
clavien_atlas_of_upper_gastrointestinal_and_hepato-pancreato-biliary_surgery2007-10-01_3540200045_springer
.pdf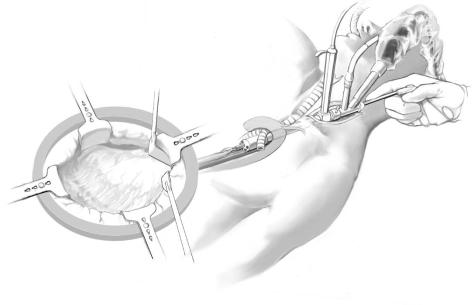
Minimally Invasive Esophagectomies |
111 |
|
|
|
|
STEP 2 |
Endodissection |
|
|
|
The mediastinal endodissector is then assembled and inserted into the upper medi- |
|
|
|
|
|
astinum. This instrument features a tissue dilator at the tip, a 15-degree Hopkins fiber- |
|
|
optic device and a working channel for one 5-mm laparoscopic instrument. The tissue |
|
|
dilator is anatomically designed so that it can “ride” on the esophageal surface and opens |
|
|
an anterograde dissection space of 2–3cm in the mediastinum. The tissue dilator of the |
|
|
mediastinoscope can be freely rotated 360degrees. For full operation, the medi- |
|
|
astinoscope is connected to a video camera, a xenon light source, and a flushing/suction |
|
|
device. |
|
|
It is normal that the first steps of endoscopic dissection of the retrotracheal space are |
|
|
difficult due to the limited initial vision and the anatomical narrowing of the thoracic |
|
|
inlet. Microinstruments such as scissors, forceps or a coagulation/suction instrument |
|
|
as well as ultrasonic shears can be used through the working channel of the medi- |
|
|
astinoscope. |
112 |
SECTION 2 |
Esophagus, Stomach and Duodenum |
|
|
|
STEP 3 |
Endodissection: mediastinoscopic anterior view |
|
|
|
|
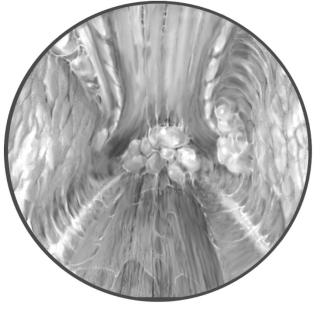
The retrotracheal tissues are divided by pushing the tissue with the coagulation/suction device followed by the application of a short “coagulation” impulse or dissection with ultrasonic shears.
The anterior surface of the esophagus is subsequently dissected until 2–3cm below the tracheal bifurcation.
We usually identify the left recurrent nerve, both vagal trunks, the tracheal bifurcation and the subcarinal lymph nodes, which can be removed in toto.
By turning the tip of the instrument counterclockwise by 90degrees, the left surface of the esophagus can be dissected. This is usually the most difficult part of endodissection due to adhesions between esophagus and the left main bronchus. These must be totally divided. Care has to be taken not to divide the longitudinal muscle layer of the esophagus at this point.
Minimally Invasive Esophagectomies |
113 |
|
|
|
|
STEP 4 |
Endodissection: mediastinoscopic posterior view |
|
|
|
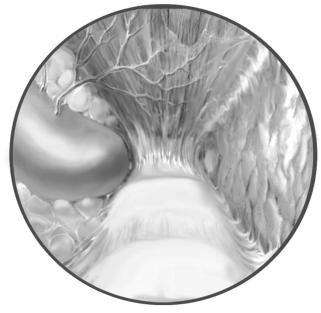
The back wall and the right surface of the esophagus usually present no major |
|
|
|
|
|
difficulties, and opening of the mediastinal pleura is not usually critical. Finally, |
|
|
the esophagus should be circumferentially mobilized and contact between the ab- |
|
|
dominal team and the cervical team should be made. The cervical team assists during |
|
|
the phase of en bloc dissection of the infracarinal esophagus by providing light and |
|
|
suction from above. This can be helpful especially in large tumors. Finally, the cervical |
|
|
esophagus is divided by a longitudinal stapler device and retracted into the abdominal |
|
|
cavity. The mediastinal procedure is completed by control of hemorrhage and removal |
|
|
of visible lymph nodes for supplementary staging information. |
114 |
SECTION 2 |
Esophagus, Stomach and Duodenum |
|
|
|
STEP 5 |
Radical transhiatal esophagectomy with endodissection; |
|
|
dissection of the hiatus and the inferior mediastinum |
|
|
|
|
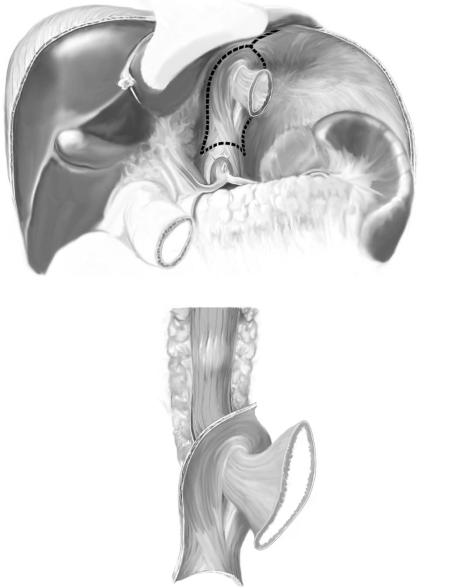
After abdominal incision (inverse-T laparotomy and self-holding Stuhler’s retractors), the hiatus of the patient should be exposed after mobilization of the left lobe of the liver. When endodissection is nearly completed, the abdominal team widely opens the
hiatus by excising portions of the crura of the diaphragm (left adherent to the specimen) and dividing the diaphragmatic vein between clamps. The periesophageal mediastinal lymphatic tissue is dissected from the pericardium and remains adherent to the specimen in “en bloc” fashion. The primary tumor should not be exposed during the operation. Both visceral layers of the pleura may be resected without problems. After complete mobilization of the esophagus by the cervical team and division of the cervical esophagus with a linear stapler, the specimen is retracted into the abdominal cavity. A lymphadenectomy in compartments I and II is always added (A-1, A-2).
A-1
A-2
Minimally Invasive Esophagectomies |
115 |
|
|
|
|
STEP 6 |
Reconstruction |
|
|
|
Routinely, we reconstruct the gastrointestinal passage by pull-through of a narrow |
|
|
|
|
|
gastric tube in the anterior or the posterior mediastinum. Only in younger patients |
|
|
with good prognosis is a reconstruction with colon accomplished. |
|
|
See chapter on “Subtotal Esophagectomy: Transhiatal Approach” for standard |
|
|
postoperative investigations. |
Postoperative Complications
■Recurrent nerve palsy
■Chylothorax
■Bleeding
■Anastomotic insufficiency
Tricks of the Senior Surgeon
Thoracoscopic Esophagectomy
■Should only be performed with excellent single lung ventilation.
■Convert early in case of bleeding or loss of orientation.
■Suture the thoracic duct with non-resorbable suture material.
Radical Transhiatal Esophagectomy with Endodissection
■Perform endodissection and abdominal approach simultaneously to save time.
■Endodissection: always keep the esophagus in sight to avoid damage to vital mediastinal structures.
■Endodissection: in case of mediastinal arterial bleeding it is better to compress/tamponate than coagulate.
■Do not attempt to dissect the tumor below the tracheal bifurcation. This is better done by the abdominal team through the open hiatus.

Zenker’s Diverticula: Open Approach
Claus F. Eisenberger, Christoph Busch
Introduction
|
The common type of diverticula (Zenker’s) is not actually of esophageal origin, |
||
|
but arises from the relatively bare triangle of mucosa located between the inferior |
||
|
pharyngeal constrictors and the cricopharyngeal muscle (Killian’s triangle). |
||
|
Zenker’s diverticula are 10 times more common than other esophageal diverticula. |
||
|
|
Zenker’s diverticula are so called false diverticula and are classified according |
|
|
to Lahey: |
|
|
|
Stage I: |
No symptoms, local mild inflammation |
|
|
Stage II: |
Dysphagia and regurgitation |
|
|
Stage III: |
Esophageal obstruction, dysphagia, and regurgitation |
|
|
Indications and Contraindications |
||
|
|
Progress over time. Treatment is recommended for patients who have moderate |
|
Indications |
■ |
||
|
|
to severe symptoms/complications (pneumonia or aspiration) |
|
|
|
Severe physical constitution |
|
Contraindication |
■ |
||
Preoperative Investigations/Preparation for the Procedure
■Clinical examination
■Contrast swallow (water-soluble)
■Upper gastrointestinal endoscopy
■Ultrasound
■Manometry
■A large gastric tube is carefully placed in the upper esophagus
118 |
SECTION 2 |
Esophagus, Stomach and Duodenum |
|
|
|
|
Procedure |
|
|
Access |
|
|
The patient is placed in a supine position with the head rotated to the right. |
|
|
|
|
STEP 1 |
Approach |
|
|
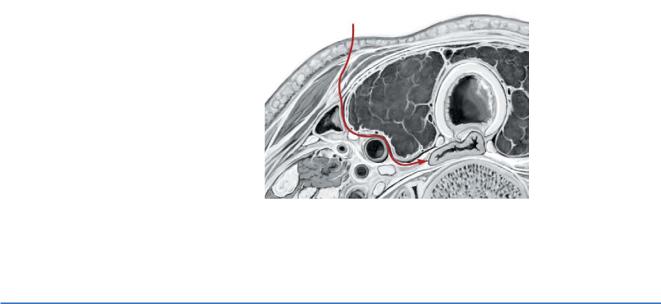
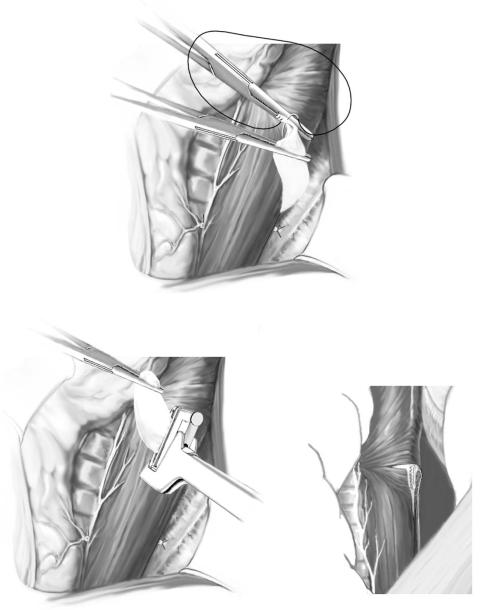
The approach to the diverticulum for surgical therapy comes through a left cervical inci- |
|
|
||
|
sion (most Zenker’s diverticula present on this side) at the level of the cricoid cartilage |
|
|
on the anterior aspect of the sternocleidomastoid muscle just above the clavicle. The |
|
|
anatomical overview of the access to the cervical esophagus is given in the figure. |
|
STEP 2 |
Dissection |
|
Dissection is performed between the medial aspect of the sternocleidomastoid muscle, |
|
|
|
which is pulled laterally, and the strap muscles by retracting the carotid sheath laterally |
|
and preserving the recurrent laryngeal nerve. The omohyoid muscle may be either |
|
retracted or transected. The thyroid gland is mobilized and vessels are dissected. |
Zenker’s Diverticula: Open Approach |
119 |
|
|
|
|
STEP 3 |
Mobilization of the esophagus and the diverticulum |
|
|
|
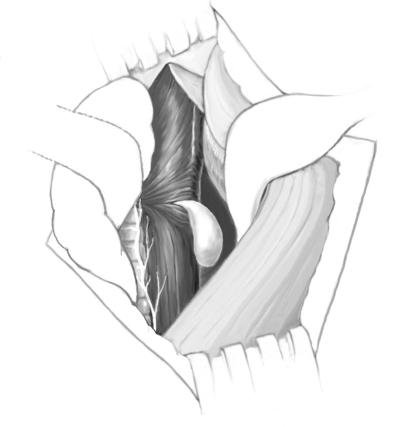
The esophagus is mobilized from the prevertebral fascia, and the diverticulum is |
|
|
|
|
|
evident posterior to the esophagus (a tube may be inserted in the diverticulum for |
|
|
better identification). Large diverticula may extend into the mediastinum, but gentle |
|
|
traction and blunt dissection are sufficient to mobilize even the largest diverticula. |
|
|
The figure shows the anatomy of the cervical diverticula. |
120 |
SECTION 2 |
Esophagus, Stomach and Duodenum |
|
|
|
STEP 4 |
Preparation of diverticulum |
|
|
|
|
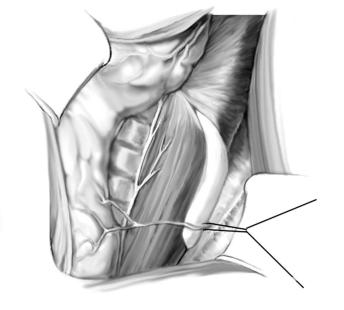
The neck of the diverticulum is dissected. Gentle traction on the diverticulum exposes the fibers of the cricopharyngeus muscle. Oral insufflation of air may help to find the diverticulum. In the figure the anatomical aspects are shown (the vessels are retracted to the left).
Zenker’s Diverticula: Open Approach |
121 |
|
|
|
|
STEP 5 |
Myotomy |
|
|
|
The cricopharyngeus muscles are divided and bluntly dissected from the mucosa. |
|
|
|
|
|
Myotomy of the pars transversa and of the upper esophagus is performed. |
|
|
After myotomy several options exist, depending on the size of the diverticulum. |
|
|
Small diverticula measuring up to 2cm virtually disappear after the myotomy is |
|
|
completed and may be left alone or fixed cranially with the apex. They may be inverted |
|
|
and sutured to the prevertebral fascia, which prevents food retention without necessi- |
|
|
tating creation of a staple line or suture line that is at risk for fistula formation (A). |
|
|
Larger diverticula are resected with a linear stapler parallel to the esophageal lumen, |
|
|
taking care not to compromise the diameter of the esophagus (B-1, B-2). Alternatively, |
|
|
open resection and closure with a running suture is performed. |
A
B-2
B-1
