
clavien_atlas_of_upper_gastrointestinal_and_hepato-pancreato-biliary_surgery2007-10-01_3540200045_springer
.pdf
Intrahepatic Biliodigestive Anastomosis
Without Indwelling Stent
William R. Jarnagin
Introduction
The technique for reestablishing continuity of the extrahepatic bile ducts to the intestinal tract is described. Multiple biliary lumen may be encountered even with minor dissection into the hepatic parenchyma. All lumens should either be anastomosed or ligated with permanent sutures.
Indications and Contraindications
Indications |
■ |
Reconstitution of biliary-enteric continuity after bile duct resection or combined |
|
|
hepatic and biliary resection for malignancy involving the proximal bile duct – |
|
|
typically hilar cholangiocarcinoma or gallbladder cancer |
|
■ |
Palliative biliary drainage for proximal biliary obstruction due to locally advanced |
|
|
malignancy |
|
■ |
Provision of durable biliary drainage in the setting of a benign stricture/injury of the |
|
|
proximal bile duct – often associated with multiple prior attempts at repair |
|
|
Elective, palliative intrahepatic biliary-enteric bypass for malignancy is best avoided |
Contraindications |
■ |
|
|
|
in the face of widespread metastatic disease, extensive intrahepatic disease or portal |
|
|
vein obstruction. |
|
■ |
Portal hypertension in patients with benign strictures is a lethal combination and |
|
|
should rarely be attempted. |
592 |
SECTION 4 |
Biliary Tract and Gallbladder |
|
|
|
|
Procedures |
|
|
General (End to Side) |
|
|
The general technique for intrahepatic (and proximal extrahepatic) biliodigestive anas- |
|
|
tomoses is shown. This technique is quite useful in all cases where access to the bile duct |
|
|
is limited by space. In such situations, approaches that might be appropriate for a |
|
|
straightforward distal bile duct anastomosis usually cannot be used. For example, one |
|
|
may be tempted to complete the posterior row as the first step, as one would in a distal |
|
|
bile duct anastomosis, only to find that completion of the anterior row is now extremely |
|
|
difficult, if not impossible, due to steric hindrance from the bowel. The technique |
|
|
described allows precise placement of sutures under direct vision, before apposition of |
|
|
the bowel and bile duct hinders access. In all cases, anastomosis is performed to a 70-cm |
|
|
retrocolic Roux-en-Y jejunal loop. Absorbable suture material (3-0 or 4-0 Vicryl or PDS) |
|
|
should be used. |
|
|
|
|
STEP 1 |
Identification of transected bile ducts |
|
|
After adequate exposure of the duct has been obtained, a tension-free jejunal loop |
|
|
||
|
is brought through the transverse mesocolon. It is imperative that the surgeon identify |
|
|
all exposed ductal orifices for inclusion in the anastomosis (see below). Failure to |
|
provide adequate drainage of all ducts often leads to serious postoperative complications, such as persistent bile leak or subhepatic abscess, biliary fistulation, lobar atrophy, cholangitis or hepatic abscess.
The jejunal limb is temporarily anchored with a stay suture at some distance from the bile duct to allow precise placement of the sutures.

Intrahepatic Biliodigestive Anastomosis Without Indwelling Stent |
593 |
|
|
|
|
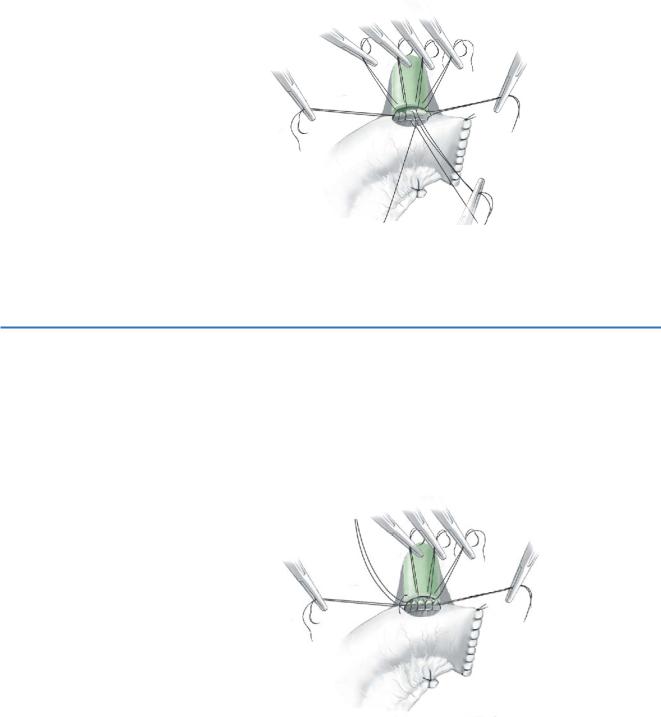
STEP 2 |
Placement of anterior stitches |
|
|
Working from left to right, the anterior row of sutures is placed on the bile duct |
|
|
|
|
|
(inside to out) (A). |
|
|
The sutures are sequentially clamped and the needles are retained. It is important |
|
|
to keep the sutures in order so that they can be easily retrieved (B). |
|
|
|
|
STEP 3 |
Placement of posterior stitches |
|
|
Once the anterior row has been placed on the bile duct, the posterior row is placed. |
|
|
|
|
Working from left to right, full-thickness sutures are placed from the jejunal limb (inside to out) to the back wall of the bile duct (outside to in) (B).
The sutures are not tied but are sequentially clamped with the needles removed. Again, it is important to keep the sutures in order.
594 |
SECTION 4 |
Biliary Tract and Gallbladder |
|
|
|
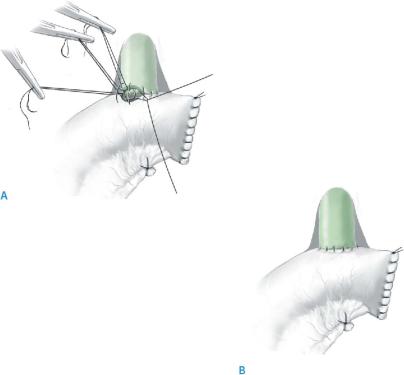
STEP 4 |
Approximating the posterior anastomosis |
|
|
|
|
The jejunal loop is then slid upward along the posterior row of sutures until the back wall of the bowel and the bile ducts are apposed.
The posterior sutures are then tied and the sutures are cut.
STEP 5 |
Completing the anterior anastomosis |
|
The previously placed sutures on the anterior wall of the bile duct are now used to |
|
|
|
complete the anastomosis. |
|
Working from right to left, the needles are passed sequentially through the anterior |
|
jejunal wall (outside to in). |
|
The sutures are not tied at this point but are sequentially clamped with the needles |
|
removed. |
Intrahepatic Biliodigestive Anastomosis Without Indwelling Stent |
595 |
|
|
|
|
STEP 6 |
Tying the anterior stitches |
|
|
|
|
The anterior layer is then completed by securing the sutures, tying from left to right (A).
The completed anastomosis is shown (B).
596 |
SECTION 4 |
Biliary Tract and Gallbladder |
|
|
|
|
Anastomosis to Multiple Ducts (End to Side) |
|
|
Resection of the biliary tree above the confluence often results in multiple disconnected |
|
|
ducts, all of which must be included in the anastomosis. Failure to do so often results in |
|
|
life-threatening complications, as described above. If possible, two or more disconnected |
|
|
duct orifices should be approximated with sutures and treated as a single duct for the |
|
|
purposes of the anastomosis. When this is not possible, the same general technique can |
|
|
be used to perform multiple simultaneous anastomoses. By placing the entire anterior |
|
|
row of sutures on all exposed ducts followed by the posterior row, as described above, |
|
|
the separated orifices are treated as if single. Interference from the jejunal limb usually |
|
|
precludes creation of a second anastomosis after the first has been completed. |
|
|
Single Anastomosis to Multiple Exposed Ducts |
|
|
|
|
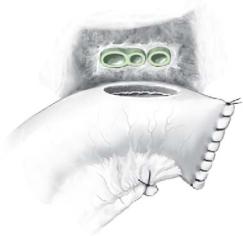
STEP 1 |
Identification of all lumens |
|
|
All exposed ducts are identified. |
|
|
|
|
Intrahepatic Biliodigestive Anastomosis Without Indwelling Stent |
597 |
|
|
|
|
STEP 2 |
Anastomosis to a single jejunal opening |
|
|
|
|
Ducts that are not connected by a septum are brought into apposition by placing two or three interrupted sutures. The complex of exposed ducts can be treated
as a single ductal orifice, and the anastomosis is created to a single jejunal opening. The anastomosis is carried out using the general technique described in “Procedures”,“General (End to Side)”.
598 |
SECTION 4 |
Biliary Tract and Gallbladder |
|
|
|
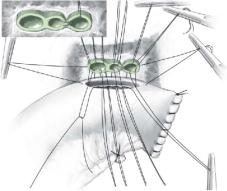
Multiple Simultaneous Anastomoses to Separated Ducts
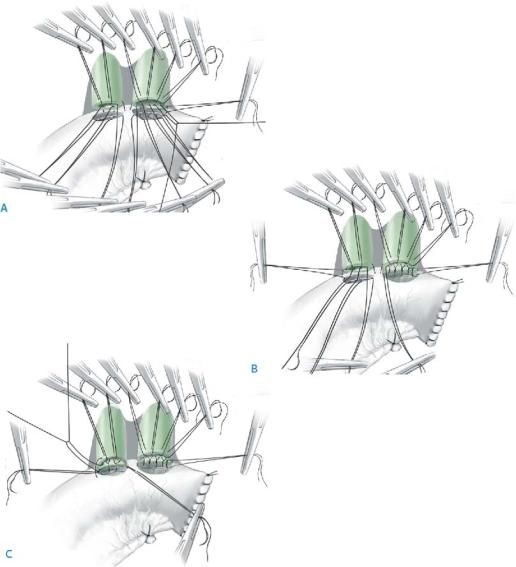
If the surgeon determines that the ductal orifices are too widely separated to create a single anastomosis, multiple simultaneous anastomoses will be required, using the same general approach as described in “Procedures”,“General (End to Side)”. Working from left to right, the anterior row of sutures is placed on all exposed bile ducts (inside to out). The sutures are sequentially clamped and the needles are retained, keeping the sutures in order so that they can be easily retrieved (A).
The jejunal loop is then slid upward along the posterior row of sutures until the back wall of the bowel and the bile ducts are apposed, making sure that the jejunal openings are properly aligned to the respective ductal orifices. The posterior sutures are then tied and the sutures are cut (B).
The previously placed sutures on the anterior wall of the bile duct are now used to complete the anastomosis, as in “Procedures”,“General (End to Side)”, making certain that the ductal sutures are correctly placed to the corresponding jejunal opening (C).
Intrahepatic Biliodigestive Anastomosis Without Indwelling Stent |
599 |
|
|
Side-to-Side Intrahepatic Anastomosis
Side to side intrahepatic biliary-enteric anastomoses are generally undertaken for palliative biliary drainage in patients with unresectable cancer, most commonly hilar cholangiocarcinoma or gallbladder cancer; they are much less frequently used in cases of benign strictures/bile duct injuries. The most common approaches are to use the segment 3 duct or the right anterior sectoral duct. Techniques have been described for exposing the segment 5 duct at the base of the gallbladder fossa, although this is difficult and rarely used. The anastomotic technique used is identical to that described in “Procedures”,“General (End to Side)” above. There are several general points worth emphasizing regarding these approaches:
■In patients with advanced cancer, the right and left ductal systems are often isolated. Decompression of the right or left side alone will result in normalization of the serum bilirubin if at least 30% of the functional hepatic parenchyma is adequately drained.
■A bypass created to a lobe with ipsilateral portal vein occlusion or gross atrophy is doomed to failure and should be avoided.
■If the right and left ductal systems are isolated, the contralateral side will not be adequately drained. In patients with advanced malignancy, this is acceptable, provided that the contralateral biliary tree has not been contaminated (i.e., prior instrumentation). If this is the case, interventional radiologists may be able to place an internal wall stent from left to right (or right to left), allowing decompression of the contralateral system through the bypass; if not, the patient will require
a permanent external biliary drain.
■For benign strictures, unlike palliative bypass for malignancy, intrahepatic bypass approaches require continuity at the hilus so that complete biliary decompression is achieved.
Tricks of the Senior Surgeon
■When multiple ducts are encountered, it is particularly important to find the open caudate ducts. If these are left without anastomoses to the intestinal tract, a chronic fistula may occur.
■If a small open duct is encountered that is too small for anastomosis, ligation with a non absorbable suture is the most expedient solution.

The Ligamentum Teres Approach and Other Approaches to the Intrahepatic Ducts for Palliative Bypass
Michael D’Angelica
Introduction
When the hilus of the liver is not accessible for decompression of obstructive jaundice, use of intrahepatic ducts for surgical bypass is a safe and effective technique as originally described by Bismuth and Corlette in 1975 and later by Blumgart and Kelly in 1984. The general principle is to identify intrahepatic healthy bile duct mucosa proximal to a point of biliary obstruction and to create a mucosa-to-mucosa anastomosis to a long Roux-en-y loop of jejunum. Anastomosis should provide biliary drainage and relief of symptoms such as jaundice and pruritis.
Indications and Contraindications
Indications |
■ |
Malignant obstruction (most commonly gallbladder carcinoma and hilar |
|
|
cholangiocarcinoma) of the biliary confluence when access to the common hepatic |
|
|
duct is not possible |
|
■ |
Life expectancy greater than 6months |
|
■ |
Extensive benign stricture involving the biliary confluence when access to the |
|
|
common hepatic duct is not possible |
|
■ |
Complete obliteration of the biliary confluence and consequent disconnection |
|
|
of the right from the left liver is not a contraindication |
|
|
Lack of safe access to healthy bile duct mucosa for an adequate anastomosis |
Exclusion Criteria |
■ |
|
|
■ |
Bypass to a portion of liver that is atrophied or fibrotic |
Investigation/Preparation
Clinical: |
Signs and symptoms of cholangitis, cirrhosis and portal hyper- |
|
tension |
Laboratory: |
Liver function tests, nutritional parameters, clotting parameters, |
|
renal function |
Radiology: |
Duplex ultrasound, magnetic resonance cholangiopancreatography |
|
(MRCP); consider direct cholangiography (percutaneous trans- |
|
hepatic) with or without preoperative stenting |
Preparation: |
Bowel preparation, perioperative broad-spectrum antibiotics, |
|
adequate treatment of cholangitis with drainage and antibiotics |
