
clavien_atlas_of_upper_gastrointestinal_and_hepato-pancreato-biliary_surgery2007-10-01_3540200045_springer
.pdf
Laparoscopic Cholecystectomy, Open Cholecystectomy and Cholecystostomy |
539 |
||
|
|
|
|
|
Cholecystostomy |
|
|
|
Indications and Contraindications |
|
|
Indications |
■ |
Percutaneous cholecystostomy is used most commonly in the setting of a severely ill |
|
|
|
patient with underlying gallbladder sepsis. |
|
|
|
|
|
|
■ |
Operative severe inflammation of Calot’s triangle at surgery where the safest option |
|
|
|
is to decompress the gallbladder. |
|
Procedure
Cholecystostomy may be performed open but this is much more typically found at laparoscopic cholecystectomy.
STEP 1
STEP 2
STEP 3
The 5-mm lateral trocar is inserted directly into the gallbladder and the gallbladder aspirated. The gallbladder will collapse, typically showing a large stone in Hartmann’s pouch; if this can be milked back and removed it should be done.
A Foley catheter is inserted via the lateral port directly into the gallbladder. Cholangiography can be completed via this if indicated.
The trocar is removed from the gallbladder, leaving the Foley catheter in place, which is then insufflated. The gallbladder is sutured 2nd request around the Foley catheter.
The Foley catheter is then left on free drainage and should be left in place at least 6weeks to allow the gallbladder to settle prior to returning to complete the laparoscopic cholecystectomy.
The Foley catheter should be irrigated twice daily with 20ml of saline.

Resection of Gallbladder Cancer,
Including Surgical Staging
Rebecca Taylor, Yuman Fong
Indications
Relative Contraindications
Contraindications
Introduction
Gallbladder cancer was first described in 1777. The average age at diagnosis is 65years, with women being three times more affected than men. In gallbladder cancer, 90% of the cancers are adenocarcinomas. Gallstones and chronic inflammation of the gallbladder are associated with malignant disease. It is estimated that 1% of patients undergoing cholecystectomy for gallstones are found to have cancer. Twenty percent to 60% of gallbladders with calcifications (porcelain gallbladder) will develop cancer.
Natural History
■Patients with incompletely resected gallbladder cancer have a 5-year survival rate of less than 5%
■Completely resected patients have a 5-year survival rate of 17–90% depending on stage of disease
Indications and Contraindications for Resectional Procedures
■Gallbladder cancer with T1–4, N0/1 and M0
■Lymph node metastases to N2 compartment
■Peritoneal carcinomatosis or other distant metastases (M1)
Presentation
■Mass in segment 4/5 associated with gallbladder
■During surgery for presumed cholelithiasis or as pathologic finding after cholecystectomy for presumed gallstone disease
■One-third of patients will present with jaundice
542 |
SECTION 4 |
Biliary Tract and Gallbladder |
|
|
|
|
Preoperative Investigations and Preparation for the Procedure |
|
|
History: |
Biliary colic, jaundice, itching, weight loss, previous gallbladder |
|
|
or biliary surgery |
|
Physical examination: |
Right upper quadrant mass |
Imaging
■Ultrasound
■Contrast-enhanced CT scan (CT angiogram is preferred)
■Magnetic resonance cholangiopancreatography (MRCP)
■Cholangiography [if invasive cholangiography is necessary, percutaneous cholangiography (PTC) is preferred over endoscopic retrograde cholangiopancreatography (ERCP)]
■Direct arteriography (rarely needed)
■Important anatomic details: porcelain gallbladder, mass, enlarged/necrotic lymph nodes, arterial involvement, portal venous involvement, adjacent organ (colon, duodenum) involvement, peritoneal metastasis
■Gallbladder polyp [solitary, sessile, large (>1cm) polyps are worrisome for cancer]
■Look at anomalous pancreaticobiliary duct junction, choledochal cyst, and of course hepatic arteries
Extent of Resection According to Stage
Patients presenting with gallbladder mass on imaging or operative exploration:
■T2/3, N0/1, M0: radical cholecystectomy and lymph node dissection
■Unilateral vascular involvement: extended lobectomy and lymph node dissection
■T4, N0/1, M0: extended lobectomy and lymph node dissection, possible adjacent organ resection
■N2 or M1: no curative surgery, possible palliation by biliary or gastric bypass
Patients with cancer discovered as an incidental finding after cholecystectomy for presumed cholelithiasis:
■T1 with negative liver and cystic duct margin: no further therapy
■T1 with positive cystic duct margin: re-resection of cystic duct or common bile duct to negative margins
■T2/3/4, M0: extended lobectomy, common bile duct resection, lymph node dissection, and resection of laparoscopic port sites
■N2 or M1: no curative surgery (palliation)
Resection of Gallbladder Cancer, Including Surgical Staging |
543 |
|
|
Procedure
A radical cholecystectomy (including segments 4b and 5) resection will be described. If an extended lobectomy is necessary because of the bulk of the tumor or because of vascular invasion, the dissection of the porta hepatis and hilar areas is performed as described below. With gallbladder cancer, when an extended resection is necessary, it is usually an extended right lobectomy. The liver resection is then performed as described in Sect.3,“Liver,” after the vasculature to the left side is dissected free and protected and the left hepatic duct has been divided.
|
Incision |
|
|
■ |
No previous surgery: A low right subcostal (hockey stick) incision is favored |
|
|
(see Sect.1, chapter “Positioning and Accesses” for descriptions of incisions and |
|
|
division of falciform) |
|
■ |
Previous cholecystectomy: Subcostal incision to incorporate excision of previous |
|
|
open or laparoscopic port incisions plus separate excision of umbilical port |
|
|
|
STEP 1 |
Surgical exploration |
|
|
Exposure and exploration: installation of the retractor (see Sect.1, chapter “Retractors |
|
|
||
|
and Principles of Exposure”) and inspection of possible port site and peritoneal |
|
|
metastasis |
|
|
|
Ultrasound to evaluate location of the primary tumor in relation to vascular |
structures (portal vein, hepatic artery, hepatic vein) and to rule out discontiguous liver metastases
Careful inspection of vascular variation
544 |
SECTION 4 |
Biliary Tract and Gallbladder |
|
|
|
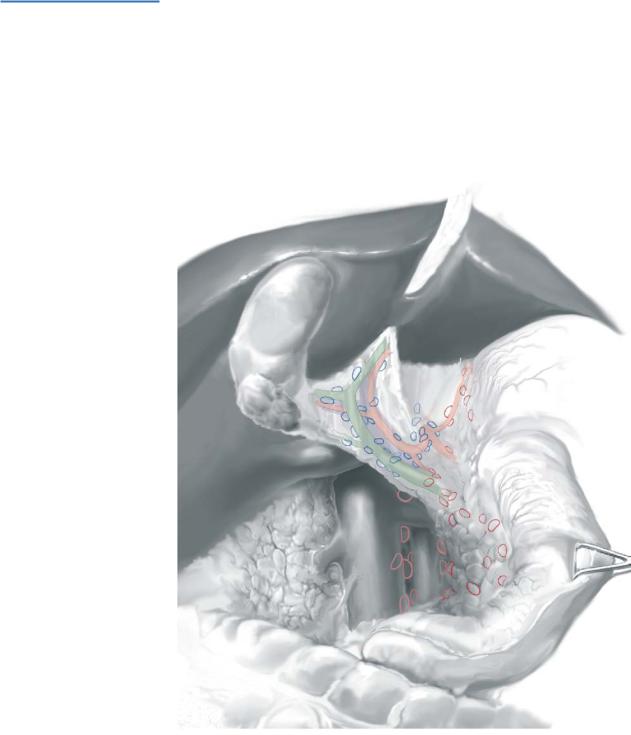
STEP 2 |
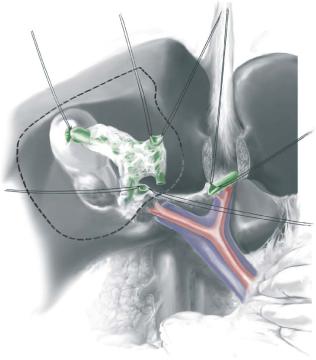
Area resected by radical cholecystectomy, and regional lymph node |
|
and connective tissue dissection
The two segments (4b and 5) contiguous with the gallbladder bed are resected.
N1 lymph nodes (blue): those in the hepatoduodenal ligament (No.12) and common hepatic (No.8) and celiac arteries (No.9) are resected. Positive N2 nodes (red), retropancreatic nodes (No.13), perigastric nodes or aortocaval nodes indicate incurable disease.
Nerve plexuses around the hepatic artery should be dissected.
Full kocherization allows inspection of these nodal stations and facilitates subsequent dissection.
Resection of Gallbladder Cancer, Including Surgical Staging |
545 |
|
|
|
|
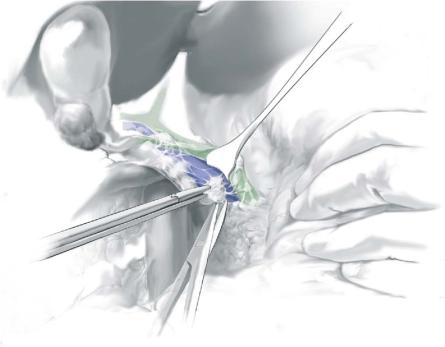
STEP 3 |
Excision of the highest peripancreatic lymph node |
|
|
|
|
After kocherization, the highest peripancreatic lymph node is excised. This node is sent for frozen section histologic analysis. After excision of this node, retraction of the bile duct anteriorly allows visualization of the portal vein and facilitates safe dissection of nodal and connective tissues. Frozen section staging using this node also guides the operative procedure. If this node is positive and the patient is at high medical risk, then the radical resection is usually abandoned. A radical resection performed in the setting of a positive node should include a retropancreatic nodal dissection and aortocaval nodal dissection, with or without a pancreaticoduodenectomy.
546 |
SECTION 4 |
Biliary Tract and Gallbladder |
|
|
|
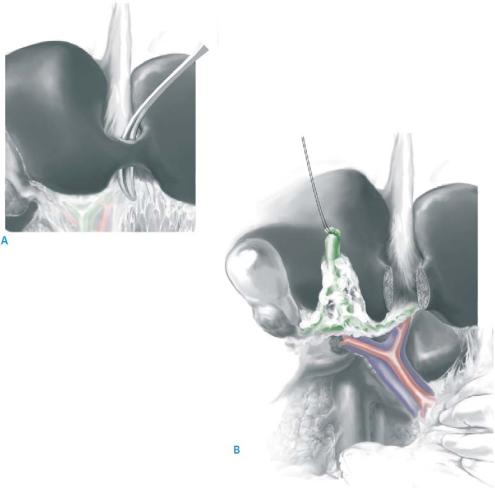
STEP 4 |
Common bile duct resection |
|
|
|
|
Except in the very thin patient, it is very difficult to adequately excise the nodal tissue in the porta hepatis without resecting the common bile duct. This is particularly true if the patient has recently had a cholecystectomy, so that the scars from such surgery further complicate identification of nodal tissue and tumor. Resecting the common bile duct also allows the most certainty of resection of the cystic duct–common duct junction. Furthermore, resecting the common duct allows the safest dissection and inspection of the portal vein and hepatic arteries behind the tumor and in the hilar area.
The bridge of liver tissue between segments 4b and 3, overlying the base of the falciform, is divided (A) to allow access to the left portal pedicle. The common bile duct is divided immediately above the pancreas and reflected upward (B). The resection margin must be examined by frozen section. All nodal and connective tissues, including the celiac, hepatoduodenal, and portal-caval nodes, are dissected with the common duct, leaving behind only the skeletonized portal vein and hepatic artery.

Resection of Gallbladder Cancer, Including Surgical Staging |
547 |
|
|
|
|
STEP 5 |
Assessment of the portal vein and hepatic artery |
|
|
With the common duct and portal nodal tissue reflected upward, the main, left, and |
|
|
|
|
|
right portal veins and arteries are dissected. If the main portal vein is involved, a portal |
|
|
vein resection and reconstruction may be necessary (see below). If the right hepatic |
|
|
artery and/or right portal vein are involved, an extended right liver resection is |
|
|
warranted. Once the arterial anatomy and possible arterial variations are clearly |
|
|
identified, the right or left hepatic artery is skeletonized distally to the right and left |
|
|
extremes of the hilar plate. In doing so, the left and right hepatic ducts are dissected free. |
|
|
|
|
STEP 6 |
Transection of the left and right hepatic ducts |
|
|
The left hepatic duct is then identified and transected at the base of the umbilical fissure. |
|
|
||
|
Unlike the dissection for a hilar cholangiocarcinoma, the junction of the left and right |
|
|
hepatic ducts can usually be freed from the liver. Retraction of the left hepatic duct |
|
|
stump upward then allows a good look at the right hepatic duct from the posterior-infe- |
|
|
rior aspects. A stay suture is then placed on this duct before transection. |
|
548 |
SECTION 4 |
Biliary Tract and Gallbladder |
|
|
|
STEP 7 |
Liver resection |
|
|
|
|
After transection of the right hepatic duct, tissue from both the left and right ductal margins is sent for frozen section analysis. The entire gallbladder bed including segments 4b and 5 is then resected along the dotted lines shown. The portal veins and hepatic arteries are protected under direct vision. Liver parenchymal transaction is as described in Sect.3, chapters “Liver Resections” and “Left Hemihepatectomy,” usually with inflow occlusion by the Pringle maneuver, and with central venous pressure (CVP) maintained below 3cm H2O (see Sect.3, chapter “Extended Hemihepatectomies”).
Resection of Gallbladder Cancer, Including Surgical Staging |
549 |
|
|
|
|
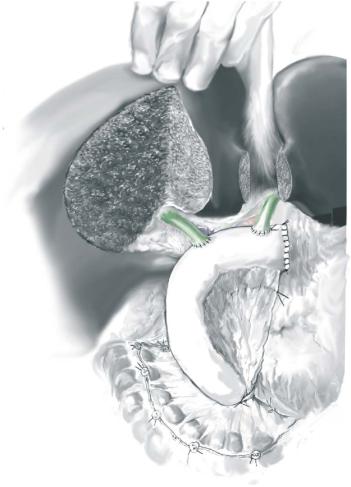
STEP 8 |
Biliary reconstructions |
|
|
|
|
Before bilioenteric anastomosis, the left and right hepatic ducts can be joined by interrupted, absorbable sutures (4-0 or 5-0 Vicryl or PDS) to minimize the number of the anastomosis. Alternatively, the two ducts can be anastomosed separately. A 70-cm Roux-en-Y jejunal loop is lifted through the shortest route that allows for no tension on the anastomosis: retrocolic or retrogastric. For details on the biliary anastomosis, please see this section, chapters “Intrahepatic Biliodigestive Anastomosis Without Indwelling Stent” and “Reconstruction of Bile Duct Injuries.” If a plastic biliary stent has been placed before surgery, it is removed and not replaced. If a metal stent has been placed, it is usually safest to cut across the metal stent at a site believed to be free of cancer. The jejunal loop is then sewn to the duct and the stent.
