clavien_atlas_of_upper_gastrointestinal_and_hepato-pancreato-biliary_surgery2007-10-01_3540200045_springer
.pdf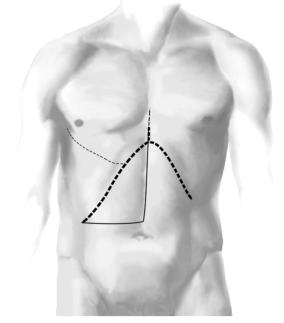
602 |
SECTION 4 |
Biliary Tract and Gallbladder |
|
|
|
|
Procedure |
|
Access and General Principles
■The incision must provide adequate access to the hilum of the liver as well as provide the ability to completely mobilize the liver if necessary.
■Potential incisions: right subcostal incision with a midline vertical extension (hockey stick), bilateral subcostal incision with or without midline vertical extension (chevron, rooftop).
■In the special case of right lobe atrophy, extension of the incision to a thoracoabdominal approach from the midpoint of the right subcostal portion up through the 7th intercostal space can be invaluable.
■Retraction with a Goligher retractor with wide blades pulling the ribs in an anterior and cephalad direction.
■Intraoperative ultrasound to determine the relationship of tumor/stricture and adequately dilated bile ducts.
■Intraperitoneal drain is placed and left for gravity drainage postoperatively.
The Ligamentum Teres Approach and Other Approaches to the Intrahepatic Ducts for Palliative Bypass |
603 |
|
|
|
|
|
Approach to the Left Hepatic Duct |
|
|
|
|
STEP 1 |
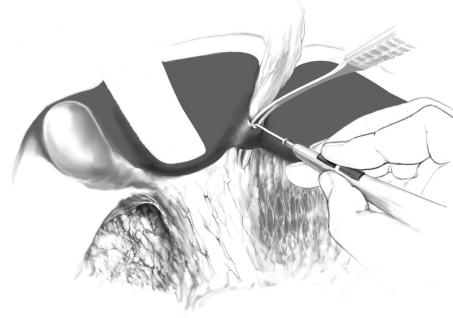
Dividing the bridge between segments 3 and 4 |
|
|
The ligamentum teres is divided and the falciform ligament is freed from the abdominal |
|
|
||
|
wall and diaphragm. A tie is left in place on the hepatic side of the ligamentum teres, |
|
|
which serves as a retractor to help elevate the liver. The bridge of liver tissue between |
|
|
the quadrate lobe (segment 4b) and the left lateral segment is divided. There are |
|
|
never major vessels in this tissue and it can be divided easily with electrocautery. |
|
This maneuver exposes the umbilical fissure completely and makes dissection at the base of segment 4 easier.
604 |
SECTION 4 |
Biliary Tract and Gallbladder |
|
|
|
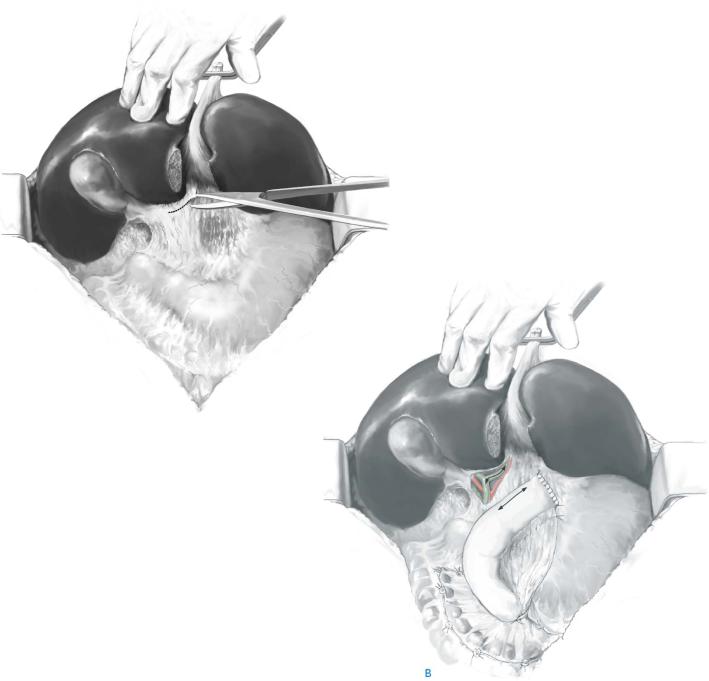
STEP 2 |
Exposing the duct |
|
|
|
|
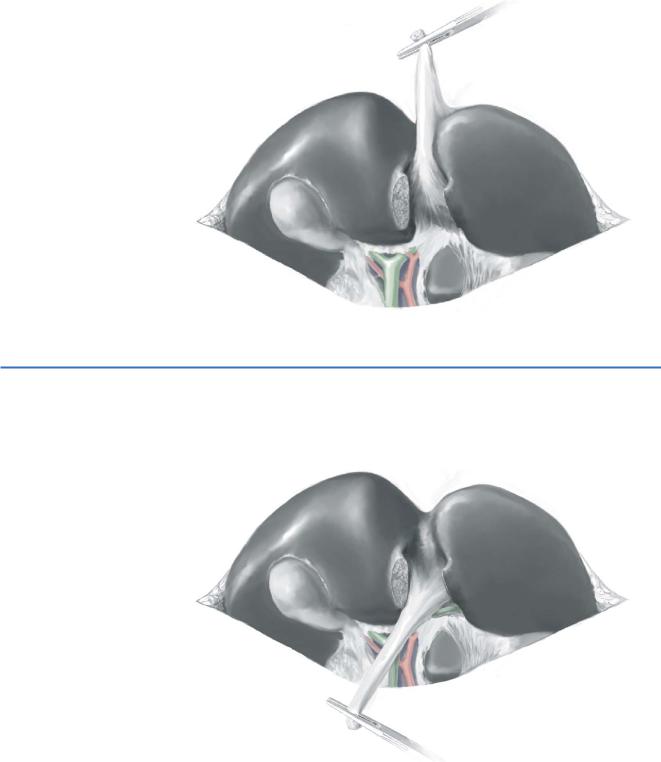
Segment 4 is elevated superiorly, exposing its base. Sharp dissection is used to dissect the plane between Glisson’s capsule and the left portal triad, thus lowering the hilar plate (A). The left hepatic duct is exposed and dissected throughout its transverse extrahepatic course at the base of segment 4 before it enters the umbilical fissure. Dissection to the right side can expose the biliary confluence and the right hepatic duct origin as well (B). Minor bleeding can occur in this area and is almost always controllable with light pressure. A thin curved retractor placed at the base of segment 4 from above can help with exposure. A large tumor in this area may make exposure difficult, mandating local excision or abandonment of this approach.
A
The Ligamentum Teres Approach and Other Approaches to the Intrahepatic Ducts for Palliative Bypass |
605 |
|
|
|
|
STEP 3 |
Biliary-enteric amastomosis |
|
|
|
|
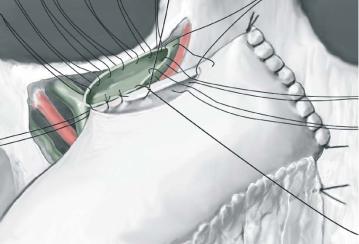
A 70-cm Roux-en-y loop of jejunum is brought up to the hilum in a retrocolic fashion and a side-to-side anastomosis is performed.
606 |
SECTION 4 |
Biliary Tract and Gallbladder |
|
|
|
|
Ligamentum Teres (Round Ligament) Approach |
|
|
(See also chapter “Intrahepatic Biliodigestive Anastomosis Without Indwelling Stent”) |
|
|
|
|
STEP 1 |
Controlling the round ligament |
|
|
The ligamentum teres is divided and the falciform ligament freed from the abdominal |
|
|
||
|
wall and diaphragm. The bridge of liver tissue between segment 4 and the left lateral |
|
|
segment is divided. |
|
STEP 2 |
Mobilizing and positioning the round ligament |
|
While holding the liver upward, the ligamentum teres is then pulled downward and its |
|
|
|
attachments to the liver are released, exposing its base. |

The Ligamentum Teres Approach and Other Approaches to the Intrahepatic Ducts for Palliative Bypass |
607 |
|
|
|
|
STEP 3 |
|
|
|
Dissection is then carried out to the left of the upper surface of the base of the liga- |
|
|
|
|
|
mentum teres. A number of small vascular branches to the left lateral segment will be |
|
|
encountered and sometimes must be ligated and divided. The main portal pedicle to |
|
|
segment 3 can usually be preserved. This dissection can be tedious and must be done |
|
|
carefully because bleeding in this area can be difficult to control. A small aneurysm |
|
|
needle can be helpful in isolating and encircling these small branches. |
|
|
|
|
STEP 4 |
Exposing the segment 3 duct |
|
|
The segment 3 duct is exposed in its position above and behind the portal vein branch. |
|
|
||
|
The duct is opened longitudinally just beyond the branching of the segment 2 and 3 |
|
|
ducts. A side-to-side hepaticojejunostomy to a 70-cm retrocolic Roux-en-Y jejunal loop |
|
|
is carried out. |
|
608 |
SECTION 4 |
Biliary Tract and Gallbladder |
|
|
|
STEP 5 |
Partial hepatectomy to facilitate exposure |
|
|
|
|
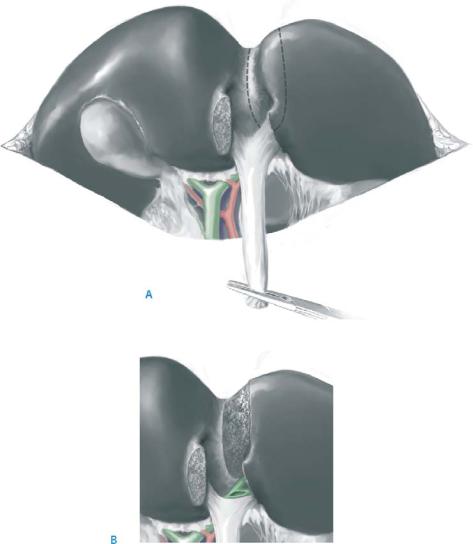
An alternative approach or a helpful adjuvant technique to expose the segment 3 duct is to split the liver just to the left of the falciform ligament superiorly (A) and to divide the tissue until the duct is reached from above (B). This can assist identification of the duct or be the primary means of approach. The added benefit of this approach is the lack of devascularization to segment 3 that is usually necessary for the dissection in the umbilical fissure.

610 |
SECTION 4 |
Biliary Tract and Gallbladder |
|
|
|
STEP 4
A side-to-side hepaticojejunostomy to a retrocolic 70-cm Roux-en-Y loop of jejunum is performed.
Postoperative Tests
■Coagulation parameters and hematocrit in the first 48hours
■Daily liver function tests
■Daily assessment of renal function
■Daily assessment of drain output for bile leakage
Postoperative Complications
■Short term:
–Bile leakage
–Biloma
–Abscess
–Liver dysfunction/liver failure
–Intra-abdominal bleeding
–Early stricture of anastomosis
■Long term:
–Recurrent benign biliary stricture
–Recurrent malignant biliary stricture
–Cholangitis
Tricks of the Senior Surgeon
■In the round ligament approach, a small branch of the portal vein passing to segment 3 usually lies immediately anterior to the segment 3 duct. This branch usually needs to be divided for adequate ductal exposure.
■Even if the malignant obstruction has isolated the left biliary tree from the right, drainage of only the left liver most often will suffice to relieve jaundice. This is particularly true if the tumor occupies predominantly the right liver and has produced right hepatic atrophy.
■Because of technical difficulties, right-sided bypasses have largely been abandoned in favor of percutaneous drainage.