
clavien_atlas_of_upper_gastrointestinal_and_hepato-pancreato-biliary_surgery2007-10-01_3540200045_springer
.pdf
Subtotal Gastrectomy, Antrectomy, Billroth II and Roux-en-Y Reconstruction and Local Excision in Complicated Gastric Ulcers |
163 |
|
|
Standard Postoperative Investigations
■The clinical course of the patient and the careful daily observation of the drains are the key points in postoperative care.
Postoperative Complications
■Anastomotic leaks and abscess formation
■Peritonitis
■Anastomotic strictures
■Delayed gastric emptying
■Recurrence of bleeding and ulcerations
■Pancreatitis
■Lesion to the pancreatic duct/papilla Vateri with biliary congestion
Tricks of the Senior Surgeon
■When mobilizing the minor curvature of the stomach, bear in mind that an atypical left hepatic artery may be present.
■Take care that the duodenal stump is closed without any tension on the wall. Mobilize the duodenum if required.
■The gastroduodenal artery should be carefully preserved to maintain adequate blood supply to the duodenum in case of Billroth II reconstruction.
■To avoid any biliary reflux, choose an adequate length of the jejunal loop (>40cm distal of the ligament of Treitz).
■To avoid any stricture of the anastomosis, choose a length of the gastrotomy for the anastomosis of 5–6cm in gastroenterostomy.
■In case of Roux-en-Y reconstruction, the blind end of the jejunal loop should be kept short to avoid the building of a reservoir within the blind end.
■In case of Billroth II procedure and artificial lesion to the spleen requiring splenectomy, take care that the remnant part of the stomach is adequately supplied with blood as the short gastric arteries arise from the splenic artery. In case of hypoperfusion, resection of the gastric remnant is necessary, and an esophagojejunostomy should be done.
Total Gastrectomy
with Conventional Lymphadenectomy
Jürg Metzger
Introduction
In 1884 Connor attempted the first total gastrectomy in humans, reestablishing continuity with an esophagoduodenostomy. His patient did not survive the operation. In 1897 Schlatter carried out the first successful total gastrectomy. In 1892, Roux described a new procedure where the jejunal loop was divided and the distal limb was joined to the esophagus. The proximal limb of the loop was anastomosed to the jejunum some 45cm distal to the esophagus. A large number of gastric substitutes have been tried over the past century grouped into large and small bowel procedures. Some operations preserve the continuity through the duodenum. Others bypass the duodenal passage. Some procedures include a pouch construction and/or an antireflux modification. Currently, Roux-en-Y reconstruction is still the most widely used procedure after a total gastrectomy.
Indications and Contraindications
Indications |
■ |
Adenocarcinomas arising in corpus or fundus of the stomach |
|
■ |
Malignant tumors arising in the antrum of the stomach and showing a poor |
|
|
pathohistological diagnosis (low grade tumors, diffuse type, signet-ring) |
|
■ |
Zollinger-Ellison syndrome |
|
■ |
Mesenchymal tumors (e.g., gastrointestinal stromal tumors, GISTs) |
|
■ |
Palliative gastrectomy for severe bleeding |
|
|
Peritoneal carcinosis |
Contraindications |
■ |
|
|
■ |
Penetration into neighboring organs |
|
■ |
Child-Pugh C cirrhosis with severe portal hypertension |
Preoperative Investigation and Preparation for the Procedure
History: |
Cardiac disease, pulmonary disease, gastric outlet function, melena, |
|
alcohol, smoking, Helicobacter pylori infection, diet, geographic |
|
risk, genetic factors |
Clinical evaluation: |
Nutritional status |
Laboratory tests: |
Hb, coagulation parameters, tumor markers, albumin |
Gastroscopy: |
To prove the diagnosis (biopsies), endoscopic ultrasound |
CT scan: |
Assessment of resectability, distant mestastases |
Preparation: |
Consider bowel preparation with preoperative signs of involvement |
|
of large bowel |

166 |
SECTION 2 |
Esophagus, Stomach and Duodenum |
|
|
|
|
|
|
Procedure |
|
|
|
Access |
|
|
|
Midline incision or bisubcostal incision, division of round and falciform ligament |
||
|
|
||
STEP 1 |
Exposure and exploration of the abdomen with focus on |
||
|
■ |
Liver metastases |
|
|
|
||
|
■ |
Peritoneal carcinosis |
|
|
■ |
Tumor localization and size |
|
|
■ |
Lymph node enlargement |
|
|
■ |
Penetration into pancreas, spleen, and transverse colon |
|
Total Gastrectomy with Conventional Lymphadenectomy |
167 |
|
|
|
|
STEP 2 |
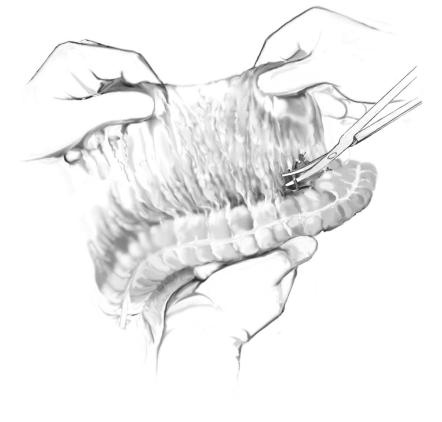
Separation of the greater omentum from the entire transverse colon |
|
|
|
|
The entire gastrocolic omentum is separated from the transverse colon by scissors dissection through the avascular embryonic fusion plane. It is tremendously helpful to be alert of the difference in texture and color of the fat in the epiploic appendices of the colon and that of the omentum. Bleeding will be avoided by keeping this important plane of dissection between these two different structures. The next step is to elevate the mobilized omentum from the transverse colon and to expose the anterior surface of the pancreas. As the omentum is mobilized, the venous branch between the right gastroepiploic and middle colic veins is identified and ligated.

168 |
SECTION 2 |
Esophagus, Stomach and Duodenum |
|
|
|
STEP 3 |
View of the mobilized left liver lobe and the esophagogastric junction |
|
|
|
|
Next mobilize the left lobe of the liver unless segments II and III can easily be retracted. The lesser omentum is divided. If present, a replaced left hepatic artery will be identified at this time and should be preserved. An additional liver retractor is used so that the abdominal part of the esophagus is visible. The stomach is then pulled in an inferior direction and the peritoneum and membrana phrenico-esophagea are incised over the esophagogastric junction. Both crura of the diaphragm are identified and cleared. Using a large dissector, the esophagus is separated from the crura and is then encircled by a finger. A rubber band is placed around the esophagus and retained by a clamp. The vagal nerves are divided, which facilitates further mobilization of the distal esophagus.
Total Gastrectomy with Conventional Lymphadenectomy |
169 |
|
|
|
|
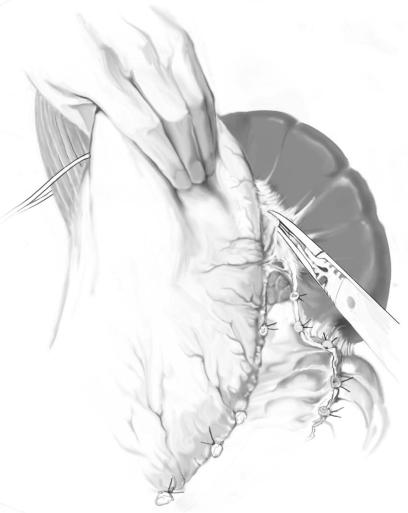
STEP 4 |
Mobilization of the greater curvature |
|
|
|
|
The greater omentum is released from the splenic flexure. The stomach is then gently pulled in an inferior and medial direction and the short gastric vessels are dissected at the point of contact with the greater curvature of the stomach.
170 |
SECTION 2 |
Esophagus, Stomach and Duodenum |
|
|
|
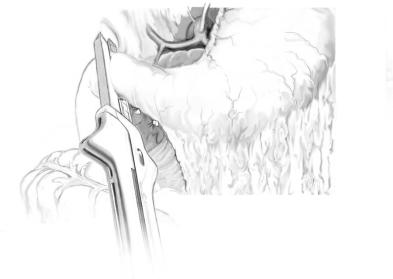
STEP 5 |
Transection of the duodenum |
|
|
|
|
The right gastroepiploic and the right gastric arteries are divided, and the posterior wall of the duodenum is freed. Extensive duodenal dissection is not necessary when the distal antrum is free of tumor. The duodenum is then transected with a linear stapler 1–2cm below the pylorus. The stapler line is oversewn with a non-dissolvable running suture. The distal end of the specimen is covered with a gauze, which should be fixed in place with an additional umbilical tape ligature.

Total Gastrectomy with Conventional Lymphadenectomy |
171 |
|
|
|
|
STEP 6 |
D2 lymphadenectomy |
|
|
|
|
The stomach is now held upwards and to the left, which allows optimal exposure. A D2compartment lymphadenectomy is carried out. This involves removing all the nodes along the common hepatic artery, nodes behind and within the hepatoduodenal ligament, and nodes along and around the celiac artery, the trunk of the splenic artery and the cranial margin and surface of the pancreas. All the arteries are fully freed of areolar and lymphatic tissue and secured with vessel loops. It is important to clip or ligate all the remaining lymphatic vessels to avoid postoperative lymphorrhea.
172 |
SECTION 2 |
Esophagus, Stomach and Duodenum |
|
|
|
STEP 7 |
Division of left gastric vessels |
|
|
|
|
The left gastric vessels are identified and isolated from adjacent tissues by blunt and sharp dissection and are then ligated and divided. The coronary vein, which is situated just caudal to the artery, is often identified first in the course of dissection.

Total Gastrectomy with Conventional Lymphadenectomy |
173 |
|
|
|
|
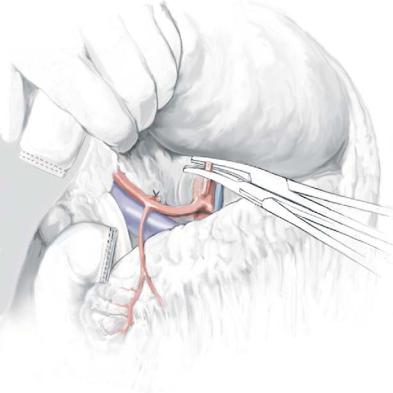
STEP 8 |
Transection of the distal esophagus |
|
|
|
|
After mobilization of the entire stomach, the esophagus is then divided just above the cardia. A right-angled clamp is placed distal to the lower esophagus and the esophagus is divided by electrocautery. The specimen, which consists of stomach, proximal 2cm of duodenum, greater omentum and regional lymph nodes, is sent to pathology to confirm the adequacy of the resected margins before reconstruction.
