
Practical Plastic Surgery
.pdf
362 |
Practical Plastic Surgery |
problem. The recommended management of a bifid uvula is close observation to ensure that speech develops normally.
Sequence of the Procedures
Multiple protocols for the management of CL/P have been suggested over the years by various authors. Today, the mainstream of cleft repair calls for closure of the lip at an early age (from age 6 weeks to 6 months) followed by closure of the palate approximately 6 months later. This protocol has little impact on facial development. When managing a residual alveolar defect and an associated oronasal fistula, the primary goal of surgery is to allow subsequent development of a normal alveolus. Optimal eruption of teeth at the cleft site and development of normal periodontal structures of the teeth adjacent to the cleft occur when bone grafting and final fistula closure are performed prior to eruption of the permanent canine teeth at the cleft site.
Choice of Repair
The list of surgical techniques used in palatal cleft closure is extensive. The repairs differ depending upon whether the cleft is an isolated cleft palate or part of a unilateral or bilateral cleft lip and palate. The three main categories include: (1) simple palatal closure; (2) palatal closure with palatal lengthening; and (3) either of the first two techniques with direct palatal muscle reapproximation.
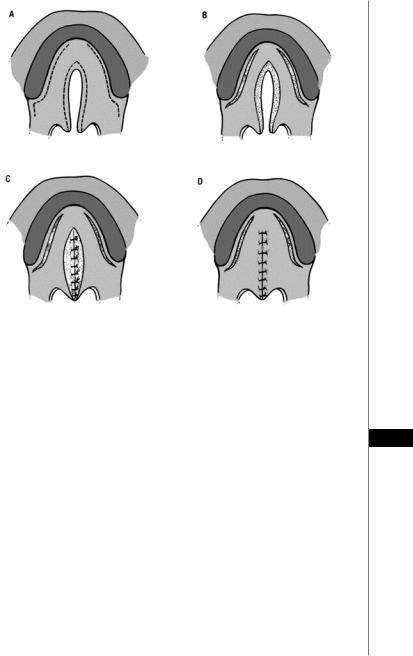
The Von Langenbeck Procedure
The simple palatal closure was introduced by von Langenbeck and is the oldest cleft palate operation in wide use today (Fig. 59.2). The bipedicle mucoperiosteal flaps are created by incising along the oral side of the cleft edges and along the posterior alveolar ridge from the maxillary tuberosities to the anterior level of the cleft. The flaps are then mobilized medially with preservation of the greater palatine arteries and closed in layers. The hamulus may need to be fractured to ease the closure. The von Langenbeck repair continues to be popular because of the simplicity of the operation. This technique can successfully close moderate-sized defects. Modern critics of the von Langenbeck technique cite the unnecessary anterior fistulas it promotes, the insufficiently long palate it produces and the poor speech result associated with it.
Trier and Dreyer combined primary von Langenbeck palatoplasty with levator
59sling reconstruction (intravelar veloplasty). The author has observed better speech and superior velopharyngeal function following intravelar veloplasty with muscle reconstruction and recommended careful reconstruction of the levator sling at the time of palate repair.
Palatal Lengthening or V-Y Pushback
Veau’s protocol for closure of cleft palate stressed the need for (1) closure of the nasal layer separately, (2) fracture of the hamular process, (3) staged palatal repair following primary lip and vomer flap closure, and (4) creation of palatal flaps based on a vascular pedicle. Kilner and Wardill devised a technique of palatal repair in 1937 that was more radical than Veau’s and that ultimately became the V-Y pushback. It includes lateral relaxing incisions, bilateral flaps based on greater palatine vessels, closure of the nasal mucosa in a separate layer, fracture of the hamulus, separate muscle closure and V-Y palatal lengthening.
The 4-flap technique is similar to the Wardill-Kilner 2-flap technique, except the oblique incisions are more posterior to create four unipedicle flaps. The flaps are again mobilized medially and closed. These pushback techniques achieve greater
Cleft Palate |
363 |
|||
|
|
|
|
|
|
|
|
|
|
Figure 59.2. The von Langenbeck repair. Two bipedicle mucoperiosteal flaps are created by incising along the oral side of the cleft edges and along the posterior alveolar ridge from the maxillary tuberosities to the anterior level of the cleft. The flaps are then mobilized medially with preservation of the greater palatine arteries and closed in layers. The hamulus may need to be fractured to ease the closure. (Reprinted from emedicine.com with permission.)
immediate palatal length but at the cost of creating a larger area of denuded palatal
bone anterolaterally. The gain in the length of the palate has not been demonstrated 59 to be permanent nor has it translated to improved velopharyngeal function. This approach has been associated with a higher incidence of fistula formation.
Intravelar Veloplasty
Several studies have emphasized the necessity of realignment of the muscle in the soft palate. The approach was designed to lengthen the palate as well as to restore the muscular sling of the levator veli palatini. Improved velopharyngeal function was sporadically reported. Marsh et al conducted a prospective study of the effectiveness of primary intravelar veloplasty and found no significant improvement in velopharyngeal function.
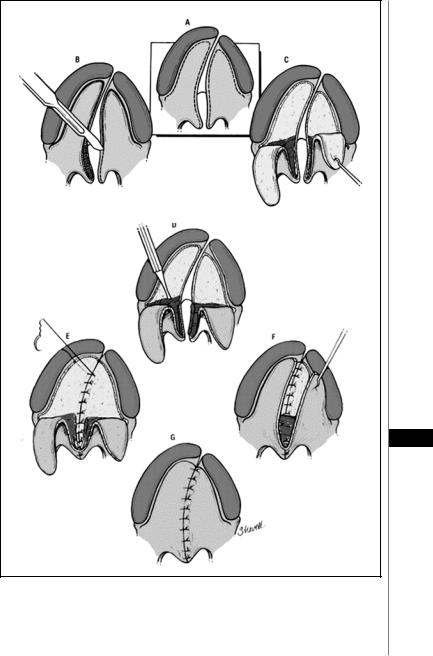
Double-Opposing Z-Plasties
In 1986, Furlow described a single-stage palatal closure technique consisting of double opposing Z-plasties from the oral and nasal surfaces (Fig. 59.3). Use of the double Z-plasty minimized the need for lateral relaxing incisions to accomplish closure. The palate was also lengthened as a consequence of the new position of the

364 |
Practical Plastic Surgery |
|
|
|
|
|
|
|
Figure 59.3. Double-opposing Z-plasties. Furlow’s single-stage palatal closure technique consisting of double opposing Z-plasties from the oral and nasal surfaces. The double Z-plasty minimizes the need for lateral relaxing incisions to accomplish closure. The palate is lengthened as a consequence of the new position of the velar and pharyngeal tissues. (Reprinted from emedicine.com with permission.)
velar and pharyngeal tissues. Preliminary data revealed that speech development was excellent, with 86% exhibiting normal speech in Furlow’s study.
Others have confirmed the improvement in speech development. The closure of the hard palate in Furlow’s technique avoids the use of lateral relaxing incisions. The mucoperiosteal flaps are mobilized from the bony hard palate and the palatal defect closed by tenting the flaps across and creating a moderate empty space between the flaps and the bony hard palatal vault. Furlow’s technique appears to be quite successful in clefts of limited size. In moderate-size clefts, lateral relaxing incisions may still be required to obtain closure.
Two-Flap Palatoplasty
Bardach (1984) and Salyer independently modified the 2-flap palatoplasty to combine elements of other operations with some innovative details (Fig. 59.4). The main goals are complete closure of the entire cleft without tension at an early age (<2 mo) with minimal exposure of raw bony surfaces and the creation of a functioning soft palate. The authors believe that a muscle sling within the soft palate, not velar lengthening, is essential to adequate speech. Morris and colleagues note that 80% of patients
59treated with this method developed velopharyngeal function within normal limits, although 51% required speech therapy before normal speech production was achieved.
Velar Closure—Delayed Hard Palate Closure
Schweckendiek (1978) closed the soft palate early (at age 6-8 mo) but left the hard palate open, albeit occluded with a prosthetic plate, until the age of 12-15 years. In unilateral clefts the soft palate is closed first, followed by lip surgery 3 weeks later. In bilateral clefts one side of the lip is closed first in conjunction with primary veloplasty, with repair of the other side of the lip and the alveolar cleft 3 weeks later. Schweckendiek reported normal jaw development subsequent to this protocol. Many European surgeons now use Perko’s (1991) approach of two-stage palatal closure. Repair of the soft palate occurs at age 18 months and of the hard palate at 5-8 years. Perko found that the remaining cleft in the hard palate does not disturb speech development to a significant degree. Several long-term assessments of patients who undergo the Schweckendiek approach or the Perko (Zurich) approach disclosed an unusually high incidence of short palate and poor mobility of the soft palate, with a correspondingly high degree of velopharyngeal insufficiency (VPI). Conversely, facial growth was judged to be quite acceptable in most patients.
Cleft Palate |
365 |
|
|
|
|
A
B
59
Figure 59.4. Two-flap palatoplasty. A) After lateral relaxing incisions are performed, bilateral flaps are elevated based on greater palatine vessels. B) Closure of the nasal mucosa is performed. The hamulus may be fractured, the muscle is repaired, and the oral mucosa is closed as a separate layer. (Reprinted from emedicine.com with permission.)

366 |
Practical Plastic Surgery |
Postoperative Management
Despite the difference in surgical technique, a general postoperative routine exists. After surgical repair, the child is given nothing by mouth until the next day. Hydration is maintained during this time with intravenous fluid. Oximetry is continuously monitored for 24-48 hours. Arm splints are also applied to prevent the child from disrupting the wound by placing his fingers in his mouth. Oral feeding is initiated by syringes or drinking from cups. Nipple feeding is avoided. Patients can usually be discharged the day after the operation with extension arm splints. The liquid diet is continued for 7-10 days with solid food to follow.
Early Complications
The complications of greatest concern in the immediate postoperative period are bleeding and respiratory distress, yet the true incidence of these complications is difficult to determine from a review of the literature. Reports of surgical experiences with CL/P typically mix children and adults, type of cleft, repair technique, timing of the surgery, or sequence of operations.
Some reports suggest that the Wardill-Kilner repair results in greater morbidity than other methods. This technique typically involves increased postoperative bleeding following division of the anterior branch of the greater palatine artery. Epinephrine is routinely injected prior to the incision to allow better visibility and easier control of bleeding. Hemostatic agents can also be used to pack denuded areas of the palate to minimize the amount of bleeding.
Respiratory compromise secondary to obstruction from the palate lengthening or sedation can be life threatening. Airway obstruction was considerably more common after a von Langenbeck procedure with pharyngeal flap.
Other complications, such as wound dehiscence and oronasal fistula, can be difficult to manage. Dehiscence of the palatal closure, as with wound closure in other parts of the body, is usually a result of poor tissue quality and excessive wound tension. The incidence of dehiscence is low, but the incidence of oronasal fistula has been reported at 5-29%.
Long-Term Complications
59 Palatal Fistula
Fistula treatment after cleft palate repair is a difficult problem. Fistulas are classified as prealveolar, alveolar and postalveolar. A fistula of sufficient size can lead to significant problems, ranging from food passing into the nasal chamber to speech difficulties secondary to nasal air emission. Factors that may contribute to fistula formation are type of cleft, type of repair, wound tension, single-layer repair, dead space below the mucoperiosteal flap and maxillary arch expansion. The usual management strategy is to avoid closure of a fistula until arch expansion can be completed.
The management of a fistula secondary to cleft palate repair is limited in success, with a high incidence of recurrence after initial fistula closure. The most frequent technique used in palatal fistula closure is local flap mobilization. Bone and periosteal grafts have been reported to improve the results. Tongue flaps and microvascular tissue transfers are used for difficult palatal fistulas and large palatal defects, respectively.
Velopharyngeal Incompetence
Morris, in his review of the literature, reported an incidence of velopharyngeal competence of 75%, as defined by the absence of consistent evidence of VPI. No

Cleft Palate |
367 |
|
|
|
|
differentiation was made on the type of cleft or the technique of repair. Peterson-Falzone (1991) reported 83.4% competence based on the same criteria. However, when using the criterion of no nasal emission or hypernasality, the incidence of velopharyngeal competence decreases to 60%. The analysis of velopharyngeal competence after various techniques is difficult to interpret in the different studies. The anatomy of the cleft has a great degree of variability that is usually not controlled.
Growth and Morphology |
|
The severity and laterality of the clefts, as well as the choice of cephalometric mea- |
|
surements used in the assessment, account for much of the variability in the reported |
|
effects of clefting on facial growth. Grayson et al studied the net effect of palatal clefts |
|
on the facial skeleton as viewed by lateral cephalograms and determined by mean |
|
tensor analysis. The authors note reduced facial bone growth in all directions but |
|
principally in the horizontal dimension. The effect was most pronounced at the level |
|
of the palate and slightly less so in height of the mid face. Vertical facial growth was |
|
most restricted in subjects who had clefts of both the primary and secondary palate |
|
compared with those who had clefts of the secondary palate alone. |
|
Pearls and Pitfalls |
|
The management of a patient with cleft palate is complex. No current universal |
|
agreement exists on the appropriate treatment strategy. Several main points should be |
|
emphasized. Normal speech should be the most important consideration in the thera- |
|
peutic plan. Growth disturbance should be minimized but not at the expense of speech |
|
impairment because facial distortion can be satisfactorily managed with future sur- |
|
gery, whereas speech impairment is often irreversible. Repair of cleft palate with the |
|
goal of establishing a competent velopharyngeal sphincter should be completed at age |
|
6-12 months. At the present time, there are widely divergent claims of superior results |
|
from various techniques. There remains a need for well-controlled, prospective studies |
|
to determine the optimal technique of cleft palate repair. Until then, cleft patients |
|
should be managed in a center with an experienced, multidisciplinary team |
|
Suggested Reading |
|
1. Bardach J, Morris HL, Olin WH. Late results of primary veloplasty: The marburg |
59 |
project. Plast Reconstr Surg 1984; 73(2):207-18. |
2.Dufresne CR. Oronasal and nasolabial fistulas. In: Bardach J, Morris HL, eds. Multidisciplinary Management of Cleft Lip and Palate. 1st ed. WB Saunders Co, 1991:425-436.
3.Furlow Jr LT. Cleft palate repair by double opposing Z-plasty. Plast Reconstr Surg 1986; 78(6):724-38.
4.Hodges PL, Pownell PH. Cleft palate surgery and velopharyngeal function. Plast Surg 1994; 7(23):1-36.
5.Kaufman FL. Managing the cleft lip and palate patient. Pediatr Clin North Am 1991; 38(5):1127-47.
6.Lindsay WK. Surgical repair of cleft palate. Clin Plast Surg 1975; 2(2):309-18.
7.Nguyen PN, Sullivan PK. Issues and controversies in the management of cleft palate. Clin Plast Surg 1993; 20(4):671-82.
8.Perko M. Two-stage palatoplasty. In: Bardach J, Morris HL, eds. Multidisciplinary Management of Cleft Lip and Palate. 1st ed. WB Saunders Co, 1991:311-320.
9.Rohrich RJ, Byrd HS. Optimal timing of cleft palate closure. Speech, facial growth, and hearing considerations. Clin Plast Surg 1990; 17(1):27-36.
10.Schweckendiek W, Doz P. Primary veloplasty: Long-term results without maxillary deformity. A twenty-five year report. Cleft Palate J 1978; 15(3):268-74.
Chapter 60
Rhytidectomy
Stephen M. Warren and James W. May, Jr.
Introduction
Aesthetic facial surgery is intended to rejuvenate the cervicofacial contour. Recognizing the elements of an aging face and neck are a prerequisite to planning any procedure. Common stigmata of facial aging include: ptotic malar pads, heavy nasolabial folds, nasojugal creases, marionette lines, jowls, geniomandibular grooving, cheek and neck skin laxity, platysmal banding, lateral orbital wrinkling, submental lipodystrophy and salivary gland ptosis. While all of these structures may be affected by the pull of gravity, repetitive contraction of the underlying muscle, and cellular/subcellular aging, each can be improved by facelifting techniques. Other problems such as forehead and glabellar lines, eyelid bulges and excess skin, fine facial wrinkles, lip atrophy, cheek fat atrophy, senile nasal dysmorphia cannot be corrected with a facelift. Since it is not possible to design a universal technique for all patients, facelifting must be preceded by a sound knowledge of the anatomy and a thorough understanding of the elements to be corrected. Careful planning and good technique are necessary to precisely remove redundant skin, resuspend or resect fat and repairing lax musculature and fascia.
Anatomy
There are five important anatomic levels in the face and neck: skin, subcutaneous fat, the superficial musculoaponeurotic system (SMAS)/muscle layer, fascia and the facial nerve. While these layers are consistent throughout the face and neck, in some area such as over the zygomatic arch, the layers are highly compressed. In addition to these tissue planes, the surgeon must be familiar with the folds, retaining ligaments, glands , blood supply and fat pads of the face.
Skin
As we age, the skin changes in its appearance and characteristics. Skin aging is accelerated by sunlight; this process is known as dermatohelisosis, solar elastosis, or photoageing. Photoageing is accelerated by long and short wavelength ultraviolet radiation (UVA and UVB) injury to the epidermis and dermis. Studies suggest that UV light can activate enzymes that degrade collagen and elastin in skin. Repetitive solar damage can cause fine lines and wrinkles, telangiectasias, solar comedones, dryness and actinic lentigines (diffuse or mottled brown patches). Signs of skin aging are accelerated by smoking. Facelifting cannot directly improve the quality of photoaged skin, but it can improve the appearance.
Subcutaneous Tissues
The subcutaneous plane provides a relatively safe plane for dissection. This layer contains innumerous fine ligaments passing from the subjacent SMAS/muscle layer to the overlying dermis of the skin. These ligaments transmit mimetic movements into facial expressions but also contribute to facial lines and wrinkles.
Practical Plastic Surgery, edited by Zol B. Kryger and Mark Sisco. ©2007 Landes Bioscience.

Rhytidectomy |
369 |
SMAS/Muscle Layer
Below the skin and subcutaneous tissues, is the SMAS/muscle layer. The SMAS/ muscle layer is a continuum from neck to scalp. It is composed of fibrous, muscular, or fatty tissues. In the neck, the platysma represents the most inferior portion of the SMAS/muscle layer. In the face, the SMAS is a tough fibrofatty layer over the parotid. Medial to the parotid, the muscles of facial expression (e.g., zygomaticus major/minor and orbicularis oculi) are contiguous with the SMAS layer. Above the zygoma, the SMAS is contiguous with the frontalis muscle and the superficial temporal fascia (or temporoparietal fascia). The temporoparietal fascia blends into the galea as it reaches the scalp. Collectively, this layer may be thought of as the platysma-SMAS-temporoparietal-galea layer.
Fascial Layer
Between the SMAS/muscle layer and the facial nerve is a fascial layer. In the neck, the layer is termed the cervical fascia. Over the parotid, it exists as a filmy, areolar layer called the parotideomasseteric fascia. This thin, nearly transparent layer lies immediately superficial to the facial nerve. The fascia continues cephalad passing over the zygoma. In the upper third of the face, the layer becomes the innominate fascia that blends into the subgaleal fascia over the scalp. The innominate fascia lies between the SMAS/muscle extension (i.e., temporoparietal fascia) and the superficial layer of the deep temporal fascia. The anatomy here is critical because the frontal branch of the facial nerve (see below) pierces the innominate fascia at the level of the zygomatic arch and travels along the undersurface of the temporoparietal fascia. Collectively, this fascia may be thought of as the cervical-parotideomasseteric-innominate-subgaleal layer.
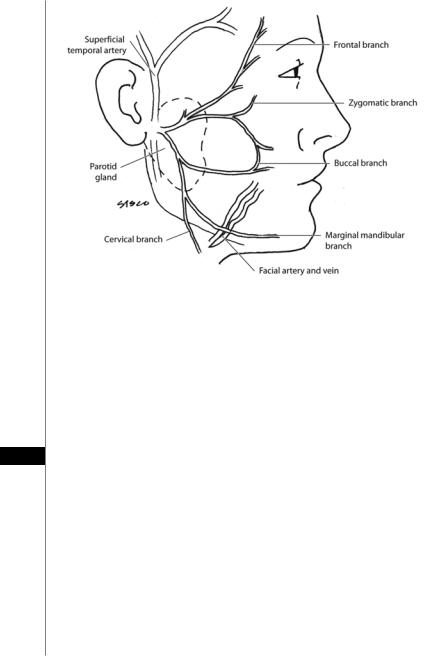
Facial Nerve
The main facial nerve trunk emerges from the stylomastoid foramen to provide motor innervation to 20 paired muscles of facial expression as well as the posterior belly of the digastric, stylohyoid and stapedius muscles. In addition, the facial nerve provides sensory innervation to the anterior two-thirds of the tongue, external auditory meatus (nerve of Jacobsen), soft palate and pharynx. The motor portion of the facial nerve divides into five major branches (Fig. 60.1). The branches of the facial nerve travel just deep to the cervical-parotideomasseteric fascia to innervate all muscles
of facial expression from their deep surface with three exceptions: (1) mentalis, (2) 60 buccinator, and (3) levator anguli oris. These muscles lie deep to the facial nerve branches and are, therefore, innervated on their superficial surfaces.
The frontal branch of the facial nerve leaves the parotid gland immediately beneath to the zygomatic arch. As it crosses the superficial surface of the zygomatic arch, the frontal branch pierces the innominate fascia to travel along the undersurface of the temporoparietal fascia (superficial temporal fascia). At this point, the frontal branch is extremely susceptible to inadvertent injury. The path of the frontal branch can be approximated by connecting a line 2 cm lateral to the edge of the eyebrow to the lower edge of the earlobe, termed Pitanguy’s line. The frontal branch innervates the muscles of the upper part of the face including the upper orbicularis oculi, frontalis and corrugator muscles. Transection of the frontal branch leads to brow ptosis.
The zygomatic branch provides motor fibers to the lower orbicularis oculi, procerus, some lip elevator and some nasal muscles. The buccal branch has tremendous overlap with the zygomatic branch and sends fibers to similar muscles, as well
370 |
Practical Plastic Surgery |
|
|
|
|
|
|
|
Figure 60.1. Facial nerve anatomy.
as the buccinator, orbicularis oris, depressor anguli oris and risorius muscles. As the zygomatic and buccal branches exit the medial portion of the parotid, they travel along the superficial surface of the buccal fat pad, just below the SMAS. This position makes them susceptible to injury during facelift procedures, particularly at the lateral edge of the zygomaticus major. As discussed below, when dissecting in the sub-SMAS plane, the surgeon must change to a subcutaneous plane at the lateral border of the zygomaticus major muscle in order to avoid interrupting the zygomatic and buccal branches. Transection of the zygomatic and buccal branch leads to unpredictable defects because muscular innervation in the mid face is variable. The
60 buccal branch is the most commonly injured branch of the facial nerve.
The marginal mandibular nerve emerges from the inferior border of the parotid gland and crosses the inferior border of the mandible deep to the platysma to reach the face. Studies suggest that posterior to the facial artery, the marginal mandibular branch may dip as far as 2 cm below the border of the mandible. Anterior to the facial artery, the marginal mandibular nerve nearly always lies above the mandibular border. The marginal mandibular nerve has little cross-innervation as it enters the orbicularis oris and lip depressors. Transection of this nerve results in paralysis of the muscles that depress the corner of the mouth; therefore, the paralyzed side of the mouth will appear higher than the innervated side!
The cervical branch travels on the undersurface of the platysma. The platysma acts synchronously with other muscles of the lower lip to draw the oral commissure and lower lip downward. Transection of the cervical branch is uncommon, but it does not result in significant functional or cosmetic deficits.
Additional discussion of this anatomy can be found in Chapter 35.

Rhytidectomy |
371 |
Tear Trough, Nasojugal, Malar, Nasolabial and Labiomental Folds
The tear trough is a depression near the medial palpebral fissure formed by the separation of the orbicularis oculi and levator labii superioris. The nasojugal fold extends inferiorly and laterally from the tear trough onto the cheek. The malar fold runs inferiorly and medially from the lateral palpebral fissure towards the inferior extent of the nasojugal fold.
The cutaneous insertion of the zygomaticus major/minor and levator labii superioris muscles determines the nasolabial fold. In a sense, the nasolabial fold may be considered a fasciocutaneous ligament necessary for lip elevating muscles to initiate a smile. Laxity of this fasciocutaneous ligament causes the malar fat pad to travel inferomedially over the crease to deepen the nasolabial fold. The depressor anguli oris superiorly and the mandibular ligaments inferiorly determine the labiomandibular crease, which similarly is converted into a fold as a result of the laxity of the masseteric ligaments that occurs with age.
Parotid and Submandibular Salivary Glands
Invested by the deep fascia, 80% of the parotid gland lies between the mastoid process and the posterior border of the mandible. About 20% of the gland extends convexly forward over the masseter muscle occasionally as far as the zygomaticus major. The parotid duct (Stensen’s duct) and branches of the facial nerve emerge from the anterior border of the parotid, beneath the parotideomasseteric fascia. The parotid duct (4-6 cm in length) travels parallel to the zygomatic arch, 1.5 cm (approximately 1 finger breadth) below its inferior border, passing over the masseter muscle and then turns medially 90˚ to pierce the buccinator muscle at the level of the second maxillary molar where it enters the oral cavity. Using surface landmarks, Stensen’s duct lies midway between the zygomatic arch and corner of the mouth along a line between the upper lip philtrum and the tragus. The buccal branch of the facial nerve parallels the parotid duct.
The submandibular glands, often referred to as the submaxillary glands because of the tendency of British anatomists to refer to the mandible as the submaxilla, lie in the submandibular triangles formed by the anterior and posterior bellies of the digastric muscles and the inferior border of the mandible. The marginal mandibular branch of facial nerve courses superficial to the submandibular gland and deep to the platysma. The submandibular ducts (Wharton’s ducts) exit the medial surface of
each gland and run between the mylohyoid (lateral) and hyoglossus muscles along 60 the genioglossus muscle to empty into the oral cavity lateral to the lingual frenulum.
The lingual nerve wraps around Wharton’s duct, starting lateral and ending medial to the duct, while the hypoglossal nerve parallels the submandibular duct, just inferior to it. The identification of the hypoglossal and lingual nerves as well as Wharton’s duct is important prior to resecting portions of the submandibular glands.
Retaining Ligaments
The retaining ligaments of the face support soft tissues in their youthful anatomic positions. Furnas described four retaining ligaments that support the soft tissues of the face. The platysma-auricular and the platysma-cutaneous ligaments are aponeurotic condensations attaching platysma to dermis. Of greater significance are the osteocutaneous zygomatic and mandibular retaining ligaments. The zygomatic ligaments (McGregor’s patch) anchor the skin of the cheek to the inferior border of the zygoma just posterior to the origin of the zygomaticus minor muscle. With age, these
