
clavien_atlas_of_upper_gastrointestinal_and_hepato-pancreato-biliary_surgery2007-10-01_3540200045_springer
.pdf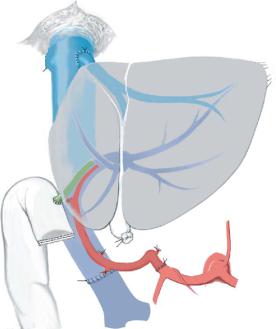
Partial Cadaveric Liver Transplantation: Donor Procedure and Implantation |
487 |
|
|
Implantation of the Left Graft in a Pediatric Recipient (Sg2 and 3)
As in this situation the cava stays with the right graft, the left hepatic vein is anastomosed directly on the inferior vena cava of the recipient. It is fundamental to keep the hepatic vein short as too long a vein can lead to kinking of the caval anastomosis. End- to-end anastomosis of the portal vein between the donor’s left portal vein and the recipient common trunk is performed. Finally, the celiac axis of the left graft is anastomosed to the hepatic artery of the recipient at the level of the gastroduodenal artery and biliary continuity is reconstituted by a Roux-en-Y biliodigestive anastomosis.
488 |
SECTION 3 |
Liver |
|
|
|
|
Alternative Management of the Hepatic Venous Outflow |
|
|
in Split Liver Transplantation for Two Adults |
|
|
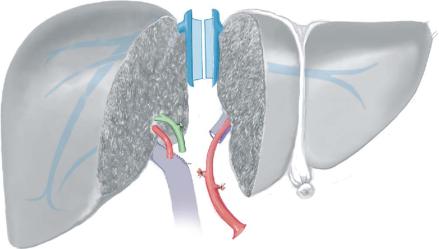
In split liver transplantation for two adults, the maintenance of an optimal venous |
|
outflow is of great importance to safeguard a maximal parenchymal integrity. In principle the same venous reconstructions and anastomoses are made as in right liver donation, including reanastomosis of segment 6 veins and reconstruction of larger segment 5 or 8 veins as shown. Additionally two techniques, not usable in living donation, can be applied to make the implantation easier while maintaining optimal venous outflow.
Splitting of the Inferior Vena Cava
This technique can be used in the in-situ as well as in the ex-situ technique. The frontand backwall of the vena cava are cut longitudinally, thus obtaining a caval patch on both grafts containing the respective hepatic veins as well as a possible segment 6 vein on the right side and Sg1 veins on the left side. At implantation the caval patches are sewn into the front wall of the preserved recipient vena cava.
Partial Cadaveric Liver Transplantation: Donor Procedure and Implantation |
489 |
|
|
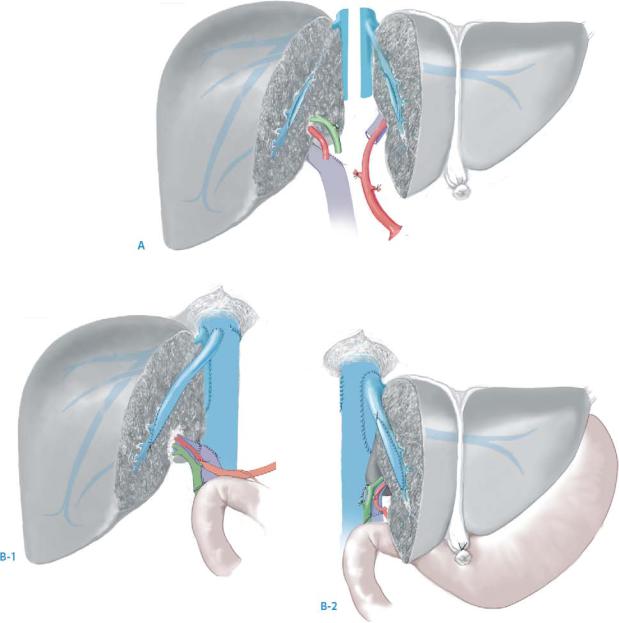
Splitting of the Middle Hepatic Vein
This technique can only be performed in ex-situ splitting. During parenchymal transection the middle hepatic vein is cut through the middle, in continuity with its orifice in the vena cava (A). On both sides it is reconstructed using donor iliac vein patches. In this way larger segment 5 or 8 veins are drained without the need for any further reconstructions or anastomoses (B-1, B-2).
490 |
SECTION 3 |
Liver |
|
|
|
|
|
|
Routine Postoperative Tests |
|
|
|
■ |
Doppler ultrasound examination daily in the intensive care unit, then weekly until |
|
|
|
discharge |
|
|
■ |
Laboratory parameters as for orthotopic liver transplantation |
|
Postoperative Complications
■Biliary leaks from the raw surface, which usually resolve with percutaneous drainage
■Other complications are the same as for orthotopic liver transplantation or living donor transplantations and should be treated accordingly
Tricks of the Senior Surgeon
■Sharp transection of the parenchyma is preferred as it leaves a flat surface allowing for most efficient hemostasis.
■Clips have a propensity to drop off during the implantation procedure. Therefore, every individual vessel seen on the cut surface is closed with stitches. During this step, care is taken to avoid liver rewarming by applying cold towels, leaving only the cut surface exposed.

Right Living Donor Hemihepatectomy
Zakiyah Kadry, Pierre-Alain Clavien
Indications and Contraindications
General Donor Criteria |
■ |
Age 18 and 60years |
|
■ |
ABO compatibility between donor and recipient |
|
■ |
No major medical problems |
|
■ |
Significant long-term emotional relationship to the potential recipient |
|
■ |
Donor competent to give informed consent |
|
|
Donor age <18years or >60years |
Donor Contraindications |
■ |
|
|
■ |
ABO blood group incompatibility |
|
■ |
Significant co-morbid condition (e.g., morbid obesity, coronary artery disease) |
|
■ |
Multiple previous upper abdominal operations |
|
■ |
Hepatic steatosis >30% (cut off center dependent) |
|
■ |
Donor remnant liver volume <5% of the total liver volume |
|
■ |
Significant celiac artery stenosis |
|
■ |
Anatomic variations (center dependent) |
|
■ |
Body mass index >28 (if a liver biopsy is not performed) |
Right Lobe Living Donor Workup
■Psychological evaluation and clinical examination
■Laboratory tests for undiagnosed liver disease
■Non-invasive tests for the assessment of liver volume and anatomy:
–CT scan or MRI for volumetry and vascular reconstruction
–Magnetic resonance cholangiopancreatography (MRCP) or CT cholangiography for biliary anatomy (center dependent)
■Invasive tests:
–Liver biopsy (center dependent)
–ERCP (center dependent)
492 |
SECTION 3 |
Liver |
|
|
|
|
Procedure |
|
|
|
|
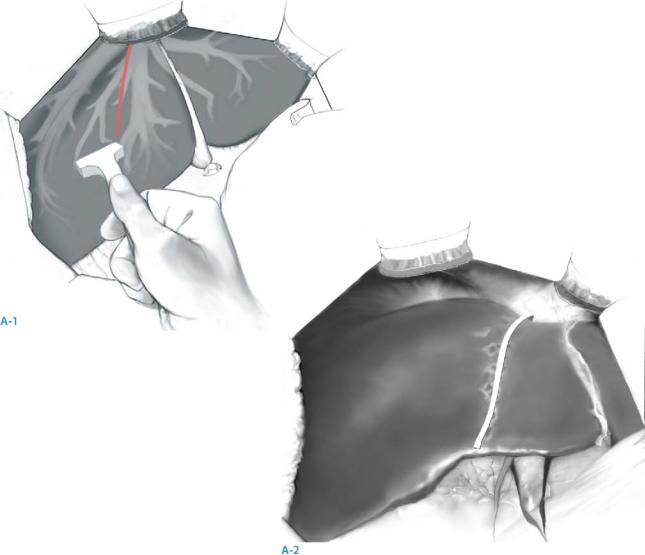
STEP 1 |
Access and intraoperative evaluation |
|
|
After a bilateral subcostal incision an appropriate retractor (e.g., Thompson retractor) is |
|
|
||
|
placed as for a conventional right hemihepatectomy. The division of the round and falci- |
|
|
form ligaments is followed by a careful exploration of the abdominal cavity. The falci- |
|
form ligament should be cut at a distance from the liver as it will be sutured to the diaphragm at the end of the procedure. The left triangular ligament is also preserved to fix the remnant left liver. Guided by intraoperative ultrasound (A-1), the position of the middle hepatic vein is marked by electrocautery (A-2) and any intrahepatic lesions missed on the preoperative workup are excluded.
Right Living Donor Hemihepatectomy |
493 |
|
|
|
|
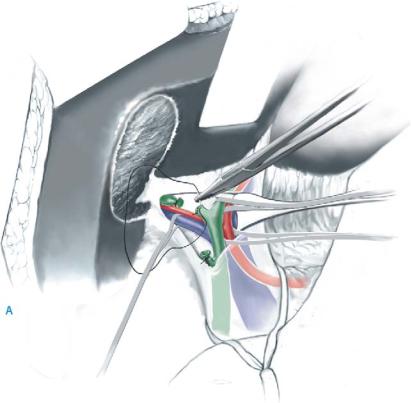
STEP 2 |
Hilar dissection |
|
|
|
A cholecystectomy is performed and an intraoperative cholangiogram is obtained with |
|
|
|
|
|
a radiopaque marker such as a metallic clip or a small metal bulldog clamp placed near |
|
|
the point where the right hepatic duct is thought to lie. At completion of the cholan- |
|
|
giogram and once no contraindications to living donation are identified on exploration, |
|
|
the recipient is brought to the operating room. |
|
|
Next, the hepatic hilum is exposed and the posterior right aspect is palpated to check |
|
|
for a right hepatic artery arising from the superior mesenteric artery (SMA). The peri- |
|
|
toneum and lymphatic tissue are divided on the right lateral aspect of the hepatic hilum |
|
|
avoiding skeletonization of the common bile duct as this could lead to strictures. After |
|
|
identification of the right hepatic artery on the posterior aspect of the bile duct it is |
|
|
followed both to its bifurcation distally and to its origin proximally without traction. |
|
|
The proximal point may occasionally be just distal to the point of origin of the segment |
|
|
4 branch (which should be preserved to avoid vascular compromise of segment 4), the |
|
|
gastroduodenal artery or the origin of the left hepatic artery. An adequate length of |
|
|
right hepatic artery is required and the point of proximal transection is variable |
|
|
depending on the donor anatomy. |
|
|
The right portal vein branch is identified posterior to the bile duct in the right |
|
|
hilum. When isolating the right portal vein, care must be taken to identify clearly the |
|
|
confluence of the right and left portal veins as well as the main portal vein trunk. |
|
|
The posterior branch arising from the right portal to the caudate process should be |
|
|
identified and divided between ligatures to avoid accidental tearing and hemorrhage. |
|
|
A vessel loop can be placed around the right portal vein. |
494 |
SECTION 3 |
Liver |
|
|
|
STEP 2 (continued) |
Hilar dissection |
|
|
|
|
If a portal vein trifurcation is present, the anterior and posterior branches should be individually identified and separately encircled.
The point of transection of the right hepatic duct as decided by intraoperative cholangiography is marked either with a metallic clip or a fine suture. The division of the right hepatic duct is started on its anterior wall at 2–3mm from the confluence with the left hepatic duct. Then, the posterior wall of the right hepatic duct is divided, leaving an adequate cuff to close the remaining donor side using a continuous suture of 5-0 or 6-0 resorbable PDS or Maxon without causing a stricture of either the common or left hepatic ducts. If there are an additional one or two bile ducts draining segments of the right liver into the left hepatic duct, they are identified and divided during the parenchymal dissection.

Right Living Donor Hemihepatectomy |
495 |
|
|
|
|
STEP 3 |
Mobilization of the right lobe and preparation of the right hepatic vein |
|
|
|
The right liver is mobilized basically as for a conventional right hemihepatectomy with |
|
|
|
|
|
the important difference being that short accessory hepatic veins greater than 5mm in |
|
|
diameter should be preserved for venous reconstruction in the recipient. |
496 |
SECTION 3 |
Liver |
|
|
|
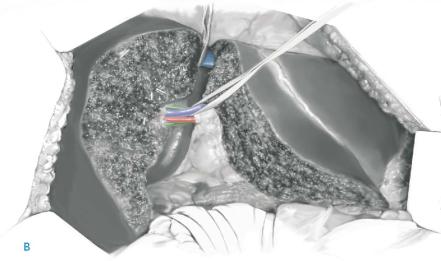
STEP 4 |
Hepatic parenchymal transection |
|
|
|
|
The line of hepatic transection should be approximately 1cm to the right of the middle hepatic vein, identified and demarcated at the start of the procedure by intraoperative ultrasound. The line of demarcation can also be checked by placing a vascular or bulldog clamp on the right hepatic artery and right portal vein.
Alternatively, a partial Pringle maneuver involving the left hemiliver by temporarily occluding the left hepatic artery and portal vein using an umbilical tape is also possible. This allows demarcation of the line of transection, which can be marked using electrocautery. Next, two stay sutures (2-0 silk) are placed on either side of the line of demarcation on the inferior border of the liver as for a conventional right hemihepatectomy.
The anesthesiologist is asked to maintain a low central venous pressure below 3mmHg. In case the hanging maneuver (see chapter “Hanging Maneuver for Right Hepatectomy”) is used, it is prepared at this stage. Although different techniques for liver dissection can be used, Hydrojet or CUSA without inflow occlusion is preferred in most centers.
In a standard right donor hepatectomy, the middle hepatic vein is conserved and remains with the donor left liver. When V5 and/or V8 are significant and have to be preserved, they are carefully identified during the dissection and divided between a vascular metal clip on the right side and a ligature of 2-0 silk on the left side close to the middle hepatic vein. This preserves the V5 and V8 veins for venous drainage reconstruction in the recipient.
On completion of the parenchymal transection, time is taken to re-check for hemostasis and any potential bile leakage on both the graft and donor side.
