
clavien_atlas_of_upper_gastrointestinal_and_hepato-pancreato-biliary_surgery2007-10-01_3540200045_springer
.pdf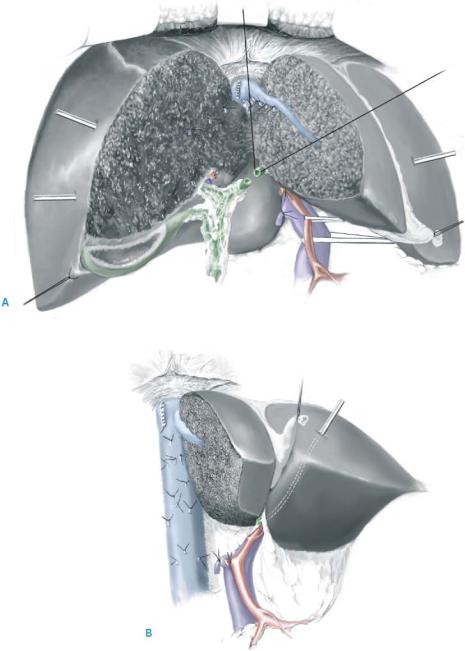
580 |
SECTION 4 |
Biliary Tract and Gallbladder |
|
|
|
STEP 10 |
Intrahepatic bile duct resection |
|
|
|
|
The left intrahepatic bile duct is identified at the right edge of Rex’s recess. Two stay sutures are placed ventrally and dorsally (A), the left hepatic duct is transected perpendicularly, and the right liver, caudate lobe and extrahepatic bile duct are removed (B). At the ventral edge of the resected margin of the left hepatic duct, the bile duct of segment 4 is opened followed by the segments 2 and 3 dorsally.
Bile Duct Resection |
581 |
|
|
STEP 11 |
|
|
Extended lymph node dissection is performed as above. |
|
|
|
|
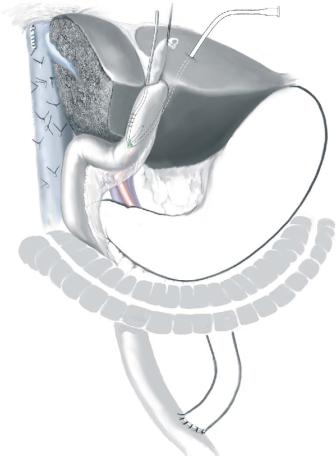
STEP 12 |
Biliary reconstructions |
|
A Roux-en-Y jejunal loop is lifted through the shortest route: the retrocolic route. |
|
|
|
A jejunostomy tube is also introduced from the proximal edge of the jejunal limb |
|
before hepaticojejunostomy. |
582 |
SECTION 4 |
Biliary Tract and Gallbladder |
|
|
|
|
|
|
Postoperative Tests |
|
|
|
■ |
Postoperative surveillance in an intensive or intermediate care unit |
|
|
■ |
Liver function test (bilirubin, ALT, AST, albumin), coagulation parameters, |
|
|
|
hemoglobin, red blood cell (RBC), withe blood cell (WBC), CRP |
|
|
■ |
Color Doppler ultrasound to estimate the blood flow of the portal vein and hepatic |
|
|
|
artery |
|
Local Postoperative Complications
■Short term:
–(Pleural effusion)
–Wound infection
–Bile leak from hepaticojejunostomy or raw surface of the liver
–Subphrenic or subhepatic abscess
–Intra-abdominal bleeding
–Liver failure
–Portal vein thrombosis
■Long term:
–Cholangitis
–Anastomotic stricture
–Chronic liver failure
Tricks of the Senior Surgeon
■Check the intraoperative external biliary drainage to prevent unexpected biliary congestion from which septic complications may develop.
■Suture the large short hepatic veins or caudate lobe veins in detaching the caudate lobe from the vena cava.
■Check the CVP in the monitor before liver transection. If the CVP is higher than 3cm H2O, do not start to transect the liver.
■The hepatic vein on the liver side should be closed by a running suture to prevent bleeding during the handling of the liver.
■Stay sutures should be placed before dividing the intrahepatic bile duct, otherwise the small segmental duct will slip away and be hidden by the liver parenchyma.
■The lymphatic vessels should be tied in a para-aortic lymph node dissection to prevent postoperative massive lymphorrhea.
Bile Duct Resection |
583 |
|
|
Editor’s Comments
■Tissue diagnosis is not a prerequisite for surgical resection of suspected cholangiocarcinoma – clinical presentation and radiographic appearance is enough.
■ERCP and peroral cholangioscopy are avoided for high bile duct obstruction since these are unlikely to define the problems or palliate obstruction, and can lead to cholangitis.
■Percutaneous drainage is not always necessary prior to surgery. The patients who will benefit from preoperative drainage are those who (1) have cholangitis, (2) have renal dysfunction, (3) have possible vascular invasion on the side that will be the remnant liver after resection or (4) should undergo portal vein embolization.
■In mobilizing the candidate lobe for a patient who will be subjected to a left lobectomy and caudate resection, it is usually safest to mobilize the caudate from the right to the left. Only in the thinnest patients is it safe to perform the mobilization from the left.
■Some surgeons believe that caudate resection is an essential part of every resection for hilar cholangiocarcinoma, while others believe that resecting this portion of the liver is indicated only when the caudate lobe is directly involved by tumor.
Resection of the Mid Common Bile Duct
Chandrajit P. Raut, Jean-Nicolas Vauthey
Introduction
True mid bile duct tumors are very rare. Most patients with mid bile duct obstruction should be considered to have gallbladder cancer until proven otherwise. Mid bile duct resections are usually performed for the rare mid duct cholangiocarcinomas or for patients with early gallbladder cancer and tumor at the cystic duct margin.
Indications and Contraindications
Indications |
■ |
Diagnosis of biliary strictures without confirmed malignancy |
|
■ |
Diagnosis of suspected benign disease |
|
■ |
Confirmed malignant disease confined to mid common bile duct (CBD) in patients |
|
|
unfit for more extensive resection (pancreaticoduodenectomy or liver resection) |
|
|
Malignant disease involving biliary confluence (hilar cholangiocarcinoma) |
Contraindications |
■ |
|
|
■ |
Vascular invasion involving the main trunk of the portal vein or the proper hepatic |
|
|
artery |
|
■ |
Bilateral vascular involvement of hepatic arterial and/or portal venous branches |
Preoperative Investigation and Preparation for the Procedure
History: |
Alcohol intake, cholelithiasis, choledocholithiasis, primary |
|
sclerosing cholangitis/ulcerative colitis, choledochal cysts, |
|
Caroli’s disease, recurrent pyogenic cholangiohepatitis, biliary |
parasites, exposure to chemical carcinogens
Clinical evaluation: Jaundice (90–98% of patients), weight loss (51%), abdominal pain
|
(45%), fever (20%) |
Laboratory tests: |
Alkaline phosphatase, g-glutamyl transpeptidase, ALT, AST, coagu- |
|
lation parameters |
|
Assess intraand extrahepatic biliary obstruction, presence of |
|
gallstones, tumor extension, vascular involvement |
CT scan, |
Identify metastases, define relationship between tumor mass |
CT angiography |
(if detectable) and liver, assess lobar atrophy or compensatory |
or MRI: |
hypertrophy, hepatic arterial anatomy |
PTC/ERCP/MRCP: |
Delineate proximal extent of tumor, number of tumors |
|
(10% of cases will have multiple tumors) |
Cytology: |
Percutaneous catheter drainage (positive in 47% of cases), |
|
fine needle aspiration (sensitivity 77%), endoscopic transpapillary |
|
biopsy, ERCP brushing |
586 |
SECTION 4 |
Biliary Tract and Gallbladder |
|
|
|
|
Procedure |
|
|
|
|
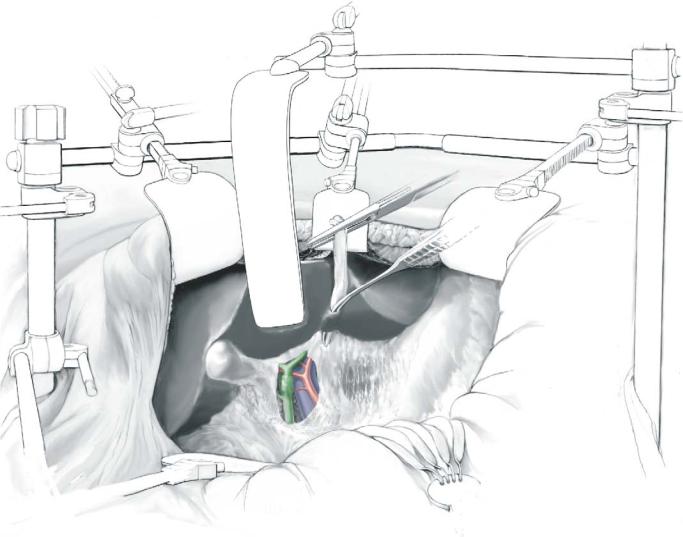
STEP 1 |
Exposure and exploration |
|
|
The abdomen is explored through a bilateral subcostal incision. Retraction is main- |
|
|
||
|
tained with broad blade retractors from a fixed support, elevating the costal margin. |
|
|
A soft retractor blade (malleable) may be inserted from above to retract segment 4. |
|
|
The ligamentum teres is divided, and the falciform ligament is separated from the ante- |
|
|
rior abdominal wall. Cephalad traction on the ligamentum teres provides additional |
|
exposure of the undersurface of the liver. If present, the bridge of liver parenchyma between segment 4 and the left lateral bisegment is divided with electrocautery; bleeding is easily controlled as this tissue rarely contains large vessels. This maneuver exposes the umbilical fissure for a later step.
Resection of the Mid Common Bile Duct |
587 |
|
|
|
|
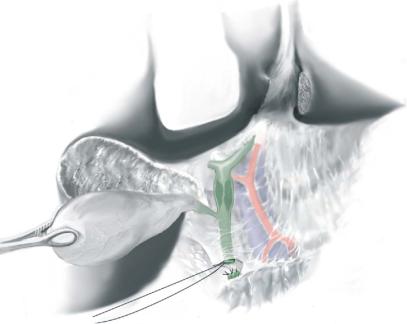
STEP 2 |
Division of the distal CBD |
|
|
|
|
The gallbladder, if present, is dissected free from its liver bed. The proximal CBD and the right and left hepatic ducts are dilated proximal to the stricture, unless stenting across the stricture has drained the obstruction. The distal CBD is isolated and divided early in the dissection above the superior edge of the pancreas and a frozen section analysis of the margin is obtained. The distal CBD stump is ligated in a figure-of-eight fashion with 4-0 PDS suture on an SH needle.

588 |
SECTION 4 |
Biliary Tract and Gallbladder |
|
|
|
STEP 3 |
Division of the proximal CBD |
|
|
|
|
The CBD, gallbladder and hepatoduodenal lymph nodes are reflected superiorly en bloc, exposing the hilar vessels and confirming resectability. Dissection is continued between the tumor anteriorly and the hepatic artery posteriorly. The hilar plate is lowered by dividing the peritoneal reflection at the base of segment 4 and the umbilical fissure is opened to expose the extrahepatic left bile duct (A). As this exposure is extended to the left, a branch of the portal vein or hepatic artery to segment 4 may be encountered and should be preserved. This exposure allows the base of segment 4 to be elevated; the malleable blade retracting the quadrate lobe may be repositioned. The proximal duct is transected at the confluence of the right and left hepatic ducts, and the specimen is marked for orientation. Additional duct margins are submitted for intraoperative microscopic frozen section examination. The opening in the proximal duct at the site of transection can be extended into the extrahepatic left bile duct sharply using Pott’s scissors (B).
If the proximal bile duct is dilated, there may be no need to lower the hilar plate or extend the incision to the left hepatic duct – Y.F.
Resection of the Mid Common Bile Duct |
589 |
|
|
|
|
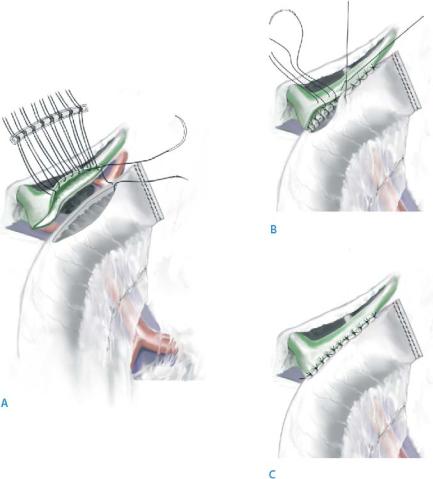
STEP 4 |
Hepp-Couinaud reconstruction |
|
|
|
|
The biliary-enteric continuity is restored with a side-to-side retrocolic Roux-en-Y hepaticojejunostomy with a single layer of interrupted, absorbable sutures (5-0 PDS vs. an shRVI needle as preferred by the authors). This technique incorporates the extrahepatic portion of the left duct in the anastomosis, as first described by Hepp and Couinaud, thus creating a wide side-to-side hepaticojejunostomy. A 70-cm jejunal Roux-en-Y limb is prepared and brought through the transverse mesocolon to the right of the middle colic artery; the stapled end does not need to be oversewn. Both the left duct and the jejunum are incised longitudinally for a 2-cm-wide anastomosis. The anterior row of No.5-0 absorbable sutures is brought through the bile duct wall and the needles are left intact (A). A Gabbay-Fisher suture guide (Genzyme Co., Fall River, MA) facilitates the management of these free sutures by organizing them; each guide holds up to 16 sutures. Gentle retraction on these sutures superiorly allows exposure of the posterior edge of the ductal incision. Precise mucosa-to-mucosa anastomosis is established with interrupted No.5-0 absorbable sutures between the posterior edge of the ductal incision and the posterior edge of the jejunal incision. The posterior sutures are tied with the knots on the inside (B). The anterior stay sutures are then placed through the jejunum to complete the anterior row of sutures. These are tied such that the knots are exterior (C). Internal stenting is not required. A drain on bulb suction is left near the anastomosis and brought through the abdominal wall in the right upper quadrant.
590 |
SECTION 4 |
Biliary Tract and Gallbladder |
|
|
|
|
|
|
Local Postoperative Complications |
|
|
|
■ |
Short term: |
|
|
|
– Bile leak |
|
|
■ |
Long term: |
|
|
|
– Cholangitis (rare) |
|
Tricks of the Senior Surgeon
■Preoperative biliary drainage with a transtumoral catheter may be of technical assistance for the hilar dissection and biliary enteric anastomosis, but does not reduce perioperative morbidity or duration of hospitalization. Drainage is only indicated in patients with sepsis and cholangitis.
■If present, the bridge of liver parenchyma between segment 4 and the left lateral bisegment is divided by electrocautery.
■Duct margins should be submitted for intraoperative frozen section analysis.
■A Gabbay-Fisher suture guide facilitates the management of these free sutures by organizing them to minimize entanglement; each guide holds up to 16 sutures.
■Internal stenting is not required.
■Resection and reconstruction utilizing the Hepp-Couinaud approach, which employs a wide mucosa-to-mucosa anastomosis extended to the left hepatic duct, has the advantage over an end-to-side anastomosis of having a lower rate of stricturing.
