
clavien_atlas_of_upper_gastrointestinal_and_hepato-pancreato-biliary_surgery2007-10-01_3540200045_springer
.pdf
Orthotopic Liver Transplantation |
467 |
|
|
STEP 2 (continued) |
Mobilization of the infrahepatic inferior vena cava |
|
The Cava-Sparing (or Piggyback) Technique |
|
|
|
For this technique the right liver is rotated to the left upper quadrant in order to expose |
|
adequately the right and anterior sides of the retrohepatic IVC. The tissue between the |
|
retrohepatic IVC and the posterior surface of the liver is divided. All smaller Spigelian |
|
veins draining the caudate lobe and the right accessory veins when present are selec- |
|
tively ligated and divided from below upwards. In this way, the hepatic veins are |
|
approached. The right hepatic vein is encircled and transected using a vascular endosta- |
|
pler. Precise stapler application close to the liver parenchyma permits safe and tight |
|
transsection of the right hepatic vein without narrowing the retrohepatic IVC. The |
|
transsection of the right hepatic vein allows the retrohepatic-IVC to be turned away |
|
from to a further extent and makes the safe isolation of the middle and left hepatic veins |
|
much easier. |
|
Some surgeons construct a temporarily end-to-side portal-caval shunt to reduce |
|
splanchnic pressure and bleeding and to facilitate mobilization of the liver (not shown). |
|
In the case of a retransplant following a previous classical liver transplant with IVC |
|
replacement, the previous allograft’s IVC is preserved. The plane between the |
|
parenchyma and the previous donor IVC will have remained intact. In case of a retrans- |
|
plant after previous cava-sparing transplant, the graft can be removed without inter- |
|
fering with IVC flow. |
468 |
SECTION 3 |
Liver |
|
|
|
|
The Anhepatic Stage |
|
|
|
|
STEP 3 |
Removal of the native liver |
|
|
Before completion of the recipient hepatectomy, hemostasis of the retroperitoneal bare |
|
|
||
|
areas is performed using an argon beam coagulator. The bare areas are not routinely |
|
|
oversewn in order to keep the available space for the allograft to the maximum. |
|
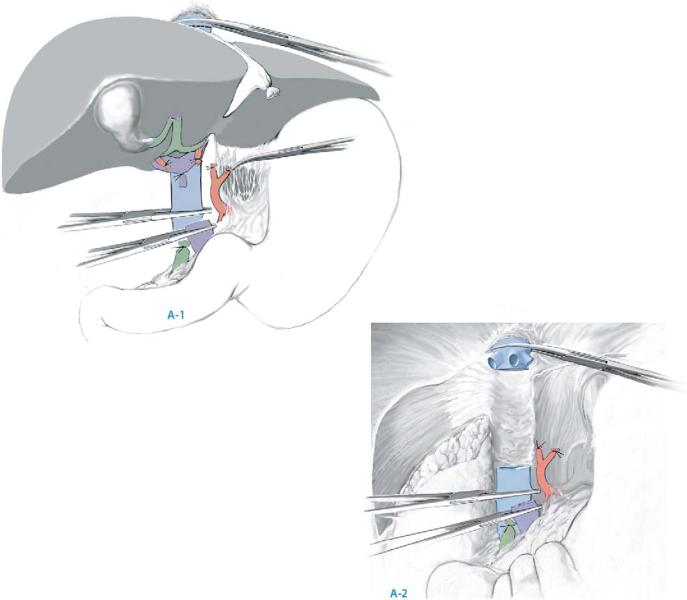
The Classical Technique with Resection of the IVC
Ligate and divide the portal vein as high up into the hilum as possible (A-1). Place vascular clamps on the suprahepatic and infrahepatic IVC and transsect it (A-2).
The Cava-Sparing (or Piggyback) Technique
After clamping and division of the portal vein high up in the liver hilum, the middle and left hepatic veins are clamped and transected and the native liver is removed.
Orthotopic Liver Transplantation |
469 |
|
|
STEP 4 |
Anastomosis of the IVC |
|
The Classical Technique with Resection of the IVC |
|
|
|
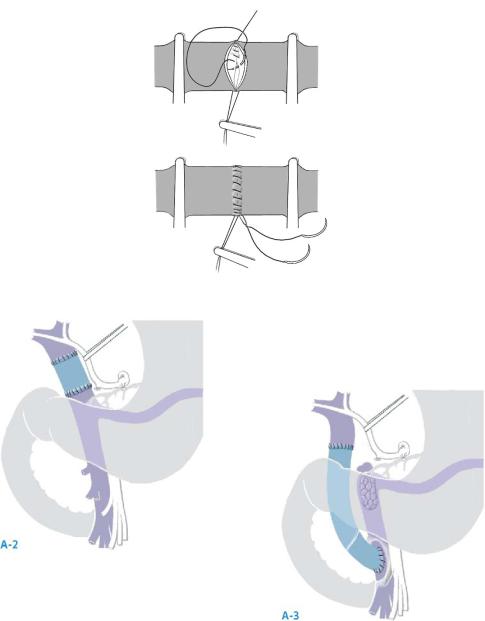
The suprahepatic vena cava of the recipient is sutured to the suprahepatic cava of the |
|
donor liver in an end-to-end fashion, using running polypropylene 3-0. During each |
|
step, the vessel wall is everted to obtain nice endothelium to endothelium apposition. |
|
Identical procedure for the infrahepatic vena cava. A sterile suction catheter can be |
|
positioned in the retrohepatic cava transanastomotically for venting upon. Do not tie |
|
the infrahepatic anastomosis yet (A-1). |
470 |
SECTION 3 |
Liver |
|
|
|
STEP 4 (continued) |
Anastomosis of the IVC |
|
|
|
|
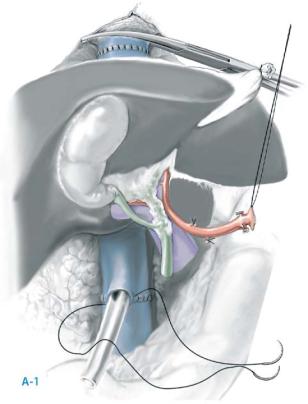
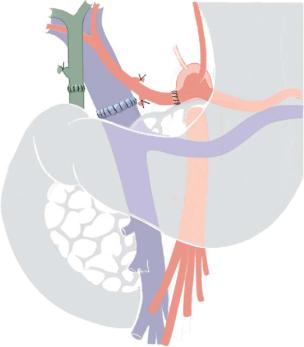
The Cava-Sparing (or Piggyback) Technique
The retrohepatic IVC of the allograft needs careful preparation on the back-table. The upper cava cuff is shortened flush to the hepatic veins. The lower cava cuff of the allograft is shortened up to the level of the first major vein draining segment 1 and subsequently oversewn with a running polypropylene 4-0 or 5-0 suture. A suctioning catheter can be positioned through this suture to facilitate flushing of the liver upon reperfusion (see below).
From here on, three different methods can be used to anastomose the donor and recipient IVC:
a)End-to-end anastomosis. The ostia of the three hepatic veins are interconnected to create a wide opening for the suprahepatic caval anastomosis (A-2) and an end-to- end anastomosis is performed with the suprahepatic IVC of the donor liver (A-3). This technique
is becoming less popular because of the risk of (partial) venous outflow obstruction due to kinking of this relatively narrow anastomosis.
Orthotopic Liver Transplantation |
471 |
|
|
STEP 4 (continued) |
Anastomosis of the IVC |
|
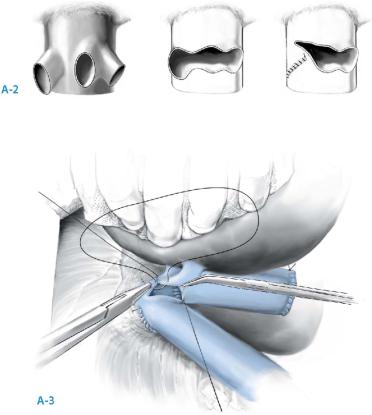
b) Side-to-side cavo-cavostomy. The donor suprahepatic IVC is closed as well with |
|
|
|
running polypropylene 4-0 suture, and a 6-cm-long cavotomy is made on the left |
|
posterior side of the donor IVC. This cavotomy should encompass the orifices of the |
|
major hepatic veins in order to obtain optimal venous allograft drainage and to |
|
permit later procedures such as transjugular biopsy or TIPS placement (A-4). A large |
|
anastomosis is made between the left posterior wall of the donor IVC and the ante- |
|
rior wall of the recipient IVC using partial clamping of recipient IVC (A-4). The anas- |
|
tomosis is performed from the right (or the left) side by using two running sutures of |
|
polypropylene 4-0. This anastomosis is rendered easier using a specially designed |
|
caval clamp. |
|
c) End-to-side cavo-cavostomy. The suprahepatic end of the donor IVC is spatulated |
|
on the dorsal side over 4cm, allowing a wide anastomosis. The anterior wall of the |
|
recipient IVC is partially clamped as described above. A wide (>6cm) anastomosis |
|
is subsequently made between the spatulated suprahepatic IVC of the allograft and |
|
the recipient IVC in an oblique end-to-side fashion, using two running sutures of |
|
polypropylene 4-0 (A-5). An advantage of this technique is that the anastomosis can |
|
be made as wide as possible and that the blood flow from the hepatic veins follows |
|
a more direct course into the IVC, compared to the side-to-side technique. |
472 |
SECTION 3 |
Liver |
|
|
|
STEP 5 |
Anastomosis of the portal vein |
|
|
|
|
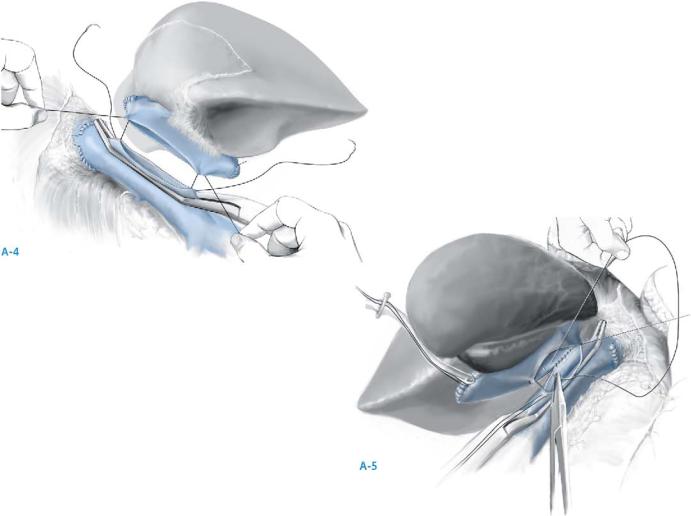
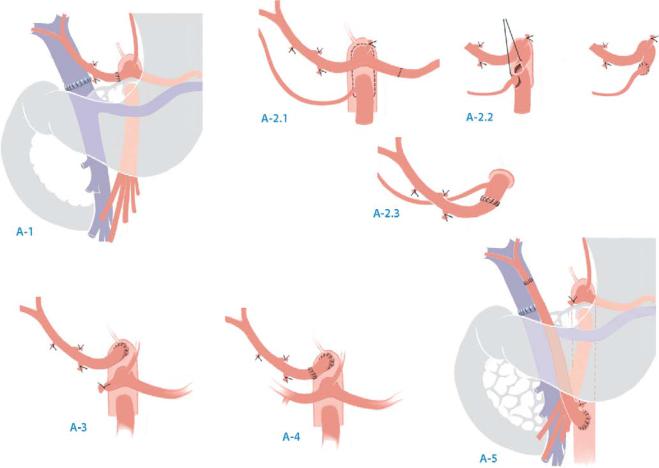
From here on, the procedure is essentially the same for both the classical and the IVCsparing techniques.
After cutting the donor portal vein to adequate length, the portal vein is anastomosed end-to-end, using running polypropylene 5-0 or 6-0. Avoid kinking or rotation and flush the recipient portal vein briefly to remove any clots. Ensure an adequate growth factor of about 3/4 the diameter of the vessel (A-1).
When the recipient portal vein is not suitable for anastomosis (i.e., after longstanding thrombosis), or when the two portal vein stumps are too short, a segment of common iliac vein from the donor can be used to extend the donor portal vein or as a jump graft to the superior mesenteric vein (A-2, A-3). In case of portal vein thrombosis, cannalization can usually be obtained using the eversion thrombectomy technique.
A-1
Orthotopic Liver Transplantation |
473 |
|
|
|
The Post-anhepatic Stage |
|
|
STEP 6 |
Reperfusion of the donor liver |
|
|
Reperfusion can be done in different ways.
■Remove the vascular clamp from the portal vein and reperfuse the liver, flushing 300–400ml of blood via the catheter in the infrahepatic IVC to remove air, preservation solution and potassium from the graft. Remove the catheter in the inferior vena cava and tie the suture at the infrahepatic cava. Subsequently, slowly remove the vascular clamp at the suprahepatic and infrahepatic vena cava (in case of a classical procedure) or the clamp at the anterior aspect of the IVC (in case of a cava-sparing technique).
■When anastomosing the portal vein, the allograft can also be flushed retrogradely via the IVC. Advantage of this technique is complete restoration of the caval venous return to the heart before reperfusion of the graft.
■Once the liver is reperfused, topical irrigation of the liver with warm saline facilitates rewarming.
■Some centers flush the liver with albumin solution prior to reperfusion.
474 |
SECTION 3 |
Liver |
|
|
|
STEP 7 |
Arterial anastomosis |
|
|
|
|
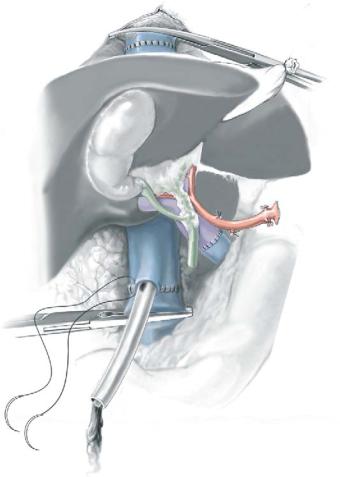
There are several options for the arterial anastomosis. In most cases, an end-to-end anastomosis is made between the common hepatic artery or celiac trunk of the donor and the common hepatic artery or the bifurcation of the left and right hepatic arteries of the recipient, using running or interrupted polypropylene 6-0 or 7-0 (A-1). Depending on the length and diameter of the vessels, alternative sites for anastomosis are possible. The recipient artery should be adequately flushed to remove clots, before completing the anastomosis.
Accessory or aberrant donor arteries should be revascularized by either making a direct anastomosis to the recipient artery or by anastomosing it to the stump of the gastroduodenal artery or splenic artery of the graft (A-2.1, A-2.2, A-2.3).
When the recipient artery is not suitable for grafting (i.e., hepatic artery thrombosis or severe stenosis of the celiac trunk), a segment of iliac artery from the donor should be used as a conduit to make a direct anastomosis with the supratruncal or infrarenal abdominal aorta. In some cases, the donor artery is long enough to make a direct anastomosis between the donor celiac trunk and recipient supratruncal aorta (A-3). When an iliac conduit is used, it can either be anastomosed in an end-to-side fashion to the supratruncal aorta after removal of the native liver (A-4), or to the infrarenal aorta, when the anastomosis is delayed until after reperfusion of the liver via the portal vein (A-5). In the latter situation, clamping of the aorta during construction
of the anastomosis will not interfere with the portal perfusion of the graft.
Orthotopic Liver Transplantation |
475 |
|
|
STEP 8 |
Bile duct reconstruction |
|
The bile duct is shortened on both the donor and the recipient side, until adequate |
|
|
|
bleeding is obtained from both ends. The bile duct anastomosis can be made in an |
|
end-to-end fashion, using interrupted PDS 5-0 to 7-0. An alternative is a side-to-side |
|
anastomosis (as shown in the chapter on biliary anastomoses). A biliary catheter can |
|
be introduced via the recipient common bile duct and placed transanastomotically using |
|
a T-tube. In patients with primary disease of the bile ducts, such as primary sclerosing |
|
cholangitis, the bile duct usually should be reconstructed by a Roux-Y hepatico- |
|
jejunostomy. However, some surgeons would perform a direct duct-to-duct anastomosis |
|
when extrahepatic strictures and inflammation have been excluded. |
|
Before closure, three abdominal vacuum drains are placed (Redon or Jackson |
|
Pratt drain): two subdiaphragmatic drains (one on the left and one on the right side) |
|
and an infrahepatic drain behind the anastomosis. |
476 SECTION 3 Liver
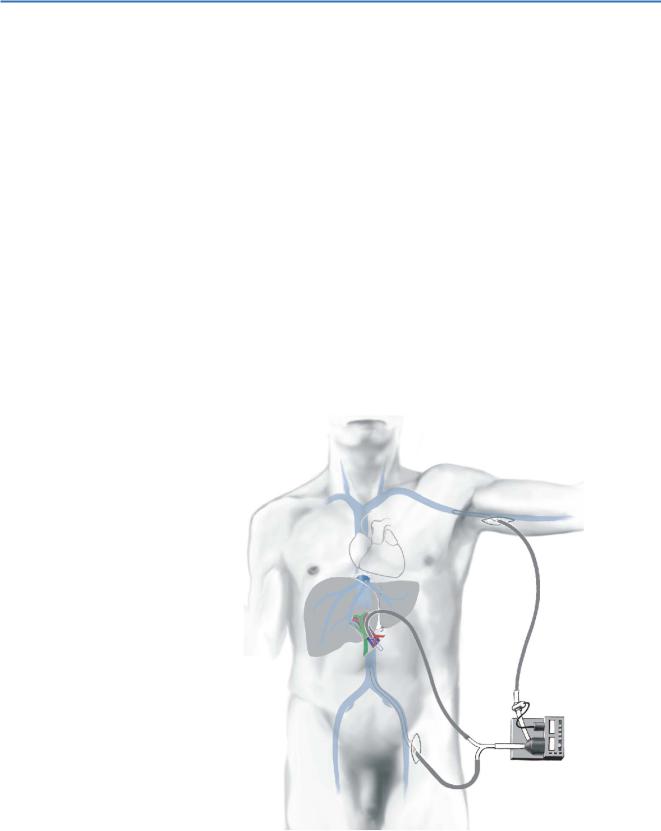
Venovenous Bypass (Optional)
Depending on the center, a venovenous bypass will be used systematically, occasionally, or never. When venovenous bypass is used during the anhepatic stage, this usually includes drainage of (a) the portal vein and (b) the lower part of the body via the left greater saphenous vein into the left axilliary, brachial or internal jugular vein. An alternative for direct cannulation of the portal vein stump is cannulation of the inferior mesenteric vein. The centripetal Biopump with heparin-coated, armed cannulas is the most widely used one. Before use, the cannulas are primed with normal saline or an equivalent solution.
A 6-cm longitudinal incision is made in the left groin, just below Poupart’s ligament, and the proximal end of the greater saphenous vein is isolated and encircled with sutures. After ligation of the distal side, the cannula of the venovenous bypass is inserted via a small venotomy in the proximal side of the greater saphenous vein and advanced into the femoral vein. The portal vein can be cannulated either directly by inserting and securing the cannula into the stump of the recipient portal vein or by cannulation of the inferior mesenteric vein. The axillary vein is cannulated following an identical procedure as for the saphenous vein, via a small longitudinal incision in the left axilla. It is also possible to insert a large bore catheter transcutaneously into the internal jugular vein.
Some centers perform a temporary portosystemic shunt, which will not be covered in this chapter.
