
clavien_atlas_of_upper_gastrointestinal_and_hepato-pancreato-biliary_surgery2007-10-01_3540200045_springer
.pdf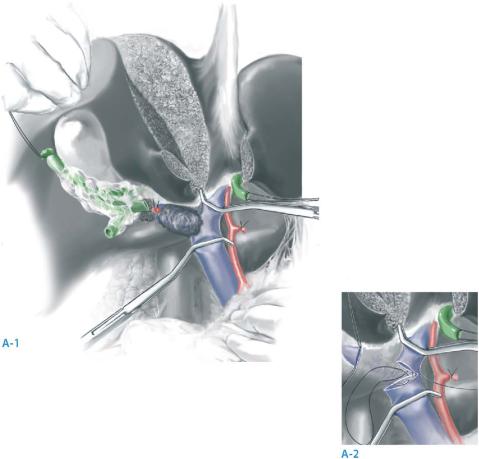
550 |
SECTION 4 |
Biliary Tract and Gallbladder |
|
|
|
STEP 9 |
Portal vein reconstruction |
|
|
|
|
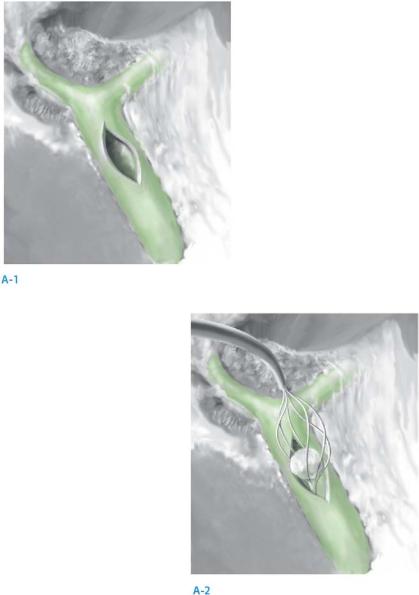
Tumors that occupy the neck of the gallbladder or the cystic duct often invade into the right portal vein or the main portal vein. Patients presenting with jaundice are at particularly high risk for portal invasion. If the left portal vein and artery are free of tumor, these vascularly invasive tumors may often be resectable by combined extended lobectomy, portal lymphadenectomy, and portal vein resection and reconstruction.
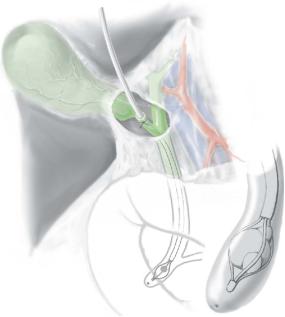
Splitting the liver along the umbilical fissure, on the line of the extended lobectomy, provides access to the hilar area and allows for easier control of the portal vein and safer reconstruction. After cutting the left hepatic duct, this duct is reflected to the patient’s left. The right hepatic artery is then transected to allow for unobstructed access to the portal vein. Vascular clamps are then placed on the main portal vein and the left portal vein (A-1). After transection, anastomosis of the main and left portal vein is accomplished with a running, nonabsorbable suture (e.g., 5-0 Proline) (A-2).
Resection of Gallbladder Cancer, Including Surgical Staging |
551 |
|
|
|
|
STEP 10 |
Liver resection and biliary reconstruction |
|
|
|
|
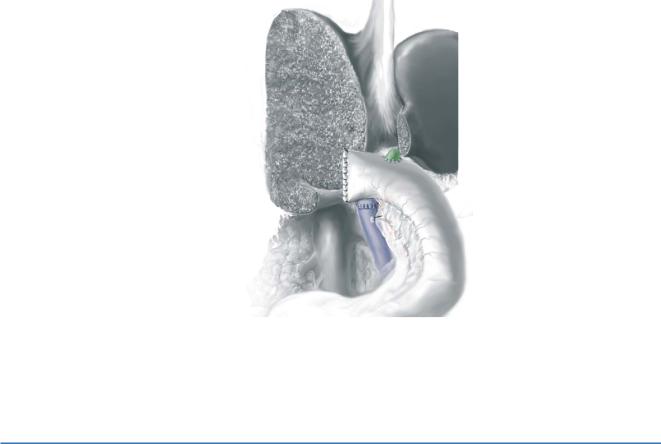
An extended right hepatic resection is then performed as described in Sect.3, chapter “Extended Hemihepatectomies.” The figure illustrates the subsequent reconstruction utilizing a retrocolic Roux-en-Y hepaticojejunostomy.
STEP 11 |
Drainage after reconstruction |
|
After completing hemostasis in the surgical field, closed drains are placed in the right |
|
|
|
upper quadrant near the biliary anastomosis. If a percutaneous transhepatic stent has |
|
been removed, a drain should also be placed near the site of the stent entry site on the |
|
liver surface. We do not usually use stents for the anastomosis. Nasogastric tube decom- |
|
pression of the gastrointestinal tract is usually continued until return of bowel function. |
|
This is particularly important if the bile duct used for anastomosis is small. Nasogastric |
|
decompression prevents swelling of the Roux-en-Y limb and possible disruption of the |
|
anastomosis. |
552 |
SECTION 4 |
Biliary Tract and Gallbladder |
|
|
|
|
|
|
Postoperative Tests |
|
|
|
■ |
Postoperative surveillance in an intensive or intermediate care unit |
|
|
|
(for extended procedures) |
|
|
■ |
Coagulation parameters and hemoglobin for at least 48hours |
|
|
■ |
Liver function test and electrolytes (including phosphorus) for at least 48hours |
|
Postoperative Complications
■General:
–Pleural effusion
–Pneumonia
–Deep vein thrombosis
–Pulmonary embolism
■Abdominal:
–Intra-abdominal bleeding
–Infected collection/abscess
–Liver failure (extended procedures)
–Bile leak with biloma formation
–Leakage of biliodigestive anastomosis (procedures with common bile duct resection)
–Portal vein thrombosis
Tricks of the Senior Surgeon
■If the patient presents with a radiologic T3 or T4 gallbladder cancer, laparoscopic staging is warranted because of the high incidence of peritoneal metastases.
■For surgical planning, any patient with a tumor in the neck of the gallbladder or in the cystic duct, or presenting with jaundice, should be scrutinized on preoperative scans for signs of right hepatic arterial involvement. If the right artery is encased, a minimum of an extended lobectomy is necessary for resection.
■Accessory or replaced left hepatic arteries do not reside in the porta hepatis, but rather pass across the lesser omentum and enter the base of the umbilical fissure. Patients with these anomalous vessels can therefore often be resected even when extensive involvement of the porta exists.
■Stay sutures should be placed before dividing the intrahepatic bile duct; otherwise the small segmental duct can slip away and retract within the liver parenchyma.
■The lymphatic vessels throughout this dissection should be tied to prevent postoperative lymphorrhea.
Exploration of the Common Bile Duct:
The Laparoscopic Approach
Jean-François Gigot
Introduction
Stone migration is a common situation encountered during the management of gallstones. Common bile duct (CBD) exploration (CBDE) thus remains the cornerstone of complete surgical treatment of gallbladder and common bile duct stones (CBDs). The first laparoscopic choledochotomy was reported in 1991 by Petelin.
Indications and Contraindications
Indications |
■ |
CBD stone disease |
|
■ |
Failed endoscopic removal of stones |
Choice of Route
■The choice of optimal strategy for laparoscopic CBDE (LCBDE) will be guided by the features of intraoperative cholangiography (IOC), according to the characteristics of the stone and to the biliary anatomy.
The transcystic (TC) route is chosen when there is:
■A patent cystic duct
■A limited number of stones
■Small stone size (stone size £ cystic duct size)
■Stones located below the cystic duct (CD)–CBD junction
■Adequate biliary anatomy of the CD–CBD junction (the ideal case is a perpendicular angle of insertion of CD into the CBD)
Choledochotomy is chosen when there is:
■Dilated CBD ≥7–8mm
■Accessible porta hepatis (no acute inflammation)
554 |
SECTION 4 |
Biliary Tract and Gallbladder |
|
|
|
|
|
|
Contraindications General
■High risk patients (ASA III or IV) for whom an endoscopic approach is preferred
■Dense peritoneal adhesions due to previous upper abdominal surgery (a limitation for the laparoscopic approach)
■Liver cirrhosis with portal hypertension/severe coagulation disorders
Transcystic
■Presence of obstructive cystic valves (associated with a risk of instrumental CD or CBD injury)
■Stones too large for TC stone extraction
■Stones located in the common hepatic duct or in intrahepatic bile ducts
■Inadequate biliary anatomy of the CD (tortuous, etc.) and the CD–CBD junction (parapapillary insertion, acute angle of insertion of CD into CBD, etc.)
Choledochotomy
■Thin CBD (risk of stricture after suturing)
■The presence of severe inflammation (gangrenous cholecystitis, acute necrotizing pancreatitis, etc.) at the porta hepatis, precluding a safe identification of CBD
Preoperative Investigations
History and evaluation: |
Previous and actual clinical history of biliary symptoms |
|
Pain, jaundice, fever, chills, signs of pancreatitis |
Laboratory tests: |
White blood cell (WBC) count, CRP, bilirubin, ALT, AST, alka- |
|
line phosphatase, amylase, lipase, coagulation parameters |
Preoperative radiologic |
Ultrasound, MR cholangiography, endoscopic ultra- |
assessment: |
sonography |
Conditions for LCBDE
■Adequate experience in open biliary surgery and in laparoscopic advanced procedures, in suturing techniques and in endoscopic techniques
■Routine practice of Intraoperative cholangiography (IOC)
■Adequate technical environment (instrumentation, fluoroscopy, flexible scopes, etc.)
Instrumentation/Material
LCBDE is a technically demanding operation requiring:
■High volume insufflator
■High energy light source
■Fluoroscopic intraoperative cholangiographic equipment
■Dormia basket or balloon extraction baskets
■Flexible endoscope 3.5mm (fine, fragile and expansive)
■Contact or laser lithotripsy device (optional)
■Laparoscopic knife
■Laparoscopic needle holder
■Transcystic drain or T-tube
Exploration of the Common Bile Duct:The Laparoscopic Approach |
555 |
|
|
Procedure
Incision
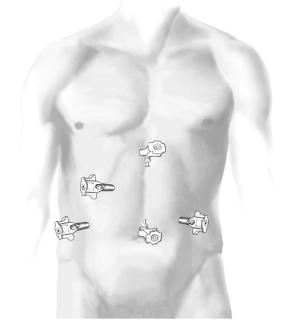
■Same four-trocar technique as for laparoscopic cholecystectomy.
■An additional atraumatic soft fifth trocar is placed below the right costal margin, serving as the port for the introduction of the scope.
Exposure
■LCBDE is performed during cholecystectomy after completion of IOC, when the dissection of Calot’s triangle is completed, the gallbladder remaining in place
■The hepatoduodenal ligament is stretched by pulling up on the quadrate lobe. The patient is placed in an anti-Trendelenburg position to allow gravity to pull down on the duodenum.
556 |
SECTION 4 |
Biliary Tract and Gallbladder |
|
|
|
|
|
|
Laparoscopic Transcystic CBDE |
|
|
|
|
|
|
STEP 1 |
Introduction of instruments |
|
|
|
The cystic duct incision done for performing IOC is used for transcystic CBDE |
||
|
|||
|
(TCBDE). Care is taken to avoid a cystic duct incision too close to the CBD, in order to |
||
|
reduce the risk of instrumental CBD injury. The incision must also not be too far from |
||
|
the CBD, because the presence of obstructive cystic valves may preclude instrumental |
||
|
TCBDE. If the caliber of the sufficiently large CD is not dilated enough, it can be care- |
||
|
fully dilated using a soft, flexible dilator, with care taken to avoid instrumental CBD |
||
|
injury. |
|
|
|
|
|
|
STEP 2 |
Instrumental stone extraction |
|
|
|
Stone extraction through TCBDE can be performed using a three-wire soft Dormia |
||
|
|||
|
basket with three different approaches: |
|
|
|
■ |
By blunt introduction of the instrument into the CBD through the CD. |
|
|
■ |
Under fluoroscopic guidance (safer for ensuring stone capture and avoiding instru- |
|
|
|
mental CBD injury). |
|
|
■ |
Under visual cholangioscopic guidance (for small stones). |
|
A balloon catheter is not used during TCBDE, in order to avoid stone migration in the upper part of the CBD. In the case of huge, impacted, obstructive stones not amenable to extraction by using standard instrumental or endoscopic methods, the stone can be fragmented by using an endoluminal electrohydraulic or laser lithotripsy probe under endoscopic visual control.
Exploration of the Common Bile Duct:The Laparoscopic Approach |
557 |
|
|
|
|
STEP 3 |
Stone clearance assessment |
|
|
|
|
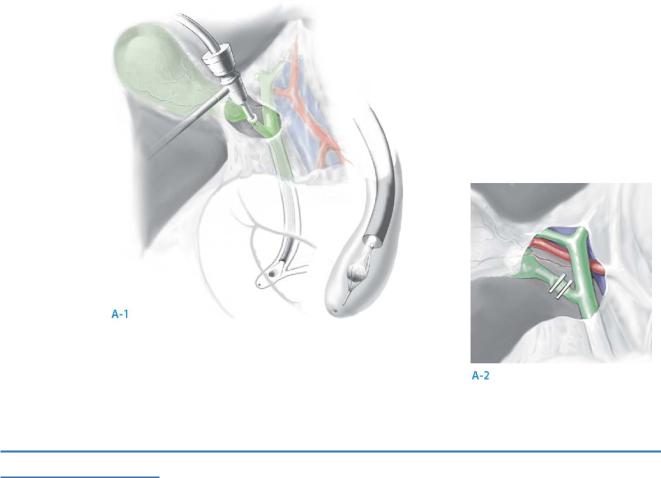
The assessment of complete stone clearance is performed in two different ways:
■By control cholangiography.
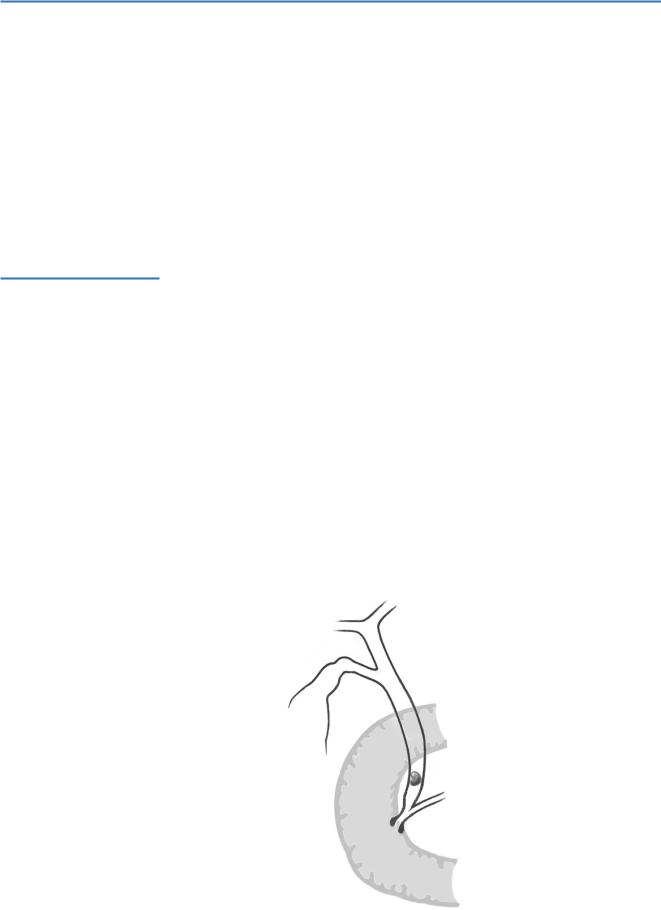
■By using flexible choledochoscopy (A-1, A-2): the scope is introduced under fluoroscopic or visual guidance into the CBD to assess the presence of residual CBDs. When used through a TC approach, choledochoscopic stone clearance assessment is usually only possible in the lower part of the CBD, except in the case of a wide angle of insertion of the CD into the CBD. In this case (15–20% of cases), the scope can be guided into the upper part of the biliary tract.
In case of residual CBDS, an additional endoscopic attempt at stone extraction can be performed by introducing a Dormia basket through the operative channel of the scope, and also by guiding stone capture under visual control. When the number of stones is limited and when stone clearance is complete, the CD can be primarily clipped.
When doubt exists about the completeness of stone clearance, the CBD can be drained by using a transcystic duct drain, carefully secured with an endoloop or an extracorporeal suturing technique.
STEP 4
Routine subhepatic drainage is used.
558 |
SECTION 4 |
Biliary Tract and Gallbladder |
|
|
|
|
Laparoscopic Choledochotomy |
|
STEP 1
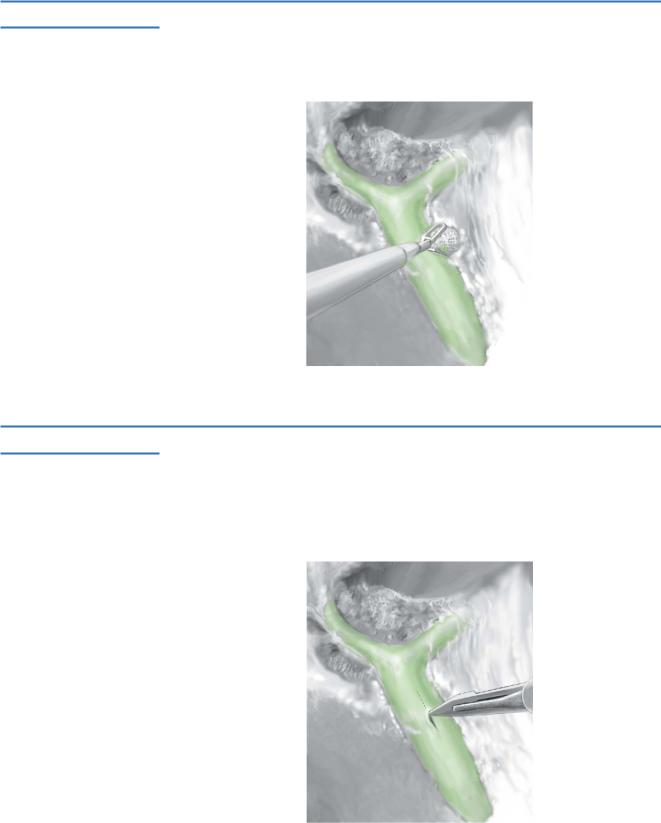
The anterior wall of the CBD is additionally dissected within the porta hepatis, by using blunt or instrumental dissection (avoiding the use of electrocautery close to the CBD).
STEP 2
A longitudinal incision is made with a laparoscopic knife into the CBD after having blown up the CBD with saline solution through the transcystic cholangiographic catheter. The size of the incision is dependent on the size of the largest CBDS to be extracted from the CBD.
Exploration of the Common Bile Duct:The Laparoscopic Approach |
559 |
||
|
|
|
|
STEP 3 |
Stone extraction |
|
|
|
■ |
By blunt introduction of a Dormia basket or a balloon catheter through the choledo- |
|
|
|||
|
|
cholithotomy (A-1, A-2). |
|
|
■ |
Under endoscopic visual control by introducing a Dormia basket or a balloon |
|
|
|
catheter through the operative channel of the flexible scope. |
|
|
■ |
If a large, obstructive stone is encountered, an endoscopic electrohydraulic or laser |
|
|
|
lithotripsy technique can also be used. |
|
