
clavien_atlas_of_upper_gastrointestinal_and_hepato-pancreato-biliary_surgery2007-10-01_3540200045_springer
.pdf394 |
SECTION 3 |
Liver |
|
|
|
|
Procedures |
|
|
Left Lateral Sectionectomy (bisegmentectomy 2, 3) |
|
|
This is the most common anatomic liver resection performed laparoscopically. |
|
|
|
|
STEP 1 |
Access, exploration, and mobilization of the left lateral section |
|
|
After placement of the ports, the liver is explored by laparoscopic ultrasound to deter- |
|
|
||
|
mine the size and location of the tumor, to detect additional lesions and to assess the |
|
|
quality of surrounding liver tissue as well as the feasibility of the laparoscopic resection. |
|
|
First, the round, the falciform, and the triangular ligament need to be divided and the |
|
|
lesser omentum is opened. The dissection of the falciform ligament is pursued to the |
|
|
inferior vena cava at the level of the insertion of the hepatic veins. The left triangular |
|
|
and coronary ligaments are divided. |
|
|
|
|
STEP 2 |
Preparation for the Pringle maneuver and parenchymal transection |
|
|
A tape is placed around the porta hepatis and passed through a 16-Fr rubber drain to be |
|
|
||
|
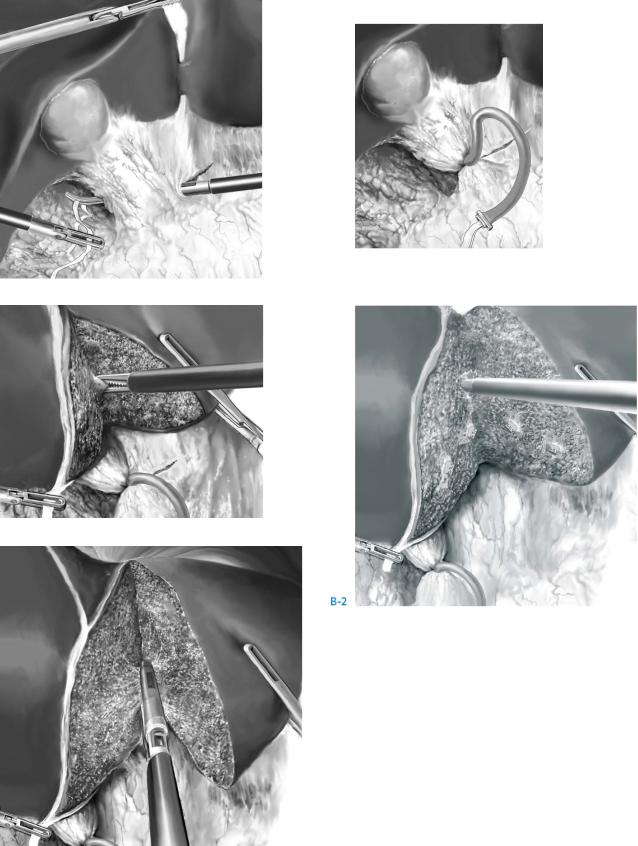
used as a tourniquet secured by a clip (A-1, A-2). The Pringle maneuver is not applied |
|
|
systematically but is used when required to reduce hemorrhage during transection. |
|
|
When present, an additional left hepatic artery originating from the left gastric artery |
|
|
should be either clamped or ligated and divided. Parenchymal transection follows the |
|
|
left margin of the round and falciform ligament from the anterior edge of the left lateral |
|
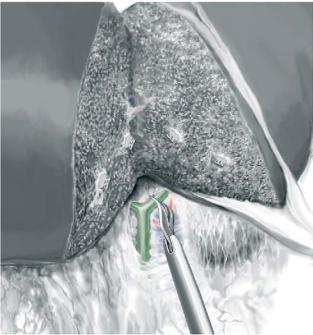
section up to the level of the origin of the left hepatic vein (B-1). The exposure during transection is maintained by traction of the round ligament towards the right and traction of an atraumatic forceps on the left lateral segment to the left. It is important that the line of transection remains on the left side of the ligaments to avoid injury to the pedicles of segment 4. Posteriorly, the line of transection follows the anterior margin of the Arantius’ ligament. The technique of parenchymal transection includes division of the liver with step-by-step control and division of the encountered pedicles. In case of a parenchymal bridge covering the inferior aspect of the round ligament, it should be divided first. A harmonic scalpel is used for the superficial transection (the initial 2–3cm of depth) for structures up to 3mm in diameter. Its advantage lies in the ability to cut and coagulate simultaneously. However, it is a blind instrument which becomes more hazardous in the depth of the liver with a risk of injury to larger vessels.
Deeper vessels must be identified before division, and a CUSA with laparoscopic extended hand piece is the recommended device (B-2). Bipolar cautery is used for minor vessels while structures larger than 3mm in diameter are clipped before division. We do not recommend the use of the argon beam coagulator during laparoscopy because severe gas embolisms due to sudden hyperpressure have been reported.
Portal pedicles to Segments 2 and 3 can be divided using a linear stapler. Stapler application must be performed on the left side of the round ligament (C).
Laparoscopic Liver Resection |
395 |
|
|
STEP 2 (continued) |
Preparation for the Pringle maneuver and parenchymal transection |
|
|
A-2
A-1
B-1
C
396 |
SECTION 3 |
Liver |
|
|
|
STEP 3 |
Transection of the left hepatic vein and extraction of the specimen |
|
|
|
|
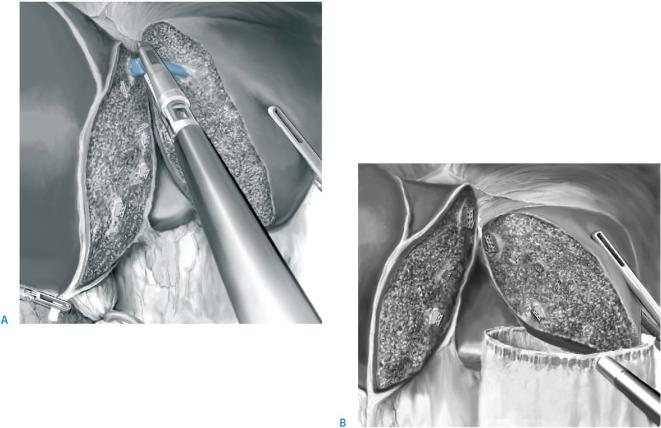
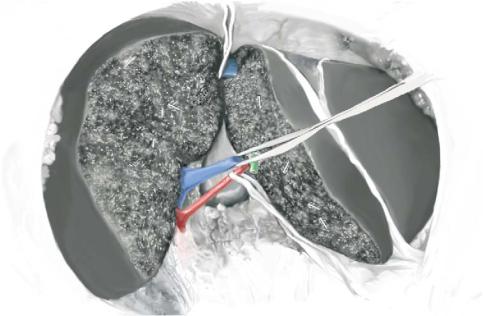
Once the portal pedicles have been divided, an ultrasonic dissection can progress cephalad to identify the left hepatic vein, which can then be divided using the same linear stapler, finishing the transection (A).
Additional hemostasis or biliostasis of the transected surface can be achieved by cautery, further clipping or suturing.
A 5-cm incision is usually sufficient for a left lateral section specimen. The incision can be a previous appendectomy incision or a suprapubic incision. At the chosen location, skin and subcutaneous incisions are made without incising the fascia to maintain the pneumoperitoneum. A 15-mm trocar is inserted under internal visual control for the insertion of a large specimen bag (B). The specimen is placed in the bag, which is then extracted with the 15-mm trocar. CO2 insufflation is stopped and the fascia is incised to allow externalization of the bag. After reinsufflation, hemostasis is checked again and completed if necessary. CO2 pneumoperitoneum is vented as completely as possible to reduce postoperative pain and the fascia of port sites >5mm is carefully closed with absorbable suture material.
Laparoscopic Liver Resection |
397 |
|
|
|
Non-anatomical or Wedge Resection for a Peripheral Lesion |
|
These resections are for small lesions located on the edge of the anterolateral segments |
|
of the liver (i.e., Segments 3–6). |
|
The liver is exposed and explored as for a left lateral sectionectomy. Although a |
|
Pringle maneuver is rarely necessary for these types of resections, it is a safety measure |
|
to prepare for the possibility of clamping in case of bleeding. The preparation is the |
|
same as for the left lateral sectionectomy. |
|
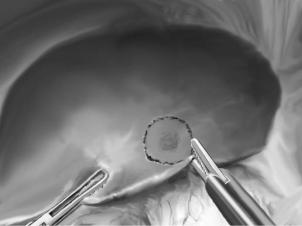
Resection limits are marked on the liver surface with electrocautery. No wide margins |
|
are required in case of benign lesion, while a 10-mm margin is recommended for malig- |
|
nant tumors of the liver. |
|
Parenchymal transection follows the margins marked on the liver surface by cautery. |
|
Since this is a peripheral resection, the harmonic scalpel (Ethicon EndoSurgery) is |
|
usually very convenient and sufficient. Additional hemostasis is achieved by bipolar |
|
cautery and according to the size of the encountered pedicles. Staplers are usually |
|
unnecessary except for pedunculated lesions, whose pedicles can be divided by stapler |
|
applications. |
|
The specimen is extracted as shown for the left lateral sectionectomy. While the size |
|
of the incision should be adapted to the specimen, port sites >5mm need to be sutured. |
398 |
SECTION 3 |
Liver |
|
|
|
|
Laparoscopic Living Donor Left Lateral Sectionectomy |
|
|
for Liver Transplantation in Children |
|
|
This procedure consists of a laparoscopic left lateral sectionectomy without vascular |
|
|
clamping or division in order to minimize parenchymal ischemia. General principles |
|
|
of patient installation and instrumentation are the same as for the left lateral section- |
|
|
ectomy. The mobilization is the same as for a conventional left lateral sectionectomy. |
|
|
For open living donor left lateral sectionectomy see chapter by Tanaka and Egawa. |
|
|
|
|
STEP 1 |
Preparation of the left portal pedicle |
|
|
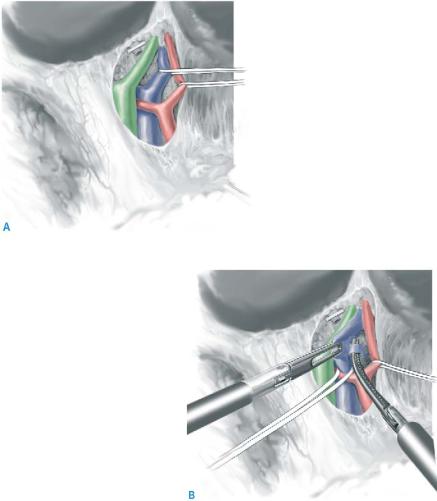
The left arterial and portal branches are dissected, encircled, and marked with a vascular |
|
|
||
|
band in the hepatoduodenal ligament (A). Arterial and portal branches to segment 1 are |
|
|
divided between clips (B). |
|
Laparoscopic Liver Resection |
399 |
|
|
STEP 2 |
Parenchymal transection |
|
In contrast to the conventional resection of the left lateral section, the parenchymal |
|
|
|
transection for living donation needs to be performed along the right aspect of the falci- |
|
form ligament. The harmonic scalpel is used for the superficial part of the transection |
|
and the CUSA for deeper transection. Bleeding is controlled only by using bipolar |
|
cautery and clips without any vascular clamping. Segment 4 portal pedicles are divided |
|
inside the liver parenchyma with a linear stapler or clips depending on their size. |
|
|
STEP 3 |
Left bile duct division |
|
Once parenchymal transection has reached the hilar plate and the left hepatic duct |
|
|
|
becomes visible, the left bile duct is divided using sharp scissors. Its proximal stump |
|
is sutured using absorbable running sutures (PDS 5-0). |
400 |
SECTION 3 |
Liver |
|
|
|
STEP 4 |
End of transection and isolation of the left hepatic vein |
|
|
|
|
After bile duct division, transection progresses cephalad with section of Arantius’ line and progressive dissection of the left hepatic vein. At that stage, the graft is only attached by its vessels.

Laparoscopic Liver Resection |
401 |
|
|
STEP 5 |
Graft harvesting |
|
An 8–10cm suprapubic, transverse incision is performed in order to extract the left lobe |
|
|
|
to be transplanted. Only the skin and subutaneous tissue are opened and a 15-mm trocar |
|
is inserted to fit the extraction bag. The left lobar arterial branch is clipped and divided. |
|
The left portal branch is then divided initiating warm ischemia. In order to preserve an |
|
adequate length of the left portal vein, an Endo-TA stapler (endoTA, Tyco, USA) with |
|
one-sided stapling on the remaining donor liver side is used. In addition, a bulldog is |
|
placed on the side of the graft in order to prevent bleeding. Finally, the left hepatic vein |
|
is stapled with the same one-sided stapling device. |
|
The graft is placed in the bag and extracted through a suprapubic incision after incision |
|
of the fascia as for a conventional left lateral sectionectomy. |
|
The graft is handed to another team for perfusion with the preservation solution. |
|
Warm ischemic time is usually less than 10min. |
|
Final hemostasis and biliostasis remain the same as for the conventional left lateral |
|
resection. |
402 |
SECTION 3 |
Liver |
|
|
|
|
Tricks of the Senior Surgeon |
|
■Laparoscopic hepatectomy is a difficult procedure requiring expertise in both hepatic and laparoscopic surgery. This may require the association of two surgeons.
■In cases of technical difficulty such as persistent bleeding, insufficient exposure or vision, the risk of tumor rupture or insecurity with respect to the tumor margin, one should convert to an open procedure. A conversion, in contrast to a less than optimal outcome, is not a failure of the procedure.
■Abdominal pressure of less than 12 might reduce the risk of gas embolism.
■Before new tools become available, a combination of harmonic scalpel and ultrasonic aspirator is the recommended combination for laparoscopic parenchymal transection.

Cryosurgery
Koroush S. Haghighi, David L. Morris
The goal of hepatic cryosurgery is complete destruction of tumors for curative or palliative reasons as an alternative to resection where resection is not feasible.
Indications and Contraindications
Indications |
Malignant liver tumors in the case of: |
|
|
■ |
Cirrhosis – if risk of resection is excessive |
|
■ |
Bilobar disease where resection would not leave enough hepatic parenchyma |
|
■ |
Debulking of neuroendocrine tumors |
|
■ |
As an adjunct to resection (i.e., resect one side and cryoablate the other side) |
|
■ |
Edge cryotherapy when resection margins are less than 1cm |
|
|
Non-resectable extrahepatic disease (except neuroendocrine tumors) |
Contraindications |
■ |
|
|
■ |
High number of lesions (i.e., > nine lesions; other centers may consider > five lesions |
|
|
as a contraindication) |
|
■ |
Tumors >5cm |
|
■ |
Synchronous bowel resection and hepatic cryoablation (increased risk of liver |
|
|
abscess) |
Preoperative Investigation and Preparation for the Procedure
In addition to the preoperative investigations before liver resections:
■In the case of neuroendocrine tumors: H1 and H2 blockers and somatostatin (double existing dose or 100mg twice daily if not on it) 48h preoperatively
■Bowel preparation (facultative)
■Make sure there is liquid N2 in the machine
