
clavien_atlas_of_upper_gastrointestinal_and_hepato-pancreato-biliary_surgery2007-10-01_3540200045_springer
.pdf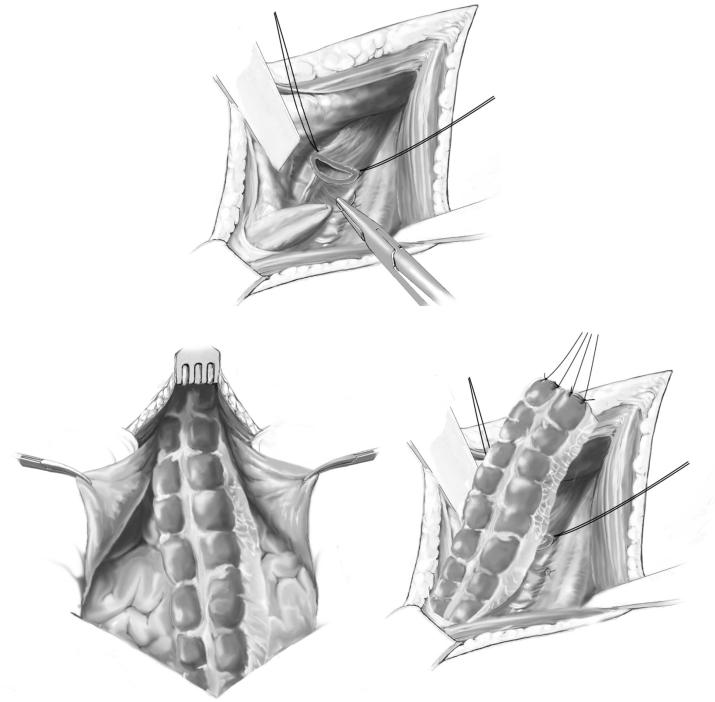
204 |
SECTION 2 |
Esophagus, Stomach and Duodenum |
|
|
|
STEP 18 |
Pull-through procedure |
|
|
|
|
For the substernal reconstruction, a long strong suture fixed to a drainage tube can be used for the pull-through procedure. The suture is tied to the oral end of the colonic interposition. The colon is transposed in the substernal tunnel to the cervical incision under a continuous and gentle pull, and the sternum should be pulled upwards with a sharp retractor during the procedure (A-1, A-2, A-3).
A-1
A-2
A-3
Transhiatal Esophagogastrectomy |
205 |
|
|
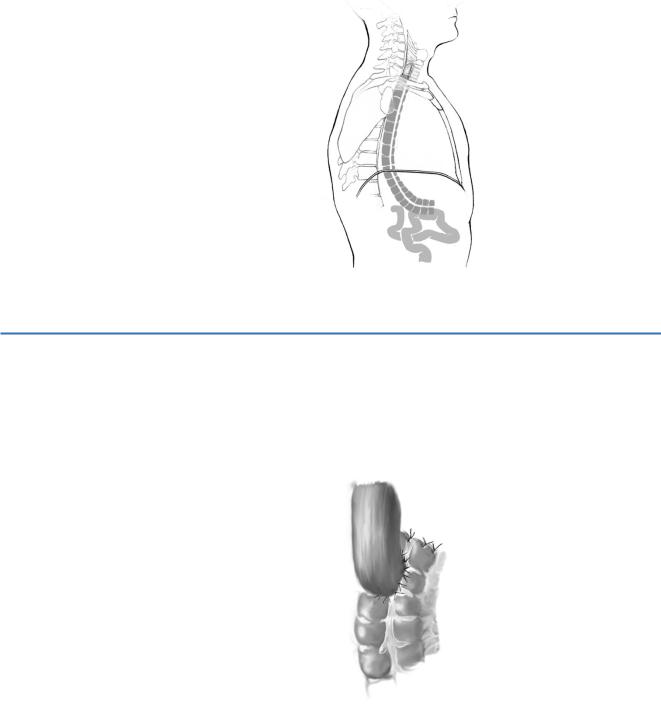
STEP 19 |
Posterior mediastinum |
|
Interposition of the colon through the posterior mediastinum is performed in the bed of |
|
|
|
the removed esophagus. The posterior mediastinal route of the interposed colon is |
|
favorable to the substernal or presternal position because of the shorter distance to the |
|
neck. In addition, the posterior mediastinal route prevents kinking of the colon and |
|
leads to better functional results. The interposed colon causes hemostasis in the opera- |
|
tion field. |
STEP 20 |
Terminolateral anastomosis |
|
If possible, the terminolateral anastomosis should be performed in a double row |
|
|
|
suture technique. |
|
In case of a different lumen diameter, single stitches and a terminolateral |
|
anastomosis can be performed close to the taenia libera. |
206 |
SECTION 2 |
Esophagus, Stomach and Duodenum |
|
|
|
STEP 21 |
Laterolateral anastomosis |
|
|
|
|
The alternative technique for anastomosis after colonic interposition is a laterolateral colo-esophageal anastomosis performed by a linear stapler.
STEP 22 |
Reconstruction of the intestine |
|
Gastrointestinal continuity is achieved by descendojejunostomy and jejunojejunostomy. |
|
|
|
A caecosigmoidostomy completes the reconstruction. The mesenteric incisions have |
|
been closed. The operative site after transposition of the colon and reconstruction is shown. |
Transhiatal Esophagogastrectomy |
207 |
|
|
Combined Transhiatal Transthoracic Esophagectomy
Introduction
We reported this technique for the first time in 1980. It uses the concepts acquired in transhiatal dissection in tumors located more superiorly in the cervicothoracic esophagus or in the middle third of the thoracic esophagus, and avoids a “blunt” dissection performed without visual control, which increases the possibility of iatrogenic injury to mediastinal structures. However, at present more and more surgeons favor transhiatal esophagectomy for its technical simplicity and favorable outcome.
|
Indications and Contraindications |
|
■ Esophageal carcinoma in the mid or upper third after subtotal gastrectomy |
Indication |
|
|
See page 189. |
Contraindications |
|
|
Preoperative Investigations/Preparation for Procedure |
|
See page 189. |
|
■ Bronchoscopy |
208
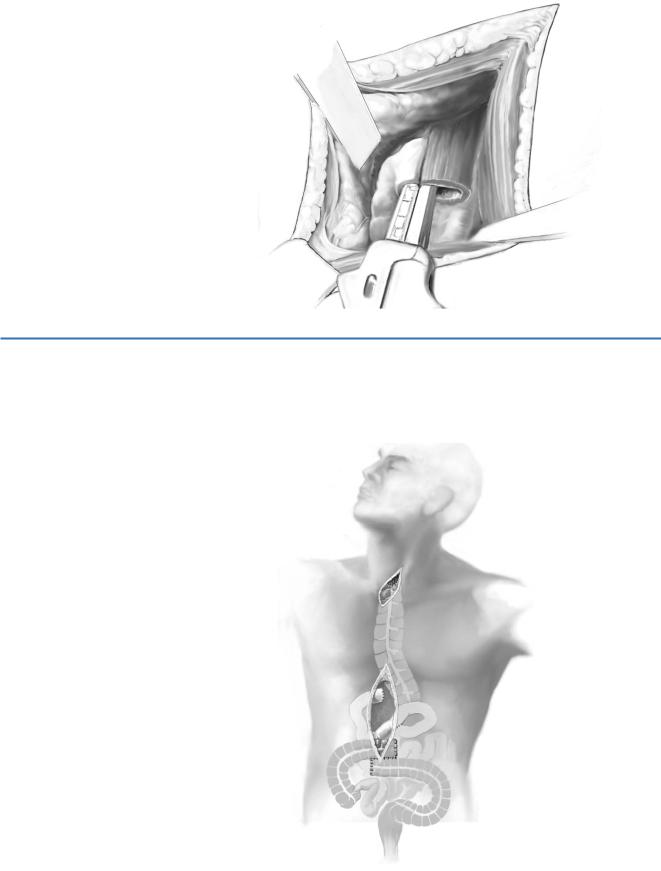
STEP 1
STEP 2
STEP 3
SECTION 2 |
Esophagus, Stomach and Duodenum |
Procedure
Access
See chapter on “Subtotal En Bloc Esophagectomy: Abdominothoracic Approach”.
Abdominal exposure
The operation begins with a supraumbilical medial laparotomy, and the abdominal viscera and diaphragmatic section are examined (see above), which permits access to the posterior mediastinal space. The mediastinal section is done as for the previous patient, allowing visual control as far as the tracheal branching.
Right anterior thoracotomy
A right anterior thoracotomy is then performed, if possible without costal resection. If the rigidity of the thorax so requires, the anterior arch of the costal vein is removed, and should this prove insufficient, the remaining posterior arch of this rib is resected via the anterior thoracic incision.
Esophageal dissection and mediastinal lymphadenectomy
The ipsilateral mediastinal pleura, which remains in contact with the esophagus, is incised through the anterior thoracic incision. The arch of the azygos vein is incised, enabling the dissection of the cervicothoracic esophagus. To expand the mediastinal lymphadenectomy, this incision is used to dissect the intercostal veins. The trunk of the azygos vein is ligated at the supradiaphragmatic level and associated thoracic duct excision is required by the lymphatic involvement.
During esophageal dissection at the high level of the cervical region, a tracheobronchial intubation with a Carlens tube can be used to facilitate access to the esophagus, occluding the right bronchial tube (see Chapter “Abdominothoracic Esophagectomy” STEP 1–3).
Transhiatal Esophagogastrectomy |
209 |
|
|
STEP 4 |
Technique of cervical anastomosis |
|
See chapter on “Transhiatal Esophagogastrectomy.” |
|
|
|
|
STEP 5 |
Technique of high intrathoracic esophagocolostomy |
|
See chapter on “Abdominothoracic En Bloc Esophagectomy with High Intrathoracic |
|
|
|
Anastomosis.” |
210 SECTION 2 Esophagus, Stomach and Duodenum
Standard Postoperative Investigations
See chapter on “Subtotal Esophagectomy: Transhiatal Approach.”
Postoperative Complications
Early Postoperative Course
■Pulmonal infections
■Septic complications: subphrenic or intra-abdominal abscess; cervical wound infection
■Anastomotic leak
■Necrosis of the interposition
■Enterothorax
Late Postoperative Course
■Cicatricial strictures of the cervical esophagoor pharyngeo-colostomy, mostly due to anastomotic leak
■Kinking of the interposition
■Mechanical trauma to a subcutaneous graft, which often needs surgical intervention
■Propulsive disorder
Tricks of the Senior Surgeon
■Treatment of the stenosis is performed by bougienage or balloon dilatation. Very rarely is surgical intervention indicated.
■Reasons for necrosis of the interposition are: decrease of circulation due to kinking or compression of the main vessels, hypovolemia, and hypercoagulability. Avoidance is by interposition of a long colonic segment without tension. Optimization of the postoperative hemodynamic and rheologic parameters is necessary.
■Kinking of the interposition is a rare but dangerous complication, which often requires surgical intervention, due to clinical symptomatic disturbance of the gastrointestinal passage by elongation of the interposition. Surgical intervention is performed by shortening of the graft.
■To avoid enterothorax phrenicotomy has to be performed.
Laparoscopic Gastrectomy
Geert Kazemier, Johan F. Lange
Introduction
Laparoscopic resection of the stomach should mimic an open operation as closely as possible. This is applicable to the technique, as well as to the considerations on which the indication is based. Palliative resection for gastric malignancy can be indicated to prevent hemorrhage or obstruction.
Indications and Contraindications
Indications |
■ |
Malignant tumors [carcinoma, gastrointestinal stromal tumor (GIST)] |
|
■ |
Benign tumors (e.g., GIST, apudoma) |
|
■ |
Arteriovenous malformations |
|
■ |
Recurrent peptic ulcer disease |
|
|
Severe cardiac failure (unable to withstand pneumoperitoneum) |
Contraindications |
■ |
|
|
■ |
Sepsis |
|
■ |
Severe coagulopathy |
|
■ |
Morbid obesity (BMI>40) (relative) |
|
■ |
Previous upper abdominal surgery (relative) |
|
■ |
T4 or bulky tumors (relative) |
Preoperative Investigation/Preparation for the Procedure
See chapter “Total Gastrectomy with Conventional Lymphadenectomy.”
Instrumentation
■Two monitors
■Three 10to 12-mm trocars, two 5-mm trocars
■One 15-mm trocar (optional) to pass the 60-mm stapler and retrieval bag
■30° laparoscope
■Unipolar or bipolar coagulation
■Hemostatic device (LigaSure, Ultracision)
■Standard laparoscopic instruments for advanced laparoscopic surgery, including fenestrated clamps and endo-Babcock clamp
■Vascular clip applier
■Endostapler (45–60mm, with white, blue and green cartridges)
■Liver retractor
■Vessel loops
■Gastroscope (optional, to identify small lesions)
■Retrieval bag
212 |
SECTION 2 |
Esophagus, Stomach and Duodenum |
|
|
|
|
Procedure |
|
|
|
|
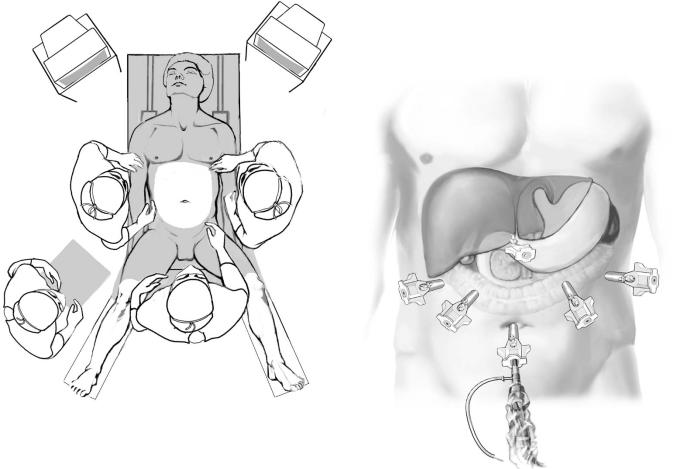
STEP 1 |
Positioning and installations |
|
|
Positioning: |
|
|
|
The patient is placed in the supine position. The surgeon stands between the legs of the patient, the first assistant on the left, the second assistant on the right side of the patient. The scrub nurse is positioned on the right or left hand side of the surgeon (A).
Installation of pneumoperitoneum and inspection of abdominal cavity: Pneumoperitoneum is installed at the site of the umbilicus. In obese patients, the
umbilicus is located more caudally; in these patients the first trocar may be introduced cranially to the umbilicus. In case of malignancy the abdominal cavity is inspected for signs of dissemination to the peritoneum or other organs. To allow for optimal inspection and to create the opportunity to take biopsies, one or more additional trocars are inserted. Inspection of the caudal side of the mesentery of the transverse colon and the region of Treitz ligament can be facilitated by bringing the patient into a Trendelenburg position.
Introduction of trocars (B):
The total number and position of trocars is dependent on the level of resection. The subxiphoidal trocar is only necessary for high resections of the stomach. Introduction of this trocar should be on the left side of the falciform ligament, especially when exploration of the cardia and gastroesophageal junction is necessary.
A
B
Laparoscopic Gastrectomy |
213 |
|
|
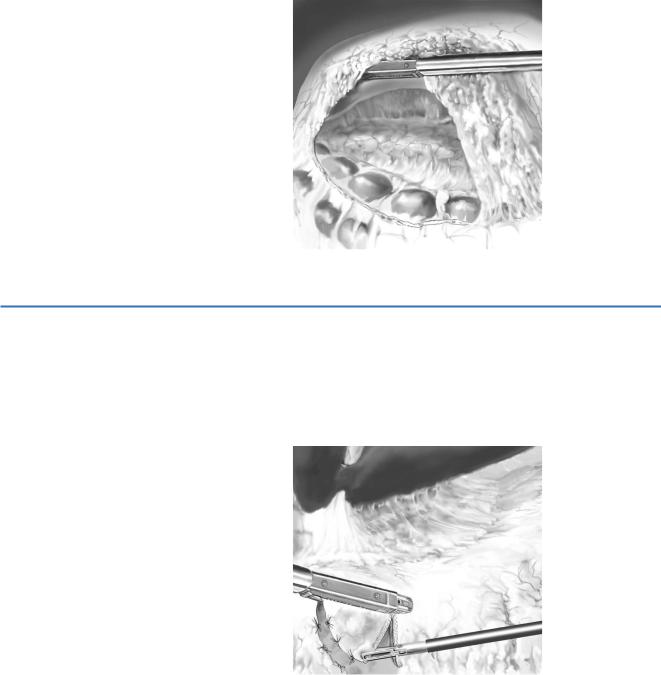
STEP 2 |
Opening of the lesser sac |
|
To determine (laparoscopic) resectability of the tumor, opening of the lesser sac is |
|
|
|
achieved by detaching the greater omentum from the transverse colon by sharp dissec- |
|
tion. In case of a benign indication, opening of the lesser sac can be performed more |
|
easily by creating a window in the greater omentum, for instance by using Ultracision. |
|
Involvement of the pancreas in malignant tumors requires conversion to open resection |
|
in most cases. In case of malignancy, once resectability has been established, the lesser |
|
sac is opened until the gastrocolic ligament is completely dissected from the hepatic to |
|
the splenic flexure. |
STEP 3 |
Resection of benign lesions |
|
In benign lesions, a stapled wedge resection is performed. Resection is performed |
|
|
|
under gastroscopic surveillance in case the lesion is not visible on the serosal side |
|
of the stomach. The gastrohepatic ligament must be opened if the tumor is located |
|
on the smaller curvature of the stomach. |
