from the intestines should be avoided or removed to reduce the possibility of postoperative infection, possibly leading to dehiscence of the anastomosis.
STEP 5 |
Continuous running suture of the ventral part of the anastomosis |
|
One or two sutures are made around the corner at the duodenal side of the anastomosis, |
|
|
|
after which this side of the suture is put on a clamp and the other end is used to |
|
continue the suture for the ventral part of the anastomosis from the top. At this point the |
|
stay-sutures may be removed . |
Choledochojejunostomy and Cholecystojejunostomy |
617 |
|
|
|
|
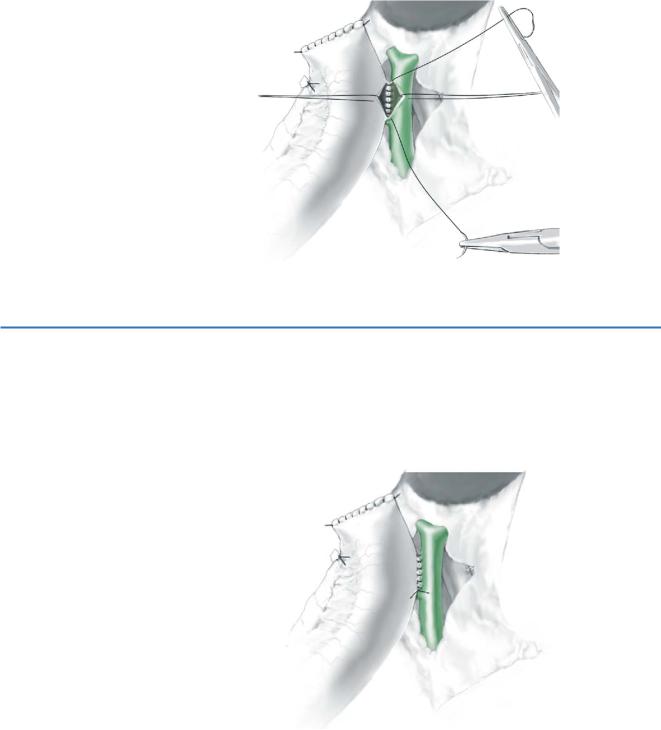
STEP 6 |
Final situation, side-to-side choledochojejunostomy |
|
|
|
|
After the anastomosis is finished, a drain is left in situ behind the anastomosis to indicate postoperative blood loss and/or bile leakage. No suction on the drain is needed.
618 |
SECTION 4 |
Biliary Tract and Gallbladder |
|
|
|
|
End-to-Side Choledochojejunostomy |
|
|
|
|
STEP 7 |
Opening of the jejunum and division of the choledochal duct, |
|
|
closure of the duodenal part; placement of stay-sutures |
|
|
|
After exploration of the hepatoduodenal ligament (Steps1 and 2, see above), the choledochal duct is cut and the duodenal side is closed using a continuous slowly resorbable monofilament suture. This is usually done in the supraduodenal part, which is about 3.5cm long; however, the middle or retroduodenal and distal or pancreatic parts of the choledochal duct are at least 2–3cm long. Stasis of pancreatic juice in this part is possible and could lead to rupture into the abdomen. If this is anticipated, the distal part should be anastomized separately during the operation or stented perior postoperatively. Damage to pancreatic tissue should be left untreated perioperatively; however, in order to protect the hepaticojejunostomy a drain should be left in place. To facilitate the making of the anastomosis, stay-sutures are placed in the ventral side of the choledochal duct as well as in the opening of the jejunal loop. The anastomosis is started using a long 3-0 PDS suture, with needles on both ends, inside-out in the jejunum and outsidein in the hepatic duct on the median side (suturing toward oneself). Both ends should be of equal length and a clamp is placed on one side and the other suture used to continue the closure of the dorsal part of the anastomosis. Again the “parachute” technique may be used (see Step3).
Choledochojejunostomy and Cholecystojejunostomy |
619 |
|
|
|
|
STEP 8 |
Continuous running suture of the dorsal part of the anastomosis |
|
|
|
|
Full thickness bites of both the duct and the jejunum should be taken while suturing. Mucosa-to-mucosa contact should be ensured with every stitch using a forceps while bringing the suture to tension. Tearing of the diseased ductus requires anastomosis on a level closer to the hilus of the liver.
STEP 9 |
Running suture of the ventral part of the anastomosis |
|
One or two sutures are made around the corner on the lateral side of the anastomosis, |
|
|
|
after which this side of the suture is put on a clamp and the other end used to continue |
|
the suture for the ventral part of the anastomosis. |

620 |
SECTION 4 |
Biliary Tract and Gallbladder |
|
|
|
|
Cholecystojejunostomy |
|
|
Facile bypass for those with distal common duct obstruction and high resection of |
|
|
cystic duct. |
|
|
|
|
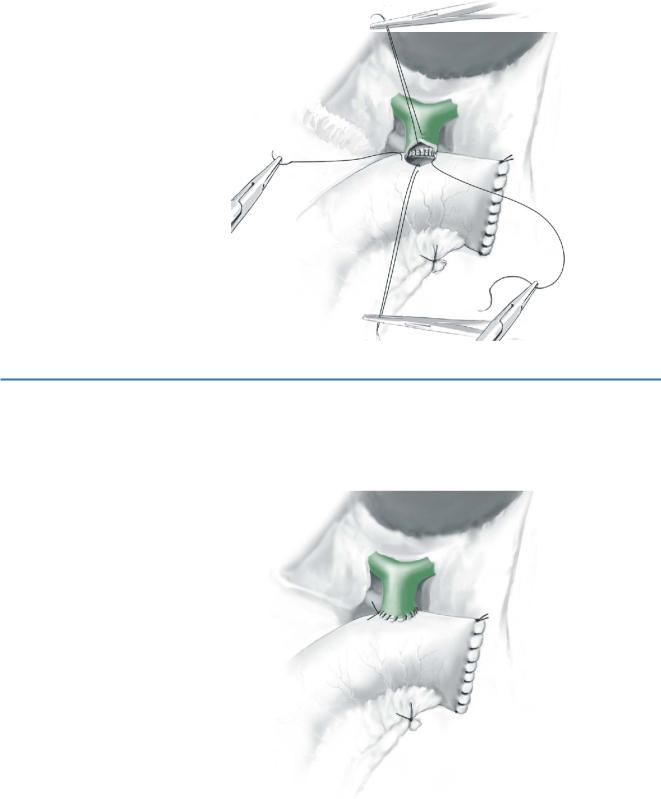
STEP 10 |
Preparation and dorsal running suture |
|
|
If obstruction in the hepatoduodenal ligament and in the distal biliary tree is such that |
|
|
||
|
the bile duct cannot be reached, a cholecystojejunostomy is performed. However, before |
|
this procedure is started, one should be certain that the cystic duct and the proximal part of the bile duct are not obstructed. Since the anatomic structures are more on the surface, this solution is an option when minimally invasive or endoscopic surgery is desirable. The gallbladder is left in situ and opened for at least 2–3cm. A jejunal loop is created as described previously and an opening of the same size is made. One should clearly identify the gallbladder and the jejunal wall, and free it from omental adhesions, in order to perform adequate through-wall stitches. A continuous running 3-0 PDS is used to anastomose the gallbladder onto the jejunum, starting on the medial side (A).
While suturing, one should take care to take full thickness bites of both the gallbladder wall and the jejunum. With every stitch, mucosa-to-mucosa contact should be ensured using a forceps while bringing the suture to tension. The size of the opening in the gallbladder as well as in the jejunum may be adjusted while making the anastomosis in order to create a perfect fit and thereby avoid postoperative leakage (B).
Choledochojejunostomy and Cholecystojejunostomy |
621 |
|
|
|
|
STEP 11 |
Completed cholecystojejunostomy |
|
|
|
|
A drain is left in situ after finishing the anastomosis, to indicate postoperative bleeding or bile leakage. If a drain is really indicated, drainage is set up as shown in Sect.1, chapter “Principles of Drainage”
Postoperative Tests
■Check daily for clinical signs of biliary obstruction (fever, icterus and pain). However, bile obstruction may be considered normal for the first few days postoperatively due to edema of the operative area.
■If an enterohepatic drain is in place, a cholangiography through the outside drain on day 5 will reveal possible leakage of the anastomosis (in case of leakage, the drain should not be removed at day 5 but should be left in place for at least another 6 weeks).
Postoperative Complications
■Bleeding usually occurs within 24hours and may require immediate reexploration and control of the bleeding after full exposure of the cause.
■If a bile leakage from the anastomosis is recognized within 24hours, a reexploration is indicated and usually can be easily restored. If bile leakage happens later, drainage is usually the treatment of choice, which may be helped by the placement of a stent in the hepaticojejunostomy with endoscopic retrograde cholangiopancreatography (ERCP). At this point a reanastomosis would lead to dehiscence or stricture. Therefore, this should be performed in an elective setting after 6–8 weeks.
■Cholangitis, which most often occurs within the first days after surgery, should be treated by antibiotics. If obvious obstruction is observed and no reoperation is considered, it should be treated by drainage through PTC or ERCP.
■A restenosis would clinically be evident by recurrent icterus and intermittent cholangitis. As the results of reoperations are poor, the placement of a stent should be considered.
■Enterocutaneous fistula (leakage from the blind end of the jejunum) should be treated in a conservative way.
■In case of pancreatitis, conservative treatment usually suffices.
■Delayed gastric emptying and/or ileus should always be taken seriously, since it may be a sign of other problems (as mentioned above) and a CT scan may be indicated. Beware of aspiration pneumonia!
