
clavien_atlas_of_upper_gastrointestinal_and_hepato-pancreato-biliary_surgery2007-10-01_3540200045_springer
.pdf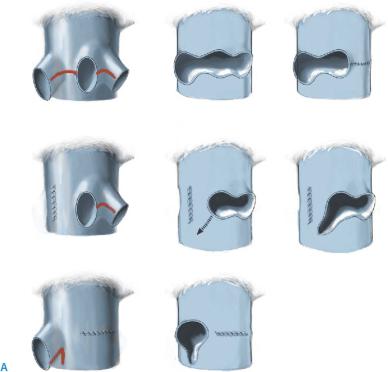
Living Related Liver Transplantation: Left Hemiliver Donor Procedure and Implantation |
507 |
|
|
|
|
STEP 2 |
Reconstruction of the hepatic vein |
|
|
|
|
We have three standard procedures for hepatic vein reconstruction in left-sided graft implantation: (a) one orifice using all of the hepatic veins, (b) the left and middle hepatic vein orifices and an additional incision of the IVC, and (c) the right hepatic vein and an additional incision of the IVC (A).
Preparation of a single orifice by using all of the hepatic veins is shown in the following figures: The inferior vena cava is entirely clamped to include all hepatic venous stumps (B-1). All septa are opened to create a single hole (B-2) and the size is measured (B-3). If the hole is too large for the hepatic vein of the graft, the diameter is adjusted by 5-0 Prolene suture at the left corner of the hole. Stitches with double armed 5-0 Prolene or PDS are placed on the right and left corners (B-4). The posterior anastomosis is made by the intraluminal method. After accomplishing the anastomosis, another small vascular clamp is placed just proximal to the anastomosis and the large one is removed to resume blood flow of the inferior vena cava.
508 |
SECTION 3 |
Liver |
|
|
|
STEP 2 (continued) |
Reconstruction of the hepatic vein |
|
|
|
|
Preparation of a single orifice by using all of the hepatic veins is shown in the following figures: The inferior vena cava is entirely clamped to include all hepatic venous stumps (B-1). All septa are opened to create a single hole (B-2) and the size is measured (B-3).
If the hole is too large for the hepatic vein of the graft, the diameter is adjusted by 5-0 Prolene suture at the left corner of the hole. Stitches with double armed 5-0 Prolene or PDS are placed on the right and left corners (B-4). The posterior anastomosis is made by the intraluminal method. After accomplishing the anastomosis, another small vascular clamp is placed just proximal to the anastomosis and the large one is removed to resume blood flow of the inferior vena cava.

Living Related Liver Transplantation: Left Hemiliver Donor Procedure and Implantation |
509 |
|
|
|
|
STEP 3 |
Portal vein anastomosis |
|
|
|
|
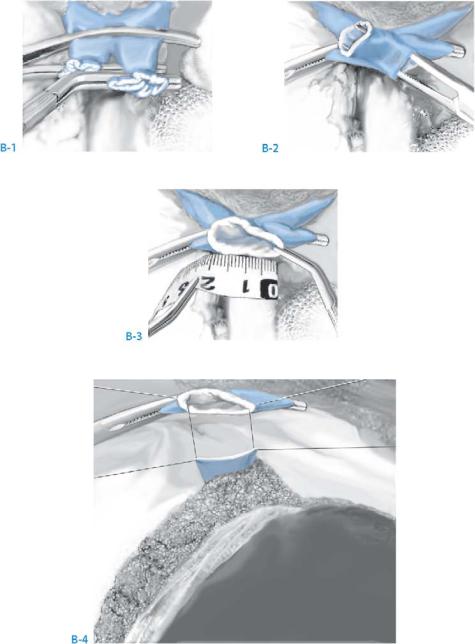
Different techniques can be used for portal vein preparation (A), including: (a) with a branch patch, (b) with an oblique incision, (c) graft interposition, and (d) a patch graft. The first two are the simplest and most frequently used to adjust the graft size of the portal vein. If the portal vein wall is damaged or narrow, it should be changed with a venous graft. When the available venous graft is too small for interposition, the patch graft technique using a patch made from a small venous graft which is longitudinally opened is recommended.
Before the portal anastomosis is started, the portal vein should be briefly unclamped and washed with heparinized saline to check the flow and to remove possible coagula. The anastomosis is started by placing two double armed 6-0 Prolene or PDS sutures at the right and left corner of the graft portal vein. Anastomosis of the posterior wall is first carried out from the inside, in a running suture fashion. During the anastomosis, the suturing stitch should be kept loose to prevent anastomotic stricture (B). When this technique is used, creation of a growth factor is not required.
This continuous suture is our standard technique in most cases. However, interrupted sutures are used for the anterior wall subsequent to a running suture for the posterior wall in cases of a size mismatch or a small diameter using 7-0 Prolene or PDS.
510 |
SECTION 3 |
Liver |
|
|
|
STEP 4 |
Arterial anastomosis |
|
|
|
|
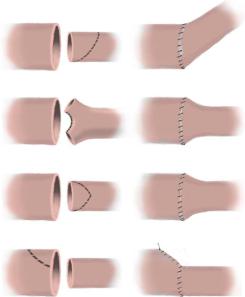
A surgical microscope and magnifying glasses should be used to perform the arterial anastomosis. First, excellent front flow of the recipient artery needs to be confirmed. Both arteries are clamped with fine vascular clips and are freed from the surrounding connective tissue with microscissors until the smooth adventitial surface is reached. The anastomosis is carried out with an interrupted 8-0 Prolene suture.
Size mismatch between the graft and recipient artery is frequently encountered. In most cases it can be managed by simple mechanical dilatation of the smaller artery
using fine forceps. When the mismatch is significant, several techniques for adaptation can be used. In cases of multiple arteries, a larger one is chosen for the first anastomosis. When excellent arterial backflow is observed from the second artery after the first anastomosis, the second artery can be ligated.
Living Related Liver Transplantation: Left Hemiliver Donor Procedure and Implantation |
511 |
|
|
|
|
STEP 5 |
Biliary anastomosis |
|
|
|
|
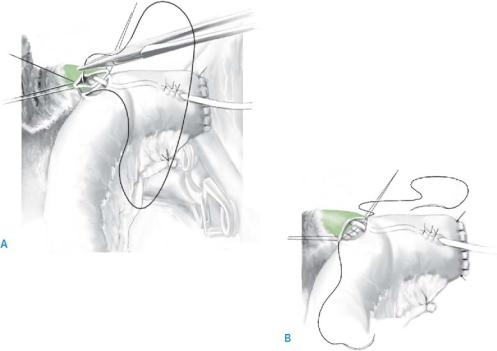
In patients with biliary atresia, pediatric patients with small-diameter bile ducts, or in patients with primary sclerosing cholangitis and a sclerotic common bile duct, a hepatico-jejunostomy should be performed. In other cases, a duct to duct anastomosis can be performed in a similar way as for orthotopic or right living donor liver transplantation.
A small hole is made in the Roux-en-Y limb close to the proximal end. A 4-Fr polyvinyl alcohol tube is inserted through the hole into the intestinal lumen as an external stent and is led out of the intestinal wall again. Two double-armed 6-0 PDS sutures are placed on the right and left corner of the graft hepatic duct. The stitch of the right corner is pulled with a small clamp to open the hepatic duct. Anastomosis of the posterior wall is made first with a running suture using the stitch of the left corner (A). After completion of the posterior wall, the inside needle of the stitch of the right corner of the graft is passed through the corner of the jejunum from inside to outside. After insertion of the tip of the stent into the duct lumen, anastomosis of the anterior wall is made using another needle of the left corner in running fashion (B). When the diameter of the hepatic duct is small, an incision on the anterior wall along the axis can be used to enlarge it.
512 |
SECTION 3 |
Liver |
|
|
|
|
Tricks of the Senior Surgeon |
|
■Preparation of the hepatic artery for a left lateral segment liver graft:
In case a small middle hepatic artery disturbs the hilar dissection, it can be cut after confirmation of a sufficiently large left hepatic artery. By contrast, the left hepatic artery should be kept even if it seems to be too small for anastomosis until the anatomy of the left and middle hepatic artery is clarified.
■Preparation of the hepatic duct for a left lateral segment liver graft:
When the left hepatic duct is cut above the B 4 bifurcation to preserve it for the donor, this is likely to result in two separate bile ducts (B2 and B3), which would complicate the biliary anastomosis. Therefore, we recommend the preparation of a single biliary orifice even if B4 needs to be sacrificed for this purpose. Since the inflow to Sg4 is usually limited it usually shrinks which leads to a compensatory enlargement of the remnant liver. Hence, the occlusion of B4 will not be a problem for the recipient.
■“Monosegment grafts”:
In cases where the lateral segment is too large, the graft can be reduced by cutting the lateral half or two thirds. If this reduced graft is still too large, the caudal 1/3 can be removed.
■To prevent twisting of the hepatic vein secondary to dislocation of the graft into the right subphrenic space, the falciform ligament should be reattached before the abdomen is closed.
Auxiliary Liver Transplantation
Karim Boudjema, Philippe Compagnon, Jean-Pierre Campion
The principle of auxiliary liver transplantation is the implantation of a right or left hemiliver into the abdominal cavity to restore normal liver function temporarily, while the native liver recuperates. Once the native liver has recovered, the graft can be removed or left in place without immunosuppression leading to atrophy.
Indications and Contraindications
Indications |
■ |
Fulminant and subfulminant liver failure (approximately 10% of all liver |
|
|
transplant indications) as defined by the King’s College or the Clichy criteria |
|
■ |
Fulminant rather than subfulminant form of acute liver failure (interval |
|
|
jaundice/encephalopathy <2weeks) |
|
■ |
Preferentially acute liver failure due to viral hepatitis (A and B), mushroom |
|
|
intoxication or drugs that are known to induce reversible acute liver failure |
|
|
General contraindications to transplantation |
Exclusion Criteria |
■ |
|
|
■ |
Presence of fibrosis (or cirrhosis) on a frozen section biopsy performed during |
|
|
the procedure |

514 |
SECTION 3 |
Liver |
|
|
|
|
|
|
Special Considerations |
|
|
|
■ |
Since there is not enough space in the abdominal cavity to harbor two entire livers, |
|
|
|
the graft has to be reduced. |
|
|
■ |
The reduced liver graft can be implanted heterotopically, i.e., below the native liver, |
|
|
|
but this technique may lead to a portal steal syndrome and compromise graft |
|
|
|
vascularization. |
|
|
■ |
Orthotopic implantation of the graft is more physiologic and is widely accepted |
|
|
|
as the standard technique. It implies resection of a native hemiliver. Consequently, |
|
|
|
two types of auxiliary partial orthotopic liver transplantation (APOLT) can be |
|
|
|
performed depending on the type of graft that is used: |
|
|
|
– Right APOLT (A-1): right hemihepatectomy of the native liver and implantation |
|
|
|
of a right liver graft (Sg5, 6, 7 and 8 and right part of the dorsal sector) |
|
|
|
– Left APOLT (A-2): left hemihepatectomy of the native liver and implantation |
|
|
|
of either a left lateral section (Sg2 and 3) or a left hemiliver (Sg2, 3 and 4) |
|
|
■ |
The liver graft can be harvested from a living donor or a cadaveric donor. |
|
|
|
When harvested from a cadaveric donor, the liver can be split in situ or ex situ. |
|
|
■ |
Two teams are mandatory and work simultaneously: |
|
|
|
– A donor team which procures and splits the graft |
|
|
|
– A recipient team which fits up the recipient abdominal cavity and performs |
|
|
|
the transplantation |
|
Auxiliary Liver Transplantation |
515 |
|
|
Specific Postoperative Complications
■Primary non-function of the liver graft
■Bleeding from the cut surfaces of both native and auxiliary livers
■Stricture of the portal vein anastomosis and subsequent portal steal syndrome and graft non-function
■Hepatic artery thrombosis and subsequent biliary tract necrosis of an atrophic graft
Procedures
Right Auxiliary Partial Orthotopic Liver Transplantation
Right APOLT is recommended for adult patients in order to raise the graft weight/patient weight ratio above 1%.
This part of the procedure mimics removal of a right living donor procedure except that it can be performed under selective occlusion of the right portal triad.
516 |
SECTION 3 |
Liver |
|
|
|
STEP 1 |
Exploration, mobilization and resection of the native right hemiliver |
|
|
|
|
After visual and manual exploration of the liver and the entire abdominal cavity, the vascular structures (median hepatic vein and its branches from segments V and VIII) are evaluated by ultrasound with a special emphasis on anatomical variations that may complicate the procedure (i.e., absence of right portal trunk). Next, a wedge biopsy is performed for the evaluation of fibrosis, as the presence of fibrosis or cirrhosis is a contraindication for auxiliary liver transplantation. Parenchymal necrosis is common and its intensity does not necessarily predict the likelihood of recovery.
After cholecystectomy, the right hemiliver is mobilized. Of note, the distal end of the right hepatic vein can be encircled from below using a lace but should not be transsected at this stage.
The lateroposterior peritoneal sheath of the right part of the hepatoduodenal ligament is opened and the right hepatic artery is gently dissected from behind the common hepatic duct up to its bifurcation and marked with a vessel loop. The right branch of the portal vein is cautiously freed from the hilar plate. This maneuver cannot be performed safely without having controlled and cut one or two small branches to the caudate process. The vein is also marked with a vessel loop.
The right hepatic artery and the right portal vein are temporarily occluded with vascular clamps in order to reveal the demarcation line between left and right hemiliver. Then both vessels are divided between ligatures, as distally as possible.
The right hepatic duct should not be isolated extrahepatically. It can easily be transsected during the parenchymal dissection.
The liver parenchyma is transected 1cm to the right of the main portal fissure, preserving the median hepatic vein. Transection is conducted posteriorly to the retrohepatic vena cava and the right hepatic duct is divided through the liver parenchyma at the confluence of its anterior and posterior branches. The bile duct from segment one is carefully preserved. Then, the right hepatic vein is transected by means of a vascular stapler (or another technique; see chapter “Right Hemihepatectomy”). At the end the retrohepatic segment of the inferior vena cava is widely exposed, ready to receive the right hepatic graft.
