
Practical Plastic Surgery
.pdf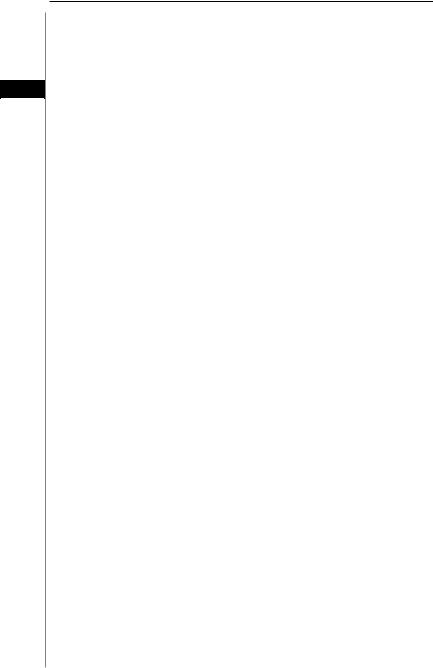
242 Practical Plastic Surgery
the maxilla is stabilized to the mandible with MMF. Any intraoral lacerations are repaired. Any orbital rim fractures are then repaired. Reconstruction of the orbits may require bone grafting, especially in restoration of the supraorbital ridge. The nasoethmoid region is dealt with including reduction of any nasal fractures and reattachment of the medial canthal tendons. The frontal bone and frontal sinus are
38 repaired when necessary. Finally, soft tissue lacerations and avulsions are repaired.
Complications of Facial Fractures
•Infection (sinusitis, meningitis, soft tissue infections)
•Brain damage
•Infraorbital nerve injury
•CSF rhinorrhea
•Ocular problems (e.g., blindness, diploplia, enophthalmos and telecanthus)
•Smell disturbances
•Nasal septal deviation
•Malocclusion
•Exposed or visible plates and screws
•Residual deformities in facial height and projection
•Malunion and nonunion
Pearls and Pitfalls
•The functional goals in midface fractures are restoration of orbital volume, movement and preinjury occlusion. The aesthetic goals include restoring the vertical height, the projection and the contours of the face. These goals should be kept in mind during any reconstruction.
•Maxillary fracture repair should begin with establishment of dental occlusion and placement of the patient in MMF, followed by restoration of the vertical buttresses using rigid fixation and bone grafting when indicated. Soft tissue repair comes last.
•Remember to resuspend the malar soft tissue after any subperiosteal dissection of the maxilla and zygoma. Failure to do so will result in a ptotic appearance of the cheek contour postoperatively. A cuff of periosteum should be preserved on the infraorbital rim to which the malar soft tissue can be reattached.
•Isolated zygomatic arch fractures are repaired when indicated with the Gillies’ approach (as described above). A common pitfall is to pass the instrument used to “pop” the arch outward in the wrong plane. Usually, this is in a plane that is too superficial. The correct plane should follow the course of the temporalis muscle and allow the instrument to easily insert underneath the zygomatic arch without any resistance.
Suggested Reading
1.Hendrickson M, Clark N, Manson PN et al. Palatal fractures: Classification, patterns and treatment with rigid internal fixation. Plast Reconstr Surg 1998; 101:319.
2.Manson PN, Clark N, Robertson B et al. Subunit principles in midface fractures: The importance of sagittal buttresses, soft-tissue reductions and sequencing treatment of segmental fractures. Plast Reconstr Surg 1999; 103:1287.
3.Markowitz BL, Manson PN. Panfacial fractures: Organization of treatment. Clin Plast Surg 1989; 16(1):105.
4.Pollock RA, Gruss JS. Craniofacial and panfacial fractures. In: Foster CA, Sherman JE, eds. Surgery of Facial Bone Fractures. New York: Churchill Livingstone, 1987.
5.Rudderman RH, Mullen RL. Biomechanics of the facial skeleton. Clin Plast Surg 1992; 19(1):11.

Chapter 39
Nasal and NOE Fractures
Clark F. Schierle and Victor L. Lewis
Introduction
The central location and prominent nature of the human nose renders it particularly vulnerable to the forces of blunt facial trauma. The nasal bones are the third most commonly fractured bones in the body after the clavicle and the wrist. They are the most common injured facial bones accounting for roughly half of all facial fractures. Despite this they are often overlooked or missed entirely. The nasoorbitoethmoid (NOE) complex is comprised of the confluence of several critical facial structures. Failure to recognize and treat nasal bone and NOE complex fractures in the appropriate time frame can lead to severe functional and cosmetic problems which can be more difficult to treat at a later time point.
Anatomy
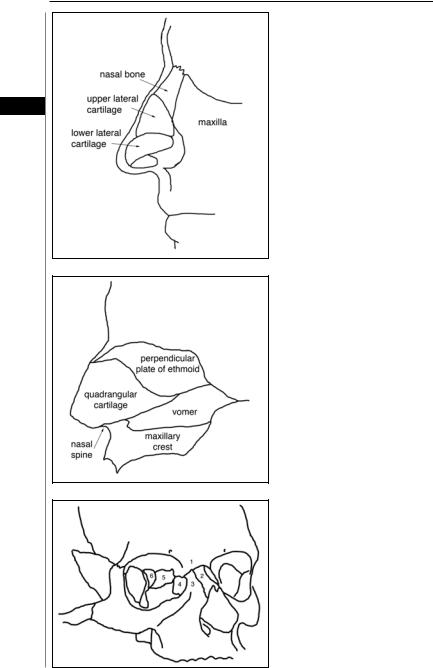
The bony pyramid of the nose is comprised of the paired nasal bones and frontal processes of the maxillary bones (Fig. 39.1). The nasal bones gradually thin as they meet the upper lateral cartilages caudally where they are most vulnerable to fracture. The upper lateral cartilage inserts on the undersurface of the nasal bone and contacts the quadrangular cartilage of the nasal septum anteriorly and the lower lateral cartilage caudally. The nasal septum is comprised of the quadrangular cartilage anteriorly, the perpendicular plate of the ethmoid bone posterosuperiorly, and the vomer bone posteroinferiorly (Fig. 39.2). The entire nasal structure rests on the groove of the maxillary crest terminating anteriorly at the nasal spine.
Fractures of the nasal bones also typically involve the bony or cartilaginous components of the nasal septum. Disruption of these structures can lead to inadequacy of the external nasal valve, formed by the angle of the upper lateral cartilages with the nasal septum, leading to chronic nasal airway obstruction. Cosmetic deformities include nasal asymmetry, inadequate dorsal support from the nasal septum resulting in a saddle nose deformity, or loss of tip support. This is due to deformation of the caudal septum or dissociation of the lower lateral cartilages from their supporting framework leading to a bulbous or drooping tip deformity.
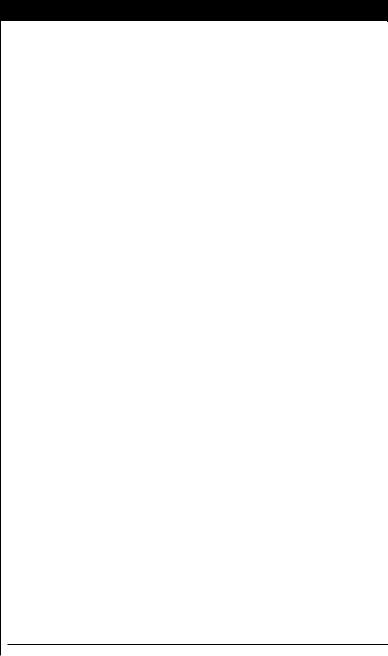
The NOE complex is formed by the confluence of the nasal, orbital, ethmoid and cranial cavities and is comprised of bony contributions from the nasal, maxillary, frontal, ethmoid, lacrimal and sphenoid bones (Fig. 39.3). The vertical support buttress of the NOE complex is comprised of the maxillary process of the frontal bone, the nasal bones and the frontal process of the maxilla. Violation of this buttress leads to disruption of the more delicate structures of the medial orbital wall including the lacrimal bones and laminae payraceae of the ethmoid bones. The horizontal buttresses of the NOE complex are the supraorbital and infraorbital rims. Violation of these supports may compromise the integrity of the superior aspect of the ethmoid
Practical Plastic Surgery, edited by Zol B. Kryger and Mark Sisco. ©2007 Landes Bioscience.
244
39
Practical Plastic Surgery
Figure 39.1. Lateral schematic view of the nasal bone and cartilages.
Figure 39.2. The components of the nasal septum.
Figure 39.3. The nasoorbitoethmoid (NOE) complex: frontal bone (1); nasal bone (2); maxilla (3); lacrimal bone (4); ethmoid bone (5); sphenoid bone-lesser wing (6).

Nasal and NOE Fractures |
245 |
bone as it forms the cribiform plate at the base of the anterior cranial fossa resulting in a leak of cerebrospinal fluid (CSF) or transection of the arteries that span the anterior and posterior ethmoid foramina leading to a vision-threatening orbital hematoma.
The medial canthal tendon (MCT) is an important soft tissue structure with a critical role in the diagnosis and treatment of NOE fractures. The MCT arises from the anterior and posterior lacrimal crests, envelops the lacrimal sac within the lacrimal fossa, and diverges to form the orbital, preseptal and pretarsal heads of the
orbicularis oculi muscle. The MCT provides a pumping action in the proper func- 39 tion of the lacrimal apparatus, as well as providing static support for the globe and dynamic support for the eyelid through the action of the orbicularis muscle. Frac-
ture of the NOE complex leads to lateral displacement of the MCT, resulting in the characteristic telecanthus which should trigger recognition of an underlying NOE fracture. Failure to properly reposition and fix the MCT in an anatomically correct location can result in a cosmetic deformity, lagophthalmos, or dysconjugate gaze.
Nasoorbitoethmoid fractures are classified into three types of increasing severity and difficulty of repair:
•Type I fractures have no comminution and involve only the segment of the medial orbit containing the MCT.
•Type II fractures involve comminuted bone external to the insertion of the MCT, and typically the MCT is still attached to a relatively large segment of the fracture.
•Type III fractures are bilateral and involve extension of comminuted bone beyond the insertion of the MCT.
Preoperative Considerations
Preoperative imaging of any patient with a suspected fracture of the facial skeleton should include dedicated facial bone CT scans with thin (<2 mm) cuts to provide adequate detail. In addition to the standard axial views, true coronal images should be obtained to properly assess the fracture in three dimensions. The extent of displacement is usually best visualized on one of the two series of cuts. If true coronal images are not obtainable (as in the presence of a cervical spine injury) reconstructed images may be adequate if the axial source images are of sufficient resolution.
Operative Technique
Nasal Fractures
Reduction of nasal fractures should be performed either immediately or after at least three to five days have passed to allow for some resolution of the initial inflammation and swelling. Nondisplaced fractures do not require treatment. Comparison with preinjury photographs can help guide reduction. Nasal fractures may be reduced with open or closed techniques. Isolated nasal bone fractures or fractures which displace the nasoseptal complex by less than half the width of the nasal bridge are candidates for closed reduction. More extensive or complex fractures generally benefit from an open approach to maximize exposure. If local anesthesia with sedation is to be used, the infratrochlear, infraorbital, supratrochlear and anterior ethmoidal nerves are blocked by injection of the nasal root, dorsum, lateral walls and anterior septum; 4% cocaine-soaked pledgets are inserted to minimize hemorrhage.
For the closed technique a blunt instrument such as a Boise elevator, empty scalpel handle or Asch forceps are introduced into the nose and controlled force applied in the direction opposite the fracturing force. Once all fractures are adequately mobilized, the symmetry of the nasal pyramid is restored by direct manipulation. Depending on

|
246 |
Practical Plastic Surgery |
||
|
|
the extent of septal involvement and the mobility of the nasal segments, internal (e.g., |
||
|
|
silastic splints or Merocel packing) or external (e.g., Aquaplast or a Denver splint,) |
||
|
|
splints may be placed to maintain fixation for one week postoperatively. |
||
|
|
Open reduction may be required if the nasoseptal deviation is too severe to be |
||
|
|
adequately addressed by the closed technique. A hemitransfixion incision at the |
||
|
|
caudal edge of the cartilaginous septum is used and mucoperichondrial flaps are |
||
|
|
elevated providing access to displaced fragments of the septum. Anchoring sutures |
||
39 |
||||
|
may help in stabilization of the caudal septum to the periosteum of the nasal spine. |
|||
|
|
Nasoorbitoethmoid Fractures |
|
|
|
|
NOE fractures necessitate an open approach. Choice of incision is determined |
||
|
|
by concerns for cosmesis, surgical exposure and location and orientation of any |
||
|
|
associated lacerations which may be exploited for access. Options include the tradi- |
||
|
|
tional vertical Lynch incision in the medial canthal region, lower lid subciliary or |
||
|
|
transconjunctival incisions, bicoronal incisions and medial conjunctival incisions |
||
|
|
through or around the lacrimal caruncle. Whatever the approach, dissection must |
||
|
|
be sufficient to expose the fracture segment and adequately identify the MCT and |
||
|
|
severity of the NOE fracture. Adequate reduction of the MCT is the goal of any |
||
|
|
operation to treat NOE fractures. If the MCT remains attached to a large piece of |
||
|
|
bone, miniplates and monocortical screws or steel wire may be used to reduce the |
||
|
|
MCT through bony fixation. If the MCT has been completely avulsed, reattach- |
||
|
|
ment is accomplished through wire fixation of a sturdy portion of the MCT to a |
||
|
|
hole drilled in the posterior lacrimal crest. In type II fractures, where there is disrup- |
||
|
|
tion or comminution of the anatomic point of fixation, transnasal fixation can re- |
||
|
|
store the appropriate vector of pull of the MCT. In type III fractures, the MCT is |
||
|
|
secured using wire passing through the nasal septum to the contralateral MCT. As |
||
|
|
the wire is tightened the MCTs are drawn medially. Care must be taken to pass the |
||
|
|
wire through a point in the septum that is sufficiently superior and posterior to |
||
|
|
recreate an appropriate vector of pull. |
|
|
Postoperative Care
Patients should be instructed to avoid nose-blowing and sneeze with an open mouth. Ice packs and head elevation help minimize swelling and discomfort. Splints and packing are removed at one week. Antibiotics are indicated if there are significant devitalized areas of cartilage or bone which must be treated functionally as grafts. Saline nasal spray can be used after packing is removed to aid in comfort and minimizing crusting. The role of antibiotics is not entirely clear; however many surgeons will prescribe 5-7 days of oral antibiotics. Steroids (e.g., methylprednisolone) can be given postoperatively to help minimize inflammation.
Pearls and Pitfalls
Although extremely rare, a septal hematoma must be ruled out in all nasal fractures. If untreated, the hematoma can lead to ischemic necrosis of the septal mucosa and consequent septal perforation. It is easy to diagnose and when present is quite striking. The mucosa is dark purple, dusky and bulging. Treatment consists of simply incising the mucosa and drainage of the blood.
The nose is extremely well-vascularized and tends to bleed a fair amount during nasal surgery. The use of lidocaine with epinephrine is essential, even when surgery is performed under general anesthesia. There is no point in using epinephrine if one

Nasal and NOE Fractures |
247 |
does not wait at least 10 minutes for its vasoconstrictive effects to kick in. Additional efforts to minimize bleeding should include intraoperative control of blood pressure (ideally maintaining a systolic blood pressure below 120 mm Hg), direct application of pressure when bleeding is significant, and avoidance of retching and coughing during extubation. Finally, prior to extubation, an oral gastric tube should be used to suck out as much blood as possible from the stomach, esophagus and
pharynx since ingested blood contributes to postoperative nausea.
39
Suggested Reading
1.Leipziger LS, Manson PN. Nasoethmoid orbital fractures. Current concepts and management principles. Clin Plast Surg 1992; 19(1):167.
2.Markowitz BL, Manson PN et al. Management of the medial canthal tendon in nasoethmoid orbital fractures: The importance of the central fragment in classification and treatment. Plast Reconstr Surg 1991; 87(5):843.
3.Mathog RH. Posttraumatic telecanthus. Facial Plast Surg 1988; 5(3):261.
4.Pollock RA. Nasal trauma: Pathomechanics and surgical management of acute injuries. Clin Plast Surg 1992; 19(1):133.
5.Rohrich RJ, Adams Jr WP. Nasal fracture management: Minimizing secondary nasal deformities. Plast Reconstr Surg 2000; 106(2):266.
Chapter 40
Mandible Fractures
Jeffrey A. Hammoudeh, Nirm Nathan and Seth Thaller
Introduction
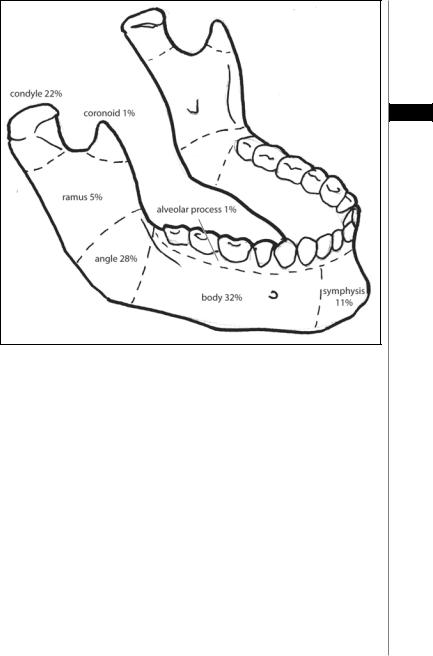
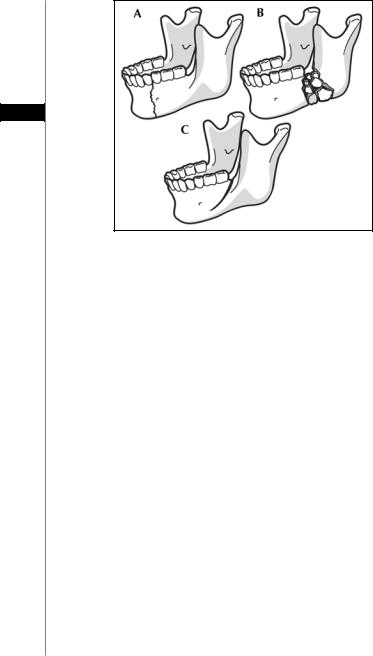
Mandibular fractures are the second most frequently occurring facial bone fracture, second only to nasal fractures and are the primary maxillofacial injury requiring hospitalization. Interpersonal violence and motor vehicle accidents remain the most common etiology of mandibular fracture with anatomic distribution as follows: body 29%, condyle 26%, angle 25%, symphysis 17%, ramus 4% and coronoid 1% (Fig. 40.1).
Classification
Accurate classification of mandibular fractures is important for both medicolegal documentation and communication among clinicians. In addition, this often determines selection of the optimal method for surgical fixation. Basic classification necessitates a concise description including anatomic location, type of fracture (simple vs. complex), degree of displacement and whether it is open or closed (Fig. 40.2). Fractures that communicate intraor extraorally are considered open fractures.
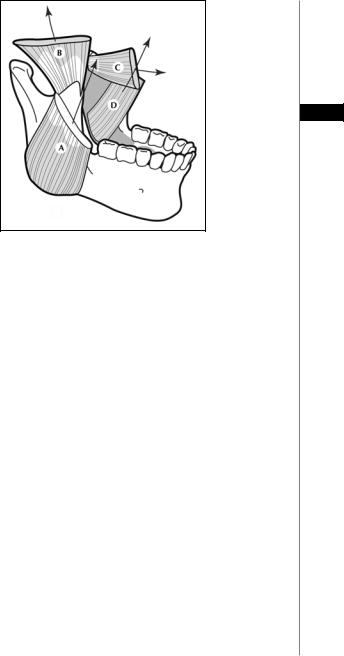
In the past fractures were also classified as either favorable or unfavorable (Fig. 40.3). This represents the relationship of the fracture segment to the vector that the associated musculature imposes on the bony segments. Favorable fractures are defined as those in which the muscle pull and the vector of displacement of the proximal fracture segment are in opposing directions, thereby preventing displacement. Unfavorable fractures occur when both muscle pull and the vector of displacement are in the same direction, resulting in bony displacement.
Diagnosis
Diagnosis of mandibular fractures can usually be made with an accurate and comprehensive history and physical exam. Initial questions should focus on the mechanism of injury and the location of impact. Predictable fracture patterns can help a clinician identify the correct diagnosis. For example, a chin laceration suggests an injury directly to the anterior mandible. This should also raise clinical suspicion of an associated contracoup injury to the contralateral condyle. Characteristic patterns of injury are based on a thorough knowledge of the underlying bony architecture and associated protective “fronts” of weakness within its horseshoe configuration. Common complaints include an abnormal bite, pain, swelling and altered sensation of the lower lip.
Physical findings generally include swelling, intraand extraoral ecchymoses, associated soft tissue lacerations, trismus, fractures or displaced teeth and malocclusion. Bimanual palpation, which is a necessary component of all head and neck exams, may confirm fracture location as well as degree of mobility. Neurosensory function of the
Practical Plastic Surgery, edited by Zol B. Kryger and Mark Sisco. ©2007 Landes Bioscience.
Mandible Fractures |
249 |
40
Figure 40.1. Mandible fracture pattern based on location and frequency.
inferior alveolar nerve using light touch, brush stroke and pinprick should be assessed. Fractures involving the angle or body may be associated with inferior alveolar nerve injury as it passes through the bony canal. It is imperative to document in the medical record completion of a neurosensory exam. The degree of eventual neurological return will vary depending on the location and displacement of the fracture. In approximately 85% of mandibular fractures, the neurosensory status was unchanged or improved after treatment. Fractures with greater than 5 mm displacement were associated with a six-fold increased risk for a decreased neurosensory score.
Imaging
Suspected mandibular fractures should be verified with a CT scan and a panoramic radiograph, or Panorex®. The Panorex® is especially useful in ruling out a fracture line that crosses the root of a tooth, since this can be missed even on a CT scan with thin cuts. The limitation of the panorex is that it necessitates the patient remain in the upright position for the duration of the radiography.
Since associated injuries are encountered in approximately 43% of mandibular fractures (11% of these injuries being cervical fractures), it is imperative for the clinician to rule out any associated cervical fractures via the appropriate radiological studies such as helical CT scans. Three-dimensional reformatted CT images can be helpful in visualizing the fracture and communicating management options to patients and families but
250 |
Practical Plastic Surgery |
40
Figure 40.2. Fracture type based on complexity. A) Simple nondisplaced fracture. B) Complex comminuted fracture. C) Greenstick fracture.
are usually not necessary for clinical diagnosis. In the poly-trauma patient, CT imaging may be the only modality available for clinical assessment. For the evaluation of the condylar and subcondylar regions, CT imaging is the method of choice.
General Principles of Treatment
Immediate relief of pain is achieved by temporary immobilization of the fracture with Barton’s head dressing, narcotic analgesics, topical ice therapy and a mechanically soft or pureed diet. Narrow spectrum antibiotics should be given immediately, especially in open fractures. Options include penicillin, clindamycin, or cefazolin. Definitive fracture management should be initiated as soon as practically possible, following stabilization of the patient’s overall medical condition.
Two general treatment options are available: maxillomandibular fixation (MMF) alone or with open reduction internal fixation (ORIF). Closed treatment depends solely on the placement of MMF permitting secondary fracture healing by immobilization of the jaws. ORIF, on the other hand, will allow for primary bone healing. At the completion of ORIF, the MMF may be released, allowing for early mobilization. This is especially important for complex fractures involving the condylar region in which early motion will decrease the potential for development of temporomandibular joint (TMJ) dysfunction.
Condylar and Subcondylar Fractures
Condylar fractures are relatively common and constitute approximately 25% of all adult mandibular fractures (due to an inherent weakness of the condylar neck that helps prevent impaction of the condyles into the cranial vault). These fractures are often associated with a fracture at a second site, in particular parasymphyseal fractures. Definitive management options remain controversial.
Mandible Fractures |
251 |
40
Figure 40.3. Displacement of fracture is based on the relationship of the muscle vector force with the angulation of the proximal/distal fracture segments. A) The masseter will try to displace the proximal fracture segment superolaterally. B) The temporalis muscle will try to displace the condylar segment superiorly. C) The medial pterygoid will try to displace the proximal fracture segment medially. D) The lateral pterygoid will try to displace the proximal sebment superiorly.
Classification
Classification of condylar fractures is based on location or displacement. A favorable condylar fracture is defined as minimally displaced or nondisplaced. Associated mild malocclusion can usually be treated through closed reduction technique. Our recommendation is 10 days of MMF followed by 10 days of elastics Ivy loops, a full MMF course, or four-point screw fixation. If the occlusion is stable, elastics may be removed and the patient should be continued on a mechanical soft diet. Reevaluation should be performed after 10 to 14 days and, if the occlusion is reproducible; a Panorex® should confirm a well-aligned, healing fracture. Arch bars may then be removed.
Unfavorable or displaced condylar fractures can be treated by either closed reduction or in certain specific instances with ORIF. Displacement of the proximal segment is caused by the insertion of the lateral pterygoid muscle resulting in one of the following: displacement anteromedially, laterally towards the zygoma, posteriorly towards the ear canal, or superiorly into the middle cranial fossa. Most cases, however, result in a medially displaced proximal fragment leading to a shortening of the ramus and an open bite deformity. Some institutions advocate initial closed reduction in this situation. This is based on data that evaluated the risks of ORIF vs. MMF which showed that adequate results can be obtained with closed reduction. However, as rigid fixation techniques have improved, and more critical data regarding ORIF vs. MMF has emerged, ORIF is now advocated by certain authors. In our opinion, the decision on when to treat with MMF vs. ORIF must incorporate other individual factors such as clinician experience, patient needs and associated facial features. One should further evaluate condylar fracture based on the specific anatomic location and the ability to actually position and fixate segments.
