
clavien_atlas_of_upper_gastrointestinal_and_hepato-pancreato-biliary_surgery2007-10-01_3540200045_springer
.pdf436 |
SECTION 3 |
Liver |
|
|
|
|
Procedure |
|
|
|
|
STEP 1 |
Incision, exposure, and staging |
|
|
Access is performed as shown in the chapters on liver resection. Careful exploration |
|
|
|
|
|
of the abdominal cavity is done to exclude extrahepatic disease. The liver should be |
|
|
completely mobilized as for a major liver resection. Since accidental opening of the cyst |
|
|
may occur during mobilization, always have a cup with povidone-iodine (or hypertonic |
|
|
saline solution) ready to use in case of intraoperative spillage of cyst contents. |
|
|
Inspection and manual exploration of both lobes of the liver need to be done with |
|
|
caution. Intraoperative ultrasound using a 5-MHz T-shaped probe is used to assess the |
|
|
number and location of the cysts. Particular attention is directed toward the relationship |
|
|
of the cysts with the portal veins, major hepatic veins, and the vena cava. In addition, |
|
|
meticulous examination of the cyst and the adjacent liver parenchyma can sometimes |
|
|
demonstrate a biliary communication. |
|
|
|
|
STEP 2 |
Definition of the surgical approach |
|
|
Most of the cysts located in the right liver are easy to dissect away from the diaphragm. |
|
|
||
If not safely feasible, a partial resection of the diaphragm must be performed.
In case of major vascular involvement or with invasion of the left or right hepatic duct, an anatomical liver resection is indicated.
In case of a cyst located deep within the liver, liver resection is also recommended. However, when depth from the liver surface is less than 2–3cm, a hepatotomy allows the cyst to be reached and a standard pericystectomy can be performed.
For cysts located close to the vena cava in segments 6 or 7, the liver needs to be mobilized as for a right hepatectomy.
Pericystectomy for Infectious Liver Cyst |
437 |
|
|
|
|
STEP 3 |
Preparation prior to pericystectomy |
|
|
|
|
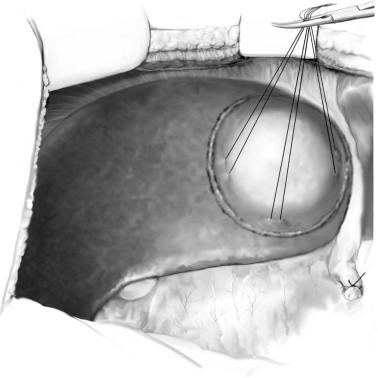
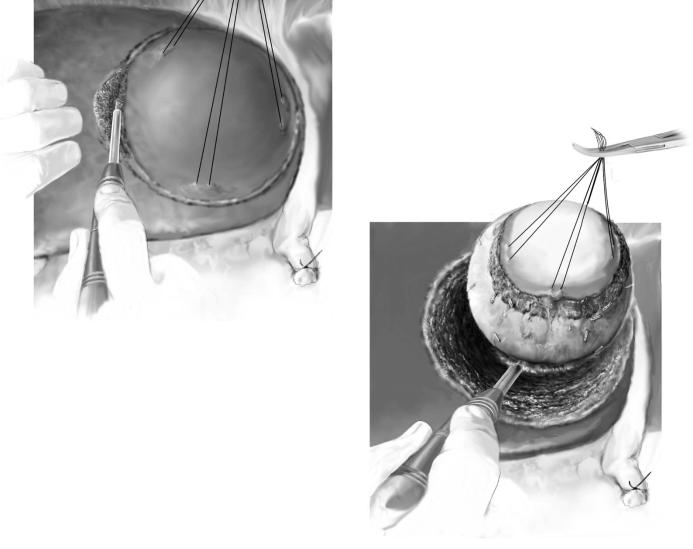
The central venous pressure should be below 3mmHg before starting the liver transection. A tourniquet is placed around the porta hepatis for inflow occlusion in case of bleeding. To prevent accidental spillage of the cyst contents, the whole space around the liver is packed using gauze swabs. A pack placed behind the right liver usually offers better exposure. The contents of the cyst should never be evacuated before resection. Stay sutures should not be placed in the cyst wall. However, stay sutures with silk 2-0 are placed in the liver parenchyma around the emerging part of the cyst to enable traction and better exposure during resection.
438 |
SECTION 3 |
Liver |
|
|
|
STEP 4 |
Resection of the cyst |
|
|
|
|
The liver capsule is incised with diathermy. Careful identification of the correct plane of cleavage is crucial to avoid bleeding or spillage of the cyst contents (A). Intrahepatic vessels are coagulated selectively with bipolar forceps or ligated with metallic clips, ties or suture-ligatures depending on the diameter. Although several possible techniques for liver parenchyma dissection can be used (see chapter “Techniques of Liver Parenchyma Dissection”), we prefer the water jet, which enables a selective and safe separation of the cyst wall from the liver parenchyma (B). Small bile ducts should be carefully identified and tied. Hemostasia of the exposed raw surface of the liver can be improved with argon beam coagulator or topical fibrin derivates.
A
B
Pericystectomy for Infectious Liver Cyst |
439 |
|
|
Postoperative Complications
■Same complications as in liver resections
■Biliary fistula is less common than in partial resection
Tricks of the Senior Surgeon
■Use magnification loops to control bile leaks after pericystectomy. Careful repair should be done with suture-ligatures with Prolene 4-0 to 5-0.
■At least two drains with powerful suction should be available in case of rupture of the cyst to avoid peritoneal spread of the contents.
■Always have a cup with povidone-iodine (or hypertonic saline solution) ready to use in case of intraoperative spillage of cyst contents into the peritoneal cavity.
■In case of intraoperative bleeding and technical difficulties during surgery, remember that adequate conservative surgery (e.g., partial resection of the cyst) can also achieve excellent results. The strategy can be changed anytime!

Special Maneuvers in Liver Trauma
Denis Castaing, Olivier Scatton, Marius Keel
Introduction
Liver injuries most often (>90% of all cases) are associated with other injuries such as ipsilateral rib fractures, lung contusions, other intra-abdominal lesions, or injuries of the extremities, the pelvis and the head. Hepatic injuries are graded according to the Organ Injury Scale of the American Association for the Surgery of Trauma (AAST-OIS) (Table1).
Because clinical examination of the abdomen is unreliable in trauma patients with an altered level or loss of consciousness, a Focused Assessment with Sonography for Trauma (FAST) should be undertaken as an adjunct to the primary survey. In hemodynamically unstable patients with free fluid in FAST, a diagnostic laparotomy without further investigation is indicated. In stable patients, CT scanning of the abdomen represents the gold standard with evaluation of hemoperitoneum, parenchymal fractures, as well as vascular mapping including a three-phase study (arterial, portal and venous) as a preparation for a possible arterial embolization. The decision for operative or non-oper- ative management of blunt hepatic trauma after CT scan is made according to the grade of liver injury and diagnosed or suspected other abdominal injuries, whereas for penetrating abdominal injuries an operative exploration of the abdomen is still standard.
Table 1. Grading of hepatic injuries according to the Organ Injury Scale of the American Association for the Surgery of Trauma (AAST-OIS)
Grade |
Injury description |
Incidence |
Mortality |
|
|
|
|
I |
Subcapsular hematoma, <10% surface area |
20% |
0% |
|
Capsular tear, <1cm in depth |
|
|
II |
Subcapsular hematoma, 10–50% surface area |
55% |
<10% |
|
Intraparenchymal hematoma, <10cm in diameter |
|
|
|
Laceration, 1–3cm in depth, <10cm in length |
|
|
III |
Subcapsular hematoma, >50% surface area expanding |
15% |
25% |
|
or ruptured with bleeding |
|
|
|
Intraparenchymal hematoma, >10cm in diameter |
|
|
|
or expanding |
|
|
|
Laceration, >3cm in depth |
|
|
IV |
Parenchymal disruption involving 25–75% of lobe |
7% |
45% |
|
or one to three segments |
|
|
V |
Parenchymal disruption of >75% of lobe |
3% |
>80% |
|
or more than three segments |
|
|
|
Juxtahepatic venous injury |
|
|
VI |
Hepatic avulsion |
<1% |
Near 100% |
|
|
|
|

442 |
SECTION 3 |
Liver |
|
|
|
|
Non-operative Management |
|
Liver injuries grade I–III should be treated non-operatively. In case of active bleeding (diagnosed by CT scan), an angiographic embolization should be performed in patients with injuries grade I–IV. However, the following conditions should be fulfilled:
■Patient without altered level or loss of consciousness
■Hemodynamic stability or rapid stabilization after initial fluid resuscitation
■Exclusion of hypothermia, acidosis or severe coagulopathy
■No doubt about another abdominal lesion
■Intensive care unit available with continuous pulse and arterial blood pressure monitoring, repeated measurements of Hb, Hct and coagulation parameters, and careful follow-up clinical examination and sonography
■Availability of a surgical team
■Arteriography and experienced radiologist available
Indications and Contraindications
Indications for Laparotomy ■ Hemodynamic instability
■Peritonitis on physical examination
■Other abdominal injuries in diagnostic studies
■Failed non-operative treatment
Special Maneuvers in Liver Trauma |
443 |
|
|
|
Procedure |
|
|
STEP 1 |
Incision and abdominal exploration |
|
|
A midline incision and, depending on the type of injury, an extension into the chest by median sternotomy or left or right thoracotomy is performed. The initial step in a trauma laparotomy is to pack all four quadrants of the abdomen in order to control hemorrhage as quickly as possible. The next step is to determine the site(s) of bleeding and injuries by exploration of the whole abdomen with special attention to the pancreas and the right retroperitoneal area. Packs are removed from one quadrant at a time, starting in the non-injured area and ending in the most seriously injured area. Injuries of the small or large bowel and of the biliary tree are repaired.
In addition, a rapid transfusion device with warmed crystalloids and blood is essential. After exclusion of hollow organ injuries, blood should be collected in the peritoneal cavity for autotransfusion (cell saver). Dilutional coagulopathy may follow massive blood transfusions, prompting the need for transfusion of platelets, fresh frozen plasma and/or activated factor VII.
In general, three situations can be found after laparotomy:
1.Diffuse severe active bleeding or cardiac arrest at the opening:
The control of massive exsanguinating hemorrhage requires clamping of the aorta and/or inferior vena cava (IVC). Aortic control can be approached through a sternotomy or left thoracotomy allowing supradiaphragmatic, intrathoracic aorta cross-clamping and open cardiac massage in situations with cardiac arrest. This is
predictable if an external cardiac massage on a “dying person with a tense abdomen” is performed. Furthermore, the suprarenal abdominal aorta can be approached through the gastrohepatic ligament or after medial rotation of the splenic flexure
of the colon (Mattox maneuver). The infradiaphragmatic IVC can be controlled by direct digital pressure or clamping after an extended Kocher maneuver or right side to medial visceral rotation (Cattel Braasch maneuver).
2.No active bleeding from the liver:
Simple hepatic injuries such as grades I, II or III without active bleeding do not require further operative investigation or treatment.
3.Active bleeding from the liver: Proceed with Step 2.

444 |
SECTION 3 |
Liver |
|
|
|
STEP 2 |
Manual compression of the liver |
|
|
|
|
In case of active hemorrhage from the liver, the surgeon or ideally the assistant performs initial tamponade by manual compression for at least 10min.
Then, two situations can be found:
1.When the hemorrhage can be controlled by manual compression, a competent team is available for appropriate assessment, and the patient is hemodynamically stable without hypothermia or acidosis, a one-step intervention leading to definitive surgical repair can be decided (see step 3).
2.When the hemorrhage is not controllable and hemodynamic instability, hypothermia, acidosis and coagulopathy occur, a liver packing (see step 9) with or without vascular control (see step 10) needs to be performed.

Special Maneuvers in Liver Trauma |
445 |
|
|
STEP 3 |
Mobilization of the liver |
|
The liver can be fully mobilized to facilitate the examination and exploration of the |
|
|
|
posterior surface and the retrohepatic vena cava. It must be carefully done to avoid |
|
hepatic vein damage. After dissection of the falciform ligament, the right triangular, |
|
the coronary and the left triangular ligaments are divided while the assistant is taking |
|
care of the fracture by manual compression. |
446 |
SECTION 3 |
Liver |
|
|
|
STEP 4 |
Risk of hepatic vein damage during liver mobilization |
|
|
|
|
When liver packing is needed (step 9), hepatic mobilization is not recommended since this maneuver increases the risk of hepatic vein damage and aggravates the initial liver injury.
Major hepatic lesions are usually caused by a deceleration trauma leading to a liver fracture at the level of the right triangular ligament along the right hepatic vein. This location is often difficult to access. To stop the bleeding, the fracture should be closed by placing the assistant’s hand beyond the fracture, while traction should be avoided.
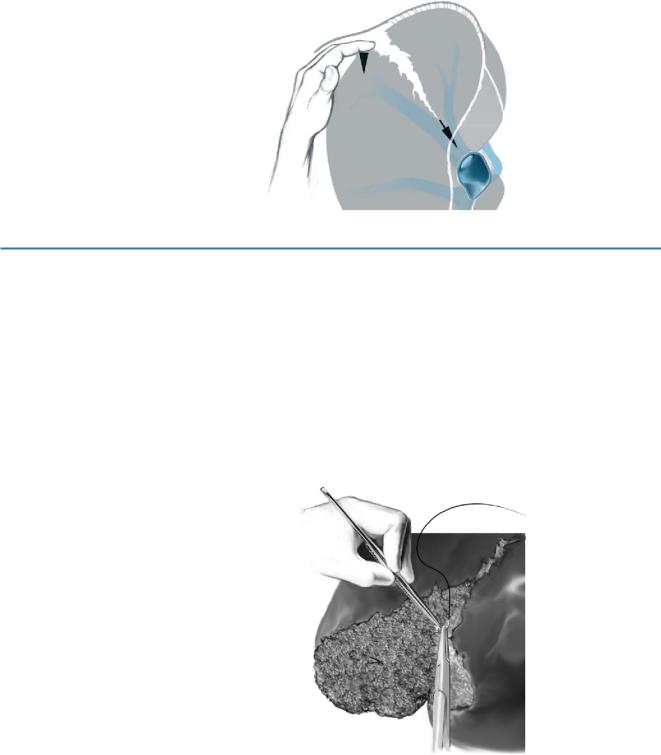
STEP 5 |
Vascular ligation |
|
The wound may require enlargement to visualize the source of bleeding by utilizing |
|
|
|
finger-fracture technique and retractors (hepatotomy). Bleeding vessels can be |
|
controlled using sutures, surgical clips, and electrocautery. However, deep stitches, which |
|
could lead to ischemic areas, should be avoided. |
|
While a Pringle maneuver might be required, prolonged pedicle clamping must be |
|
avoided whenever possible as it may aggravate ischemic injury caused by hypotension. |
|
If pedicle clamping longer than 30min is needed, intermittent clamping is recom- |
|
mended (15 min of clamping and 5min of reperfusion). |
|
Hepatic defects can be filled by vascularized omentum (omentoplasty). This helps |
|
to eliminate dead space, tamponades venous oozing and may reduce the risk of a |
|
significant bile leakage. |
