
Practical Plastic Surgery
.pdf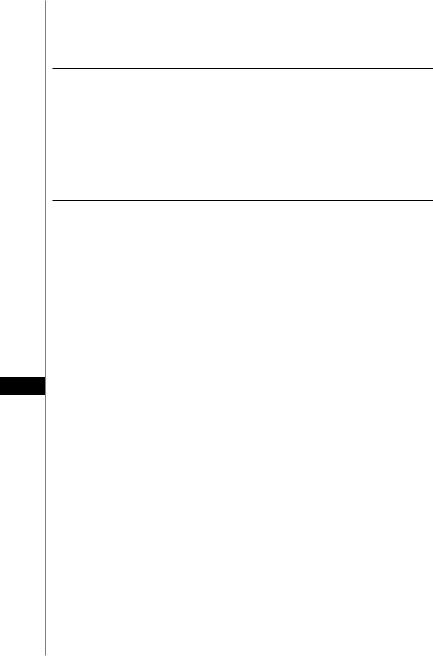
342 |
Practical Plastic Surgery |
|
|
|
|
Table 56.2. The Munro and Lauritzen classification of craniofacial microsomia. There is a progressive addition of abnormalities, ranging from Type IA, the least severe, to Type V, the most severe.
Type |
Description |
IA |
Mild craniofacial skeletal hypoplasia, normal occlusion plane |
IB |
Mild craniofacial skeletal hypoplasia, canted occlusion plane |
II |
Absent condyle, part of the ramus |
III |
Absent condyle, part of the ramus, glenoid fossa, zygomatic arch |
IV |
Absent condyle, part of the ramus, glenoid fossa, zygomatic arch, |
|
hypoplastic zygoma, lateral orbital wall displaced |
VAbsent condyle, part of the ramus, glenoid fossa, zygomatic arch, inferior orbit displacement with loss of orbital volume
Pearls and Pitfalls
•Roughly 25% of patients with craniofacial microsomia have obstructive sleep apnea (OSA). Infants with more severe mandibular and orbital deformities appear at a greater risk for OSA. Macrostomia can also result in airway obstruction. Therefore, all children with craniofacial microsomia should undergo evaluation for airway difficulties and OSA prior to undergoing any other types of reconstructive surgeries.
•The importance of treating children with craniofacial microsomia is underscored by the fact that facial asymmetry is progressive in this condition. Untreated children will develop worsening degrees of bony and soft tissue asymmetry. Further-
more, the more severe the deformity, the worse the asymmetry will become if left untreated.
56• Treatment of the soft tissue defects in this condition range from injection of fillers to free tissue transfer. The amount of soft tissue that is missing will dictate the treatment. The soft tissue defect should be addressed after the major skeletal reconstruction has taken place. For mild defects, fillers (e.g., Sculptra®) and fat injections work well. Medium-sized defects can be addressed with Alloderm® or silicone implants. Larger defects may require a dermal fat graft or even a free tissue transfer of fat (e.g., DIEP flap).
Suggested Reading
1.Kearns GJ et al. Progression of facial asymmetry in hemifacial microsomia. Plast Reconstr Surg 2000; 105:492.
2.McCarthy JG, Schreiber JS, Karp NS et al. Lengthening of the human mandible by gradual distraction. Plast Reconstr Surg 1992; 89:1.
3.McCarthy JG. Craniofacial microsomia. Grabb and Smith’s Plastic Surgery. 5th ed. Philadelphia: Lippincott-Raven, 1997:305.
4.Mulliken JB, Kaban LB. Analysis and treatment of hemifacial microsomia in childhood. Clin Plast Surg 1987; 14:91.
5.Munro IR, Lauritzen CG. Classification and treatment of hemifacial microsomia. In: Caronni EP, ed. Craniofacial Surgery. Boston: Little, Brown and Co., 1985:391.
6.Vento AR, LaBrie RA, Mulliken JB. The O.M.E.N.S. classification of hemifacial microsomia. Cleft Palate-Craniofac J 1991; 28:68.
Chapter 57
Microtia Repair
Zol B. Kryger
Introduction
Microtia ranges from a very mild form in which the ears are grossly normal but prominent, to complete absence of the ear, termed anotia. Severe abnormalities occur in roughly 1 in 8,000 births. There is a predisposition of microtia to occur in males, with a male: female ratio of about 2:1. The right side is also twice as likely to be affected as the left, and bilateral cases occur in 10% of cases. Microtia is most commonly described according to the classification described by Tanzer (Table 57.1).
Preoperative Considerations
There are a number of congenital conditions associated with microtia:
•Narrowing or atresia of the external auditory canal (very common)
•Middle ear abnormalities (very common)
•Combined ear canal and middle ear abnormality
•Cleft lip or palate
•Facial nerve abnormality
•Hemifacial microsomia (in about half of microtia cases)
•Cardiac or urogenital defects
Middle ear abnormalities are more likely to occur the more severe the degree of microtia. The tragus is the structure that is most highly correlated with the presence of an adequate middle ear cleft.
Hearing
All patients with microtia should undergo hearing evaluation, either with an audiogram or auditory brainstem response testing. Hearing loss can be either conductive or sensorineural. Conductive deafness is more common in microtia. Children with unilateral microtia and normal hearing in the contralateral ear will develop normal speech. In bilateral microtia cases, a hearing aid is required for normal speech development. This will often be a bone conduction hearing aid that is fitted shortly after birth. Most commonly, a percutaneous, bone-anchored hearing aid is used. At
Table 57.1. Classification of microtia
Grade |
Description |
I |
Anotia |
II |
Complete hypoplasia (± atresia of the external auditory canal) |
III |
Middle third auricular hypoplasia |
IV |
Superior third auricular hypoplasia |
V |
Prominent ears |
Practical Plastic Surgery, edited by Zol B. Kryger and Mark Sisco. ©2007 Landes Bioscience.

344 |
Practical Plastic Surgery |
about the age of four, a CT scan of the middle ear is useful to determine whether the middle ear is amenable to reconstruction by the otologist.
Timing of the Repair
Most experienced surgeons who treat microtia wait until the child is 5-7 years old before considering reconstruction. Some have reported auricular framework reconstruction as early as 2 to 3 years of age. There are a number of reasons to wait until the child is around 6 years old. First, this is the age that children will usually begin to tease other children with different appearances. The child is more likely to cooperate with the postoperative regimen. Second, by the age of 6, the normal ear has almost fully developed, reaching 85% of its full size. Third, the rib cartilage has sufficiently developed by this age, and it can provide an adequate framework for auricular construction.
In general, when microtia is unilateral, middle ear atresia repair is not indicated since unilateral hearing is sufficient. In bilateral cases, repair of the atresia on at least one side is usually required. If middle ear surgery is indicated, it should be postponed until after completions of the first stage of the auricular reconstruction-insertion of the costal cartilage framework. This is due to the fact that atresia surgery preceding auricular reconstruction can result in scarring and impaired vascularity in the mastoid region.
The size of the auricular framework is controversial. According to Brent, it should be matched to create an ear that is as close to the size of the normal one as possible. The rationale for this is that the cartilaginous framework continues to grow at roughly the same pace as the cartilage of the normal ear. Some surgeons, however, will create a framework that is a few millimeters larger than the other ear. They feel that the other side will “catch up” with the reconstructed ear.
Intraoperative Considerations
Microtia repair is a multi-stage procedure. Although the timing and sequence of the reconstruction is variable, a number of steps are generally followed. Brent and Tanzer each advocate following these steps:
57Step I—cartilage framework construction and placement Step II—transposition of the lobule
If indicated—atresia repair
Step III—construction of the tragus and conchal cavity
Step IV—creation of the auriculocephalic sulcus
A number of the steps can be combined, such as performing tragal reconstruction in combination with the initial cartilage framework placement, or repair of the lobule during step I. The approach that is chosen must be tailored to the individual’s wishes and unique anatomy. If atresia repair is undertaken, an oval shape of skin is excised when creating the conchal cavity. This will serve as the opening of the reconstructed auditory canal. The canal is lined with a skin graft.
In contrast to the multi-step microtia repair, Nagata has described a two-stage approach that encompasses the steps described above. The initial procedure consists of fabrication of the costal cartilage framework, rotation of the lobule, conchal accentuation and fashioning of the tragus. The second stage focuses primarily on ear elevation and creation of the auriculocephalic sulcus.
The Auricular Framework
The framework can be either autologous, using costal cartilage, or alloplastic, composed of a synthetic material.
Microtia Repair |
345 |
Alloplastic Framework
A number of materials have been used to create auricular frameworks. Currently, the most commonly used substances are silastic or porous polyethylene mold. Allopastic frameworks have a higher risk of erosion and exposure compared to autogenous ones. Factors contributing to this high rate of extrusion are scar tissue, excessively thin skin, tension over the implant, trauma and infection. Nevertheless, with adequate soft tissue coverage, such as the temporoparietal fascial flap-described below, alloplastic frameworks can be used successfully. Most authors feel that they are a second choice to costal cartilage.
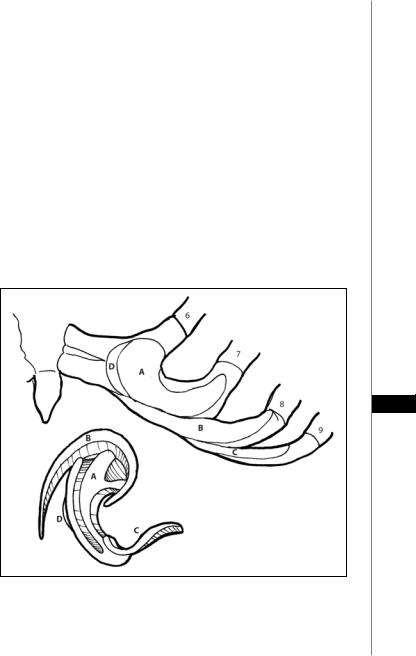
Autogenous Framework
Costal cartilage can be taken from the 6th, 7th, 8th and 9th ribs. A large piece is cut out from the 6th and 7th ribs and used for the body of the framework. A smaller adjacent wedge is removed and will be banked for future use during ear elevation. Two thin, smaller pieces are taken from the 8th and 9th ribs and used to create the helix and a strut for the tragus (Fig. 57.1). The cartilage can be removed along with the perichondrium, or the dissection can be subperichondrial, as advocated by Tanzer, leaving the perichondrium behind. Some authors prefer to use the ipsilateral ribs, whereas others use the contralateral side (as shown in Fig. 57.1). After removal of the cartilage and closure of the donor site, the pieces of
57
Figure 57.1. The auricular framework. Harvesting the cartilage framework from the contralateral costal cartilage (above). Segment 4 is banked for use in the final procedure of ear elevation by creating greater projection. Creating the framework from the segments labeled 1 (main body), 2 (helical rim) and 3 (tragus). The pieces of cartilage are sutured together using 4-0 and 5-0 clear nylon sutures (below).

346 |
Practical Plastic Surgery |
cartilage are carefully carved into the desired shapes with a scalpel and chisels. In adults, the rib cartilages are often fused and the entire framework must be sculpted as a single unit.
The framework is inserted into a pocket in the desired auricular region. The pocket must be much larger than the framework in order to have a tension free closure. Suction tubing attached to vacuum test-tubes is used to adhere the skin envelope to the framework. Problems with the hairline or inadequate tissue for coverage are described below.
Postoperative Considerations
Most children will be hospitalized for one to two days. The suction test tubes are changed daily for 5 days postoperatively and then removed. This system provides adequate compression; therefore the external dressing does not need to be compressive. Sports are restricted for 4-6 weeks, for protection of the ear as well as the chest wound. Patients are not instructed to avoid sleeping on the operative site, because most children turn in their sleep and will not be able to comply with this instruction.
Complications
As mentioned previously, alloplastic frameworks have a higher extrusion rate than for costal cartilage frameworks. Extrusion requiring removal occurs in 5-30% of silastic frameworks, compared to 1-2% for costal cartilage. Other complications include infection, hematoma and skin loss. These are usually minor, and the framework can almost always be salvaged. Donor site complications include unacceptable chest scars, mild to severe retrusion and flattening of the rib cage contour.
Auricular Prosthesis
An alternative to surgical reconstruction of the ear is to use an auricular prosthesis. In select patients, it is an excellent alternative. Its use precludes any inner ear surgery. The following patients should be considered for an auricular prosthesis:
• Major auricle loss after cancer resection
57• Absence of the lower half of the ear
•Poor quality of local tissue
•Patients at high risk for general anesthesia
•Poorly compliant patients
•Salvage after unsuccessful reconstruction
Osseointegrated titanium implants are first implanted in the mastoid bone. Once the implants have healed completely, an auricular silicone prosthesis that matches the other side is created. The titanium abutments protruding through the skin attach to the prosthesis by one of a variety of mechanisms. No glue is necessary. The prosthesis can easily be removed and the area cleaned thoroughly.
Pearls and Pitfalls
Two commonly encountered problems in microtia repair are a low hairline and inadequate coverage.
Low Hairline
A low hairline is a frequently encountered problem. A number of techniques for dealing with this problem have been described. If hair covers only the upper helix, it can be removed by electrolysis. If it covers the entire upper third of the ear, the hair-bearing skin can be excised, and the defect covered with a graft from

Microtia Repair |
347 |
|
|
the contralateral postauricular region. Perhaps the most precise and least morbid |
|
||
technique is to use a laser for hair removal as a first step. This can create the ideal |
|
||
hairline prior to insertion of the framework. |
|
|
|
Inadequate Coverage |
|
|
|
The Temporoparietal Fascial Flap |
|
|
|
The temporoparietal fascial flap is very effective for obtaining additional soft |
|
||
tissue coverage over the auricular framework in cases in which the skin is overly thin, |
|
||
poorly vascularized, or the pocket is too small. This fascial flap is based on the super- |
|
||
ficial temporal artery. It is usually elevated from the ipsilateral side. It is inferiorly |
|
||
based, and raised off the underlying deep temporal fascia. It is turned over to cover |
|
||
the framework and coapted to it by suction drainage. A thick split-thickness or |
|
||
full-thickness skin graft is used to cover it. If this fascial flap dehisces and the frame- |
|
||
work becomes exposed, a salvage procedure has recently been described using the |
|
||
deep temporal fascia. |
|
|
|
Tissue Expansion |
|
|
|
Tissue expansion has also been described as an attempt for obtaining addition |
|
||
soft tissue in cases of severe skin shortage, or a low hairline. The long-term results |
|
||
with expansion have been disappointing. The skin in this region is relatively inelas- |
|
||
tic. In response to expansion, a thick capsule forms which can obscure the details of |
|
||
the auricular framework. In addition, the expanded skin contracts and can compro- |
|
||
mise the framework. |
|
|
|
Suggested Reading |
|
|
|
1. Aguilar IIIrd EF. Auricular reconstruction of congenital microtia (grade III). Laryngo- |
|
||
scope 1996; 106(82):1. |
|
|
|
2. Brent B. Auricular repair with autogenous rib cartilage grafts: Two decades of experi- |
|
||
ence with 600 cases. Plast Reconstr Surg 1992; 90:355. |
|
|
|
3. Brent B. Technical advances in ear reconstruction with autogenous rib cartilage grafts: |
|
||
Personal experience with 1200 cases. Plast Reconstr Surg 1999; 104(2) :319. |
|
|
|
|
|
57 |
|
4. Cronin TD, Ascough BM. Silastic ear reconstruction. Clin Plast Surg 1978; 5:367. |
|||
5.Edgerton MT. Ear reconstruction in children with congenital atresia and stenosis. Plast Reconstr Surg 1969; 43:373.
6.Hackney FL. Plastic surgery of the ear. Selected readings in plastic surgery 2001; 9(16):9.
7.Nagata S. Modification of the stages in total reconstruction of the auricle: Part I-IV. Grafting the three-dimensional costal cartilage framework for lobule type microtia. Plast Reconstr Surg 1994; 93:221.
8.Tanzer RC. Congenital deformities of the auricle. In: Coverse JM, ed. Reconstructive Plastic Surgery. 2nd ed. Philadelphia: WB Saunders, 1977.
9.Tanzer RC. Total reconstruction of the auricle. The evolution of a plan of treatment. Plast Reconstr Surg 1971; 47:523.
Chapter 58
Cleft Lip
Alex Margulis
Introduction
A cleft lip is more accurately described as a cleft lip, nose and alveolar deformity because all of these anatomic structures are commonly affected. As the deformity worsens, the effect on the lip, nose and alveolar structures become more apparent.
There is no agreement on the ideal timing and the technique of repair. Advocates of different methods may demonstrate results that are comparable, underscoring the fact that more than one treatment plan is acceptable. Total familiarity with the details and limitations of a technique is as important as the type of repair chosen.
Brief History
Modern repairs have in common the use of a lateral lip flap to fill a medial defect, a concept that can be credited to Mirault. The LeMesurier repair involves the lateral quadrilateral flap, whereas the Tennison repair employs a lateral triangular flap.
In 1955, Millard described the concept of advancing a lateral flap into the upper lip combined with downward rotation of the lower segment. The benefits are twofold: the incision lines follow the natural anatomic position of the philtral column, and placement of scars across the philtrum in the lower part of the lip is avoided. This technique has become popular because of its aesthetic advantages.
More recently, emphasis has shifted away from skin flap design and has been placed on accurate and functional reconstruction of the orbicularis oris muscle and on primary nasal reconstruction. The concept of differential reconstruction of the orbicularis oris muscle was emphasized by Miller. McCoomb, Anderl, Salyer and others have championed primary nasal tip-plasty. Primary nasal repair can achieve long-lasting improvements that can be achieved without detrimental effects on the growth and development of nasal tip cartilages.
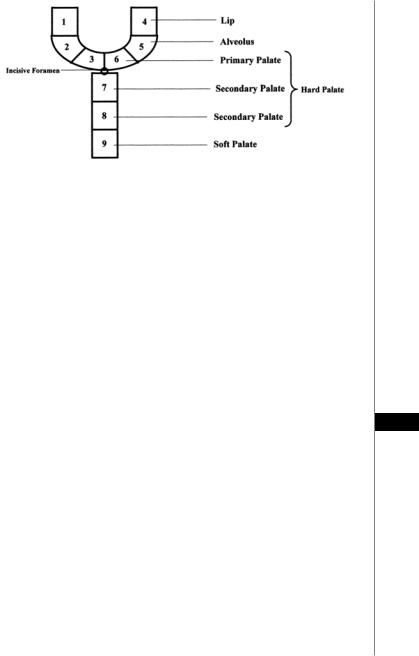
Classification
Accurate analysis and reporting of the cleft lip and palate deformity should be done in a standardized manner. Many different classification systems were introduced over the years. In 1971, Kernahan introduced a simple classification scheme that may be reported on a diagrammatic Y-shaped symbol with the incisive foramen represented at the focal point (Fig. 58.1). This was subsequently modified by Millard, and other versions were later proposed to allow easier analysis, reporting and surgical planning.
Embryology
The branchial arches are responsible for the formation of the face, neck, nasal cavities, mouth, larynx and pharynx. The first branchial arch contributes to the maxillary and mandibular prominences. The paired maxillary and mandibular prominences form the lateral and caudal borders of the stomodeum (primitive mouth)
Practical Plastic Surgery, edited by Zol B. Kryger and Mark Sisco. ©2007 Landes Bioscience.
Cleft Lip |
349 |
||
|
|
|
|
|
|
|
|
Figure 58.1. The Kernahan Y classification system for cleft lip and palate.
respectively. The frontonasal prominence, a central process formed by the proliferation of the mesenchyme ventral to the forebrain, forms the cranial boundary of the stomodeum by merging with the first arch derivatives. These five facial prominences are responsible for the development of adult facial features.
The mesenchyme of all five facial prominences that border the stomodeum is continuous; therefore mesenchymal migration may occur freely between the facial prominences. The fusion of the medial nasal, lateral nasal and the maxillary prominences produces continuity between the nose, upper lip and palate. Facial development occurs between the fourth and eight weeks. By the age of 10 weeks the face has a clearly human appearance.
Unilateral cleft lip results from failure of fusion of the medial nasal prominence and maxillary prominence on one side. A bilateral cleft lip results from failure of fusion of the merged medial nasal prominences with the maxillary prominences on both sides.
Etiology
Clefting is multifactorial, with both genetic and environmental causes cited. The observation of clustered cases of facial clefts in a particular family indicates a genetic 58 basis. Approximately 33% to 36% of cases have a positive family history for clefting. Clefting of the lip and/or palate is associated with more than 150 syndromes. The overall incidence of associated anomalies (e.g., cardiac) is approximately 30% (more common with isolated cleft palate). Environmental causes such as viral infection (e.g., rubella) and teratogens (e.g., steroids, anticonvulsants, alcohol and smoking) during
the first trimester have been linked to facial clefts. The risk also increases with advanced parental age, especially when older than 30 years, with the father’s age appearing to be a more significant factor than the mother’s age. Nevertheless, most presentations are of isolated patients within the family without an obvious etiology.
Incidence and Epidemiology
Ethnic variations exist in the incidence of clefting. The incidence is approximately 2.1 per 1000 live births in Asians, 1:1000 in Caucasians and 0.41:1000 in African-Americans. Isolated clefts of the lip occur in 21% of the affected population, while 46% of cases involve clefts of the lip and palate and 33% are isolated clefts of the palate. Clefts of the lip are more commonly left sided and unilateral (6: 3: 1 left: right: bilateral) and show a male predominance.

350 |
Practical Plastic Surgery |
Clinical Findings
Unilateral clefts are placed in one of three categories for the purpose of treatment planning: microform cleft lip, incomplete cleft lip or complete cleft lip. The associated nasal deformity is categorized as mild, moderate or severe.
The unilateral complete cleft lip involves a full-thickness defect of the lip and alveolus (primary palate) and often is accompanied by the palatal cleft (secondary palate). The premaxilla typically is rotated outwardly and projects anterior in relation to a relatively retropositioned lateral maxillary alveolar element. The nasal structures of the ala base, nasal sill, vomer and septum are distorted significantly. The lower lateral cartilage on the cleft side is positioned inferiorly, with an obtuse angle as it flattens across the cleft. The alar base is rotated laterally, inferiorly and posteriorly (acronym LIP). The developing nasal septum pulls the premaxilla away from the cleft, and the septum and the nasal spine are deflected toward the noncleft side. The cleft continues through the maxillary alveolus and palatal shelf, extending to the palatal bone and soft palate.
The bilateral cleft lip may be either complete or incomplete. The complete cleft lip involves the entire upper lip, with the cleft traversing the alar base and potentially involving the primary and secondary palates. The anatomic components of the bilateral cleft lip include widened alar bases with flared internal nasal valves; a shortened columella; excessively obtuse nasolabial angles; a hypoplastic prolabium; a vertically short upper lip; protruding premaxillary segment; absence of the orbicularis oris muscle in the prolabial segment; absence of the philtral dimple, columns and tubercle; absence of Cupid’s bow; aberrant insertion of the lateral lip orbicularis oris muscle into the alar bases; and potential involvement of the primary and secondary palates.
Timing of Repair and Treatment Planning
The goals of reconstruction include restoring the normal morphologic facial form and function as they are related intimately for proper development of dentition, mastication, hearing, speech and breathing. A multidisciplinary team approach is ideal because it provides a setting in which parents can recognize that there is a plan that will be carried out over a long term in a coordinated and specialized fashion by ex-
58 perts who are interested, educated and experienced in the care of children with clefts. Presurgical orthodontic treatment is initiated in the first or second week following birth, with the maximum response occurring during the first six weeks. The lip repair with the orbicularis oris muscle reconstruction and primary nasal repair are deferred until the patient is 2 to 3 months of age. Some centers will perform alveolar closure when the segments are ideally aligned and <2 mm apart (gingivoperiosteoplasty). In our center primary alveolar bone graft is performed as a separate procedure when the child is 6 to 8 months of age and the segments are aligned. Closure of the palatal cleft
is accomplished when the patient is approximately 10 to 12 months of age.
When alveolar closure is not completed in the first year of life, a definitive two-layer closure of the alveolus with cancellous bone grafting is performed between 7 and 9 years of age. The timing of this closure is mitigated by presurgical orthodontic treatment to align the segments and the guideline of obtaining surgical closure and bone grafting before eruption of the permanent canine teeth. Further correction of the nasal deformity, if required, is deferred until late adolescence.
Relevant Anatomy
An understanding of normal lip and nasal anatomy is essential for achieving a satisfactory repair. The elements of the normal lip are composed of the central phil-

Cleft Lip |
351 |
trum, demarcated laterally by the philtral columns and inferiorly by Cupid’s bow and tubercle. Just above the junction of the skin-vermilion border lies a mucocutaneous ridge known as “the white roll.” Within the red portion of the lip is the wet-dry junction demarcating the moist (inner) mucosa from the dry (outer) vermilion, the increased keratinized portion of the lip that is exposed to air.
The primary muscle of the lip is the orbicularis oris, and it has two well-defined components: the deep (internal) and the superficial (external). The deep fibers run horizontally or circumferentially from commissure (modiolus) to commissure and function as the primary sphincter of the mouth. The superficial fibers run obliquely, interdigitating with the other muscles of facial expression to terminate in the dermis. They provide subtle shades of expression and precise movements of the lip for speech. The superficial fibers of the orbicularis decussate in the midline and insert into the skin lateral to the opposite philtral groove forming the philtral columns. The resulting philtral dimple centrally is depressed as there are no muscle fibers that directly insert into the dermis in the midline. The tubercle of the lip is shaped by the pars marginalis, the portion of the orbicularis along the vermilion forming the tubercle of the lip with eversion of the muscle.
In the upper lip, the levator labii superioris contributes to the form of the lip. Its fibers, arising from the medial aspect of the infraorbital rim, sweep down to insert near the skin-vermilion junction. The medial-most fibers of the levator labii superioris sweep down to insert near the corner of the ipsilateral philtral column helping to define the lower philtral column and the peak of the Cupid’s bow.
The nasal muscles are equally important. The levator superioris alaeque arises along the frontal process of the maxilla and courses inferiorly to insert on the mucosal surface of the lip and ala. The transverse nasalis arises along the nasal dorsum and sweeps around the ala to insert along the nasal sill from lateral to medial into the incisal crest and anterior nasal spine. These fibers join with the oblique fibers of the orbicularis and the depressor septi (nasalis), which arises from the alveolus between the central and lateral incisors to insert into the skin of the columella to the nasal tip and the footplates of the medial crura.
A unilateral or bilateral cleft disrupts the normal termination of the muscle fi-
bers that cross the embryologic fault line of the maxillary and nasal processes. This 58 results in asymmetric (or symmetric but abnormal) muscular forces between the nasolabial and oral groups of muscles. With an unrestrained premaxilla, the defor-
mity accentuates with differential growth of the various elements. The alar cartilages on the cleft side are splayed apart and rotate caudally, subluxed from the normal position. Consequently, the nasal tip broadens, the columella is foreshortened and the alar bases rotate outwardly and cephalad.
Laboratory and Imaging Studies
Routine lab studies are not necessary in otherwise healthy infants with a cleft. Some centers obtain a blood count as a routine study before performing surgery on a child with cleft. At our institution, we do not find this necessary unless some other associated medical conditions coexist. The child’s weight, oral intake and growth and/ or development are of primary concern and must be followed closely. Routine imaging studies are also not needed in otherwise healthy infants who undergo cleft lip repair.
Diagnostic Procedures
Early collaboration with an audiologist and an otolaryngologist, including examination and early audiologic assessment; can prevent long-term hearing deficits
