
clavien_atlas_of_upper_gastrointestinal_and_hepato-pancreato-biliary_surgery2007-10-01_3540200045_springer
.pdf
560 |
SECTION 4 |
Biliary Tract and Gallbladder |
|
|
|
|
|
STEP 4 |
Stone clearance assessment |
|
|
|
■ |
Is performed only by the use of a flexible choledochoscope through the choledo- |
|
|
|||
|
|
chotomy. In this setting, a complete assessment of the lower and upper biliary tract |
|
|
|
is easily possible, up to the intrahepatic bile ducts (A-1, A-2). |
|
|
■ |
In case of residual CBDs, endoscopic stone extraction can be performed under |
|
|
|
visual control. |
|
Exploration of the Common Bile Duct:The Laparoscopic Approach |
561 |
||
|
|
|
|
STEP 5 |
Suture of the choledochotomy |
|
|
|
■ |
Closure of the choledochotomy is performed by using interrupted or continuous |
|
|
|
||
|
|
suture with resorbable 4-0 or 5-0 stitches. |
|
|
■ |
The use of resorbable or nonresorbable clips to block a continuous suture of the |
|
|
|
choledochotomy is contraindicated, to avoid further intraductal clip migration. |
|
|
■ |
At the end of the suturing, a water-tightness test is employed by blowing the CBD |
|
|
|
through the TC cholangiographic catheter, before clipping the CD or through the T-tube. |
|
|
|
|
|
STEP 6 |
CBD drainage |
|
|
|
Several options can be used, including primary closure of the CBD (see Step5), |
|
|
|
|
||
|
external biliary drainage (by a TC drain or a T-tube) or internal drainage (using an |
|
|
|
endoprosthesis). |
|
|
■Primary CBD closure: is used when there is no doubt about the complete CBD vacuity, in the absence of severe cholangitis and when papillary obstruction is absent (permeable sphincter of Oddi, absence of edema due to transpapillary instrumental maneuvers, etc.).
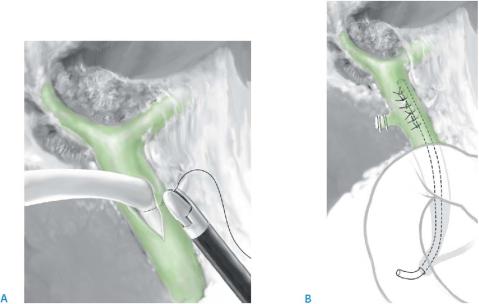
■External biliary drainage: by using a transcystic drain (see TCBDE) or a T-tube. In case of T-tube placement, the tube is fenestrated and then inserted into the CBD through the choledochotomy. The CBD suture is started after having pushed the tube at the upper corner of the choledochotomy (A). Then the T-tube is exteriorized through the site of the fifth trocar.
■Internal biliary drainage using an endoprosthesis:
–Indication: When the number of CBDs is limited, the stone clearance is accurate and in the absence of pancreatitis or Oddi dysfunction.
–Technique: The endoprosthesis is pushed under fluoroscopic guidance on
a guidewire into the CBD and through the papilla into the duodenum. Adequate transpapillary positioning is assessed by transcystic cholangiography at the end of the procedure (B).
– The endoprosthesis is removed 3weeks later by a standard duodenoscopy.
562 |
SECTION 4 |
Biliary Tract and Gallbladder |
|
|
|
STEP 7
Perform control cholangiography at the end of the procedure to detect biliary leak or transcystic drain or T-tube misplacement.
STEP 8
Routine peritoneal drainage is used.
Postoperative Tests
■Clinical assessment
■Check biliary drains
■Laboratory tests: liver function tests, pancreatic enzymes
■Control cholangiography at postoperative days 2–3 (before hospital discharge) if a TC or a T-tube drain is in place, to exclude a residual CBDS or a biliary leak
Postoperative Complications
Local Complications
■Residual CBDS
■Bile leak
■Hemorrhage
■Subhepatic abscess
■Late biliary stricture
Due to External Biliary Drain
■Patient discomfort
■Electrolyte abnormalities
■Postradiologic cholangitis
■Tube obstruction
■Accidental tube removal
■Wound infection
■Bile peritonitis at extraction
Tricks of the Senior Surgeon
■Look carefully at pictures of IOC to decide the optimal strategy for CBDE;
this will save operative time and decrease possible instrumental complications.
■Use soft, atraumatic instruments in the CBD and perform instrumental TCBDE under fluoroscopic guidance, to avoid CBD injury.
■When the suture of choledochotomy is completed, use a water-tightness test by blowing up the CBD with saline solution or methylene blue through a transcystic cholangiographic catheter or drain or through the T-tube.
■In case of failure of CBDE, postoperative endoscopic sphincterotomy can be planned. In these circumstances, placement of a transcystic biliary drain will optimize the success rate of the further endoscopic procedure.

Exploration of the Common Bile Duct:The Laparoscopic Approach |
563 |
|
|
Exploration of the Common Bile Duct:
The Open Approach
Introduction
The first choledochotomy through laparotomy was reported by Kehr in 1896 and was the surgical treatment of choice for many years. However, since the 1990s, the open approach has been increasingly abandoned in favor of the laparoscopic procedure for CBDE.
Indications and Contraindications
Indications |
■ |
After conversion to open cholecystectomy |
|
■ |
When laparoscopic and endoscopic expertise is not available |
Contraindications, Preoperative Investigations, Postoperative Tests and Postoperative Complications
These are similar to those for LCBDE.
Procedure
Incision and Exposure
Right subcostal or upper middle-line incision. The hepatoduodenal ligament is more easily stretched than for LCBDE, by pulling up the quadrate lobe using a retractor and pulling down the pancreatic head by using the assisting surgeon’s hand.
564 |
SECTION 4 |
Biliary Tract and Gallbladder |
|
|
|
Choledochotomy
Indications and techniques, including methods of stone extraction and stone clearance assessment, are similar to those for laparoscopic CBDE. However, external biliary drainage is classically used during open CBDE (OCBDE), by using either a TC drain or more often a T-tube. However, primary closure of the CBD might be indicated under the same conditions as for LCBDE. Internal biliary drainage is usually not reported during OCBDE.
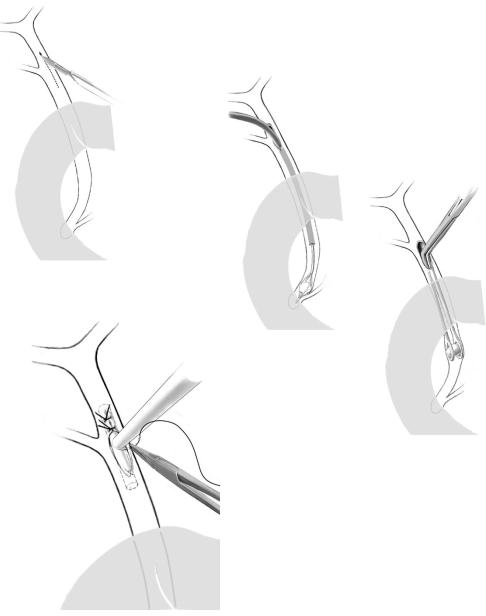
■Stay sutures are placed on the CBD on either side of the planned choledochotomy, and the CBD is openedless (A).
■The common duct stone is then extracted either by choledochoscopy (B-1) or by use of stone forceps (B-2).
■The CBD is then closed over a T-tube (C).
A
B-1
B-2
C
Bile Duct Resection
Yuji Nimura
Introduction
Resection of tumors at the bifurcation of the left and right hepatic duct requires one of the most difficult operations. The surgical procedure requires not only a portal
lymphadenectomy and bile duct resection, but almost always a liver resection. The goals of this operation are: (1) resection of the primary tumor, (2) resection of the lymphatic drainage of the liver and (3) reestablishment of biliary continuity.
Indications and Contraindications
Indications |
■ |
Primary malignancies (e.g., intrahepatic cholangiocarcinoma involving the hepatic |
|
|
hilus, hilar cholangiocarcinoma, gallbladder carcinoma involving the hepatic hilus, |
|
|
diffuse carcinoma of the extrahepatic bile duct) |
|
■ |
Benign diseases (e.g., primary sclerosing cholangitis, inflammatory pseudotumor) |
|
■ |
Traumatic lesion at the hepatic hilus |
Absolute Contraindications ■ Biliary carcinoma with distant organ metastasis (liver, lung, bone, peritoneum)
■Uncontrollable severe cholangitis with or without sepsis
■Poor liver reserve with prolonged cholestasis
■Severe coagulopathy despite vitamin K administration
Relative Contraindication |
■ Locally advanced cholangiocarcinoma with bilateral hepatic arterial encasement |
566 |
SECTION 4 |
Biliary Tract and Gallbladder |
|
|
|
|
Preoperative Investigation and Preparation for the Procedure |
|
|
History: |
Biliary surgery |
|
Clinical evaluation: |
Jaundice, cholangitis, nutritional status |
|
Laboratory tests: |
Bilirubin, alkaline phosphatase, ALT, AST, albumin, coagulation |
|
|
parameters (prothrombin time, platelets), indocyanin green test, |
|
|
tumor markers carbohydrate antigen 19–9 (CA19–9) and car- |
|
|
cinoembryonic antigen (CEA) |
|
Radiology: |
Ultrasonography, cholangiography (PTC, ERCP, MRCP), 3D CT |
|
|
(angiography), CT volumetry |
|
Endoscopy: |
Peroral cholangioscopy, percutaneous transhepatic cholangioscopy. |
|
|
The above procedures should be performed to make a differential |
|
|
diagnosis or to define the intraductal spread of cancer by taking a |
|
|
biopsy. |
What we should not do
A metallic stent should not be used in resectable biliary carcinoma.
Preparation Prior to Surgery
■Antibiotics sensitive to bile culture
■Percutaneous transhepatic biliary drainage (endoscopic biliary drainage is not advisable)
■Portal vein embolization for major hepatectomy
■Internal biliary drainage or bile replacement through a nasogastric tube for patients with external biliary drainage
Bile Duct Resection |
567 |
|
|
|
Procedure |
|
Access |
|
Incision, division of round and falciform ligament (see Sect.1, chapters “Positioning |
|
and Accesses” and “Retractors and Principles of Exposure”). |
|
|
STEP 1 |
|
|
Exposure and exploration: installation of the retractor (see Sect.1, chapter “Retractors |
|
|
|
and Principles of Exposure”) and inspection of possible peritoneal metastasis. |
|
Percutaneous transhepatic biliary drainage (PTBD) catheters are moved to the opera- |
|
tive field to maintain intraoperative biliary drainage. |
|
Ultrasound to evaluate location of the tumor in relation to vascular structures |
|
(portal vein, hepatic artery, hepatic vein). |
|
Careful inspection of vascular variation. |
|
|
STEP 2 |
Regional lymph node and connective tissue dissection |
|
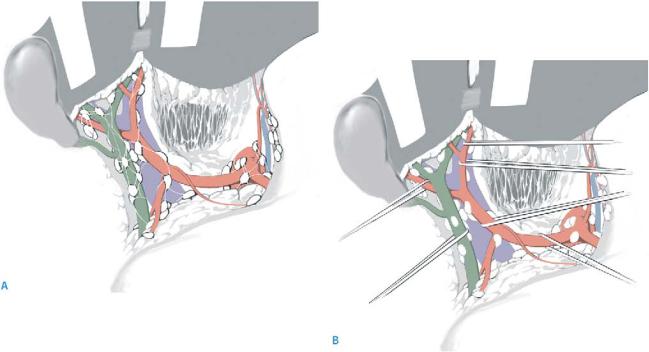
Lymph nodes in the hepatoduodenal ligament (No.12), along the common hepatic |
|
|
|
(No.8) and celiac arteries (No.9) and retropancreatic nodes (No.13), should be dissected |
|
(A) while placing a vessel loop around the common, proper, right, middle and left |
|
hepatic arteries and common bile duct (B). |
|
Nerve plexuses around the hepatic artery should be dissected. |
|
Confirmation of vascular variation. |

568 |
SECTION 4 |
Biliary Tract and Gallbladder |
|
|
|
STEP 3 |
Distal bile duct resection |
|
|
|
|
The Kocher maneuver is performed to mobilize the duodenum and allow dissection of the distal bile duct. The distal bile duct is dissected down to the head of the pancreas and divided above the pancreas. The resection margin must be examined by frozen section.
In some cases this procedure should be advanced more distally to detach the bile duct from the pancreatic tissue and resect the duct in the pancreas with a free margin.

Bile Duct Resection |
569 |
|
|
STEP 4 |
Skeletonization of the upper part of the hepatoduodenal ligament |
|
The transected distal bile duct is pulled up and the distal portion of the hepatic artery |
|
|
|
and portal bifurcation exposed (A). After dividing the caudate lobe branches of the |
|
portal vein (A), the right and left portal veins are encircled by a vessel loop (B). |
