
Practical Plastic Surgery
.pdf
282 |
Practical Plastic Surgery |
•If IMF elevation is needed, utilize a monofilament suture such as a 2-0 PDS. The suture should be placed from the subcutaneous or dermal tissue of the newly marked IMF to the chest wall, preferably on the rib periosteum. Place sutures as needed and they can remain 3-4 cm apart. Sutures can also be bought out transcutaneously and tied to a xeroform or telfa bolster, but these sutures can only remain in about one week.
Suggested Reading
1.Alderman AK, Wilkins EG, Kim HM et al. Complications in postmastectomy breast reconstruction: Two-year results of the Michigan Breast Reconstruction Outcome Study. Plast Reconstr Surg 2002; 109(7):2265.
2.Bostwick III J. Tissue expansion reconstruction. Plastic and Reconstructive Breast Surgery. 2nd ed. St. Louis: Quality Medical Pub., 2000:811.
3.Spear SL, Beckenstein MS. Breast reconstruction with implants and tissue expanders.
44In: Evans GRD, ed. Operative Plastic Surgery. New York: McGraw-Hill Professional (Appleton and Lange), 2000:635.
4.Spear SL, Majidian A. Immediate breast reconstruction in two stages using textured, integrated-valve tissue expanders and breast implants: A retrospective review of 171 consecutive breast reconstructions from 1989 to 1996. Plast Reconstr Surg 1998; 101(1):53.
5.Spear SL. Spittler CJ. Breast reconstruction with implants and expanders. Plast Reconstr Surg 2001; 107(1):177.

Chapter 45
Nipple Reconstruction and Tattooing
Kristina D. Kotseos and Neil A. Fine
Introduction
The final stage in breast reconstruction is creation of the nipple-areolar complex (NAC), which carries aesthetic and psychological importance to patients with congenital and acquired breast absence, whether from trauma, burns, or after mastectomy for cancer treatment. Nipple-areola reconstruction (NAR) began 40 years ago with the initial creation of both the nipple and areola from distant grafts. Subsequently, this approach transformed into a combination of local flaps for nipple reconstruction and distant grafts for the areola. Many of the earlier methods for nipple reconstruction are no longer used and have been relegated to historical significance including nipple banking due to spread of cancerous cells, nipple sharing due to insult on the contralateral nipple and free composite grafts of tissue from distant sites due to donor site morbidity. The current trend is the use of local dermal flaps alone with tattooing. These methods have proven to be cost-effective and carry low morbidity. These evolving techniques and modifications of NAR are based on simplicity and reliability; however, all are hampered to some extent by loss of long-term nipple projection. The goal of reconstruction is to create an aesthetically pleasing nipple areola complex with maintenance of nipple projection, symmetry and color. Although there have been numerous articles published regarding patient satisfaction, overall nipple projection and optimal color match of different methods, no one technique has proven to be superior.
Indications and Timing
A patient undergoing NAR can have nipple creation and tattooing performed simultaneously or as two separate procedures. Many patients and plastic surgeons do not consider a breast reconstruction complete until the NAR and tattooing are performed. It is recommended to delay NAR for approximately 3-6 months after breast mound creation in order to achieve stable breast volume, overlying skin and contour.
Contraindications
Nearly all patients, with the exception of those with active or progressive malignancy, should be offered NAR. As with all forms of postablative reconstruction, the first and foremost goal is adequate treatment of the specific malignancy, and this goal should never be compromised. Some consider radiation a relative contraindication due to its detrimental effects on wound healing. However, in patients with minimal breast skin changes, NAR may be performed with satisfactory results at approximately 6-8 wks following the completion of radiation treatment. Much of nipple projection is based on underlying subcutaneous fatty tissue; therefore patients who have undergone tissue expander reconstruction with thinning of this layer will need to be educated on realistic goals regarding nipple projection.
Practical Plastic Surgery, edited by Zol B. Kryger and Mark Sisco. ©2007 Landes Bioscience.

284 |
Practical Plastic Surgery |
Anatomy
In unilateral breast reconstruction, the contralateral breast determines placement of the NAC and represents a comparison for normal anatomy. In bilateral breast reconstruction, the surgeon must rely more on measurements based on anatomical landmarks, namely the midpoint of the sternum, sternal notch, midclavicular line and inframammary fold. The distance from both the sternal notch and midclavicular line to the mid-nipple position should each measure approximately 19 to 21 cm. The distance from the midpoint of the sternum to the mid-nipple position should measure 9 to 11 cm. The inframammary fold lies 7 to 8 cm from the mid-nipple position, or 6 cm from the inferior areolar border. If discrepancies arise, it is best to remember that the NAC is the primary focus of the breast mound and aesthetically should be centered at the point of maximal projection. Other equally important anatomic considerations include the color, texture and size of the areola. The average nipple diameter is 8 mm, while the average areolar diameter
45is 42 to 45 mm. The areola is darker in color than the surrounding breast mound skin and is further affected by race and parity. Projecting a millimeter or so above the breast mound, the areola hosts several Montgomery glands contributing to its rough texture. Nipple projection is one of the most important considerations and is often overcompensated at the time of NAR in anticipation of loss of projection over time. When unstimulated, the nipple normally projects approximately 4 to 6 mm above the areola.
Preoperative Considerations
There are a vast number of operative techniques available for creation of the NAC. The method selected depends on the anatomic characteristics and projection of the contralateral nipple. Both the patient’s desires and surgeon’s preferred technique must be considered.
The patient should be marked in an upright position as the NAC may shift when supine. Furthermore, to avoid unwanted superior placement of the NAC, the patient’s shoulders should be completely relaxed. Positioning should be determined based on previously described normal breast dimensions or the contralateral breast in unilateral breast reconstruction. Nipple-areolar positioning becomes difficult when there is a discrepancy between the normal anatomic measurements and the actual appearance of the NAC, typically as a result of asymmetric breast mounds. Preoperative antibiotics are typically not necessary, especially if the patient lacks an underlying implant. This procedure may be performed in an office under local anesthesia. Conversely, the procedure can be carried out in the operating room under conscious sedation or monitored anesthesia care if accomplished simultaneously with port removal or final touch-up procedures of previous autologous breast reconstructions.
Operative Technique
Approximately 100 different techniques and modifications of NAR have been described in the literature; however no single procedure can create the optimal NAC in one stage. Local flap techniques are the most popular since fears of donor site morbidity have largely been alleviated through modifications in previous flap designs allowing for direct donor site closure without the need for skin grafting. The most popular techniques are described in this chapter.

Nipple Reconstruction and Tattooing |
285 |
The Skate Flap |
|
The Skate flap has proved to be reliable but is one of the techniques which may |
|
require skin grafting to cover the donor sites. A small circle (the base) measuring the |
|
exact size of the proposed new nipple is drawn at the appropriate position on the |
|
breast mound. The wings, elevated as partial-thickness skin flaps, depend on intra- |
|
dermal blood flow and a well-vascularized subcutaneous pedicle at the base or the |
|
proposed new nipple. They are elevated at the level of the deep dermis from the |
|
periphery inward until the width of the base is reached. The base is then used to line |
|
the flap vertically. This linear portion is elevated full-thickness including underlying |
|
deep fat. The wings are wrapped around this central portion to create the nipple. |
|
The areola is created by skin grafting the donor sites and the remaining circular |
|
de-epithelialized tissue, allowing the nipple to protrude through a circular hole in |
|
the center of the graft. Skin graft donor sites include the contralateral areola, labia, |
|
upper inner thigh or lateral mastectomy dog ear. |
|
The Modified Star Flap |
45 |
|
The modified star technique is similar to the skate flap except skin grafting is not required, and the lateral flaps or wings are raised full-thickness instead of just elevating the dermis. Primary donor site closure, increased blood supply and improved nipple projection are some of the significant advantages offered by the modified technique. The base may be positioned superiorly, laterally or inferiorly and measures approximately 1 to 1.5 cm in diameter, or the desired width of the nipple. Resulting nipple projection is directly related to the width and length of the laterally diverging flaps. The flaps should measure 1.5 times the desired height to account for loss in projection with time. The limbs are typically 1.5 to 2.0 cm in length. The longer the skin flaps the greater the projection. As previously mentioned, the lateral limbs and apex flap are elevated full-thickness, including the underlying fat; 5-0 plain or chromic gut sutures are used to secure the limbs after they are rotated and interdigitated. The donor sites are undermined slightly and closed primarily.
The S-Flap
The S-flap for nipple reconstruction uses an S-shape design to create two equal skin flaps with opposing bases. The center of the S represents the desired location of the new nipple. If a preexisting mastectomy scar exists, then the central limb of the S should be drawn along the scar to secure blood supply. Nipple projection is determined by the length of the flaps, which are raised full-thickness and sutured to each other. Circular de-epithelialization and subsequent placement of a skin graft for areolar reconstruction have been described in conjunction with the S-flap.
The Modified Double Opposing Tab Flap
The double opposing tab flap allows direct closure of the donor site without skin grafting. The tabs are raised as full-thickness skin flaps and the original back cuts first described have been eliminated to improve blood supply to the flap. Two equal semicircular flaps with opposing bases are drawn extending from a shared line measuring approximately three times the desired height of the final nipple. A round nipple projection of approximately 10-12 mm is accomplished after opposing the 18 mm wide flaps; 4-0 and 5-0 chromic sutures are used to primarily close both the donor and skin sites. This technique is similar to the S-flap and also allows incorporation of the mastectomy scar without compromising skin flap viability. This method may be used for nipple reconstructions requiring a larger broad-based nipple.

286 |
Practical Plastic Surgery |
The C-V Flap
The C-V flap produces an excellent reconstruction, but it is dependent upon the underlying subcutaneous fat to provide the bulk of the reconstructed nipple. In most cases, the subcutaneous tissue is adequate. However, in cases of tissue expansion, the fat may be insufficient to produce a nipple of adequate bulk. This design uses two V flaps and a C flap to create the nipple. The widths of the V flaps determine projection, whereas the diameter of the C flap determines the diameter of the new nipple. This flap is quite similar in design to the modified star flap.
The Bell Flap
This bell-shaped flap design incorporates a unique purse string suture allowing for a tension free closure of the donor site. A circle, representing the final positioning of the new NAC, is drawn slightly larger than the contralateral areola, or approximately 45-50 mm in bilateral reconstructions. Next, the superiorly-based bell
45flap is elevated full-thickness toward the handle of the bell design and the entire circumference of the circle is incised in the subcutaneous plane. The defect created by flap elevation may be approximated after folding the flap on itself and securing the two sides of the bell around the handle. To produce final NAC projection, a subdermal nylon suture is placed around the circumference of the circle in a purse string fashion.
Tattooing
Tattooing is an optical effect used to color the areola and nipple approximately 6-8 weeks after nipple reconstruction is complete. It has several advantages, namely it is simple, reliable, easily correctable and has no effect on eventual nipple projection. Precise color matching to the contralateral NAC can be readily performed due to the many different pigments available. Intradermal pigmentation is generally performed with iron oxide and titanium dioxide pigments. The patient is encouraged to choose a pigment that is slightly darker than her normal areolar color, as the color often fades, requiring one or more touch up applications.
Postoperative Care
Following NAR, antibiotic ointment is applied to the nipple, and it is covered with sterile dressings for 48 hours. A small hole for the nipple can be cut in a few 4 x 4 gauze pads to avoid compression of the new nipple. In addition, steri-strips® can be used along the donor site regions at the base of the nipple. After 48 hours, patients may shower avoiding direct pressure to the nipple. They should be advised to wear loose-fitting, noncompressible bras for at least 2 weeks. Healing normally occurs in approximately 1 to 2 weeks. Following tattooing, impregnated-gauze dressings are applied and the patient is instructed to avoid direct water pressure to the area for 2 days.
Complications
Nipple necrosis is one of the feared and most serious complications of NAR, which can result in wound separation. Flap dehiscence with unfolding of the nipple may also occur. Smokers must be encouraged to quit smoking, at least temporarily, in order to avoid compromising the blood supply and healing of tissues. One of the more common undesirable outcomes of NAR is loss of nipple projection, occurring most significantly in the first 6 months. It is safe to assume that approximately 60%

Nipple Reconstruction and Tattooing |
287 |
of the projection achieved at surgery will be reliably maintained at one year follow up. Incorporating subcutaneous tissue allows for volume and projection, however fat is absorbed over time, thus causing flap flattening. Complications of tattooing can include infection, rash, slough and discoloration. Some patients may require retattooing for fading of pigment, poor take of pigment or revision of the shape of the pigmented area.
Pearls and Pitfalls
•Not all patients desire NAR. It should be presented as an option and not a necessity. The patient can always change her mind at a later time.
•When dressing the newly created nipple, a hole can be cut in the center of two gauze eye-patches. The patches surround the nipple and provide support and protection.
•In unilateral cases, the newly created nipple should match the contralateral side
in terms of diameter only. Its height should be at least 1.5 times greater than the |
45 |
other side. |
•In patients with extremely large, projecting nipples, always consider nipple reduction (e.g., wedge excision) of the normal side, and offer this to the patient. If she chooses to keep her normal nipple intact, the Skate flap is a good option for very projecting nipples.
•Beware of the donor site closed with excessive tension. A spread scar will not be easily concealed by tattooing, as the scarred dermis does not incorporate the pigment very well.
Suggested Readings
1.Cronin ED, Humphreys DH et al. Nipple reconstruction: The S flap. Plast Reconstr Surg 1988; 81(5):783.
2.Eng JS. Bell flap nipple reconstruction—a new wrinkle. Ann Plast Surg 1996; 36(5):485.
3.Eskenazi L. A one-stage nipple reconstruction with the “modified star” flap and immediate tattoo: A review of 100 cases. Plast Reconstr Surg 1993; 92(4):671.
4.Few JW, Marcus JR et al. Long-term predictable nipple projection following reconstruction. Plast Reconstr Surg 1999; 104(5):1321.
5.Hartrampf Jr CR, Culbertson JH. A dermal-fat flap for nipple reconstruction. Plast Reconstr Surg 1984; 73(6):982.
6.Kroll SS, Hamilton S. Nipple reconstruction with the double-opposing-tab flap. Plast Reconstr Surg 1989; 84(3):520.
7.Spear SL, Convit R et al. Intradermal tattoo as an adjunct to nipple-areola reconstruction. Plast Reconstr Surg 1989; 83(5):907.
8.Wellisch DK, Schain WS et al. The psychological contribution of nipple addition in breast reconstruction. Plast Reconstr Surg 1987; 80(5):699.
Chapter 46
Reduction Mammaplasty
Timothy W. King and Jamie P. Levine
Introduction
The goal of breast reduction is to reduce the overall volume of the breast while maintaining an aesthetically pleasing shape and the viability of the nipple areola complex. When considering the different techniques of breast reduction, it is important to understand that the two components of the surgery—the skin incisions and the pedicle—are independent of each other. Thus, you can have any type of skin incision with any type of pedicle (Table 46.1). This being said, there are commonly used approaches to breast reduction, and this chapter will focus on these combinations, namely the Wise pattern/inferior pedicle, the vertical scar/medial pedicle and the free nipple graft. The surgeon, however, should not be as limited in his thinking and should be open minded when selecting the best combination for each individual patient.
Preoperative Considerations
Indications for reduction mammaplasty are symptoms secondary to the large breast volume. These symptoms include chronic back, shoulder and neck pain, headaches, upper extremity neuropathy, postural changes, bra strap grooves in the shoulders and dermatological disorders in the inframammary folds.
In addition to the standard discussion of risks, benefits and alternatives of the procedure, the patient should know that there may be some loss of sensation, change in color, or even death/necrosis of the nipple-areola complex. Patients should also be warned that since some of the breast parenchyma is being removed, the ability to breastfeed might be altered with a breast reduction (although several studies show no significant differences in breast-feeding between women who have and haven’t undergone breast reduction). The patient should be shown where and how long the scars will be on her breasts. She should realize that although everything will be done to avoid it, there will likely be some asymmetry between the breasts. A complete history and physical exam should be performed, particularly focusing on any history of breast disease. If age appropriate, the patient should have a screening mammogram within the past year.
Marking the Patient
Patient marking is a critical step in the planning of any breast reduction. The patient should be marked in the preoperative holding area with a thick felt tip marking pen. The patient should be sitting or standing upright facing forward, with her arms at her sides. The lateral border, medial border, midline and inframammary fold are marked. Once in the operating room, key midline and angle markings can be reinforced by remarking, tattooing, suturing, stapling, or lightly scratching the marks with an 18-gauge needle.
Practical Plastic Surgery, edited by Zol B. Kryger and Mark Sisco. ©2007 Landes Bioscience.
Reduction Mammaplasty |
289 |
|
|
|
|
Table 46.1. The commonly used pedicles, their indications and the various skin incisions available for breast reduction
Type of Pedicle |
Indications for Its Use |
Types of Skin Incisions |
Inferior pedicle |
Good for almost any breast |
Wise pattern/inverted T |
|
size and shape |
|
Superior pedicle |
Best for small to moderate |
Vertical |
|
breast reductions |
|
Medial pedicle |
Reductions less than 1500 |
Lateral |
|
grams per side |
|
Partial breast |
Massive reductions (>40 cm |
Circumareolar |
amputation |
from sternal notch to nipple) |
|
Liposuction |
Minimal reduction, |
None |
|
little to no ptosis |
|
Note that any skin incision can be used with any type of pedicle.
46
Wise Pattern/Inferior Pedicle
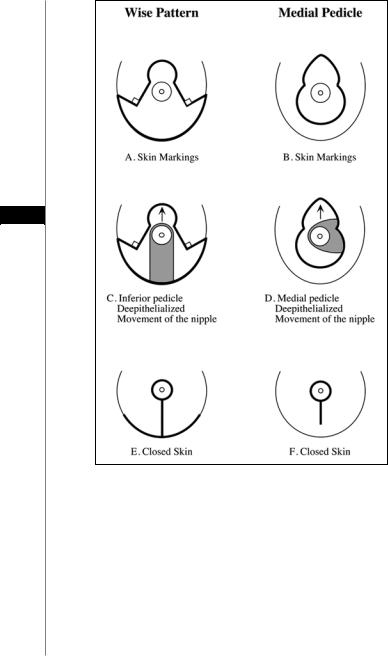
A tape measure is required for marking, and a wire keyhole pattern of 14-15 cm long can be helpful to match a 42 mm cookie cutter. The sternal notch and midclavicular points are marked. The midclavicular point, for reasons of standardization and symmetry is normally set at 6 or 7 cm from the sternal notch. A meridian line from the midclavicular point through the nipple-areolar complex is made and then transposed to the inframammary fold and marked. The inframammary fold is marked and is translated to the anterior surface of the breast at the intersection of the meridian line. The new nipple position should be 0.5-1 cm above the anatomic inframammary fold in the meridian line. The wire keyhole is placed on the breast and adjusted for the individual patient. If the breasts are large and tense, the keyhole should be made narrower to reduce the amount of skin removed. On the other hand, if the breasts are lax and ptotic, the keyhole should be widened to allow more skin excision. Two lines are drawn from the end of the keyhole circle angling away from the meridian of the breast. The angle selected determines the amount of skin excised. The height of the vertical limbs should be 5-6 cm from the bottom of the keyhole circle. The keyhole pattern is then traced onto the skin. At the base of the vertical keyhole limbs a line creating a 90° angle is drawn and extended to the line marking the inframammary fold to complete the horizontal limb (Fig. 46.1). These horizontal lines define the future inframammary fold. These points can end in the breast folds. Some surgeons use a template for the entire markings and some complete the keyhole/areolar markings in the operating room.
Vertical Scar/Medial Pedicle
As with the Wise pattern, the meridian line is established and drawn. With this technique, the new nipple should be placed 2 cm lower than in the Wise technique. This will place the new nipple at or just below the level of the existing inframammary fold. A mosque-shaped areolar pattern is used and is marked on the skin (Fig. 46.1). Lines similar to the vertical limbs of the Wise pattern are drawn. These lines can be drawn in an individualized fashion by using the breast displacement method. The breast is moved medially and a straight line is drawn reapproximating the meridian. When the breast is returned to its normal resting position, a curved line remains as
290 |
Practical Plastic Surgery |
46
Figure 46.1. Comparison of the Wise pattern/inferior pedicle (A,C,E) with the vertical scar/medial pedicle (B,D,F). Illustrated from top to bottom are the initial skin markings (A,B), the de-epithelialized pedicle with the intact nipple-areola complex (C,D) and the final scars shown in bold (E,F).
the lateral extent of excision. This process can be repeated for the medial limb by lateral displacement of the breast. However, at the point where one makes a 90˚ angle, the line continues inferiorly and curves at the base, making a “U” shape. The distance from the inferior edge of the “U” to the inframammary fold should be 2-6 cm dependent upon the amount of ptosis of the breast. If the base of the “U” is too close to the inframammary fold, the vertical scar will extend down onto the chest/ abdominal wall when the incision is closed since this technique can raise the inframammary fold position.

Reduction Mammaplasty |
291 |
Free Nipple Graft
As with the Wise pattern, the sternal notch, midclavicular points and the meridian line are determined and drawn. The markings for this procedure are similar to the Wise pattern. However, in this case there will not be a pedicle carrying the nipple/areola complex. The nipple/areola complex will be removed as a free, full-thickness graft and replanted onto the breast at its new location. The apex of the areola is marked and the vertical limbs are drawn in a similar fashion to the Wise pattern. The inframammary fold is marked and is translated to the anterior surface of the breast at the intersection of the meridian line. The height of the vertical limbs should be 5-6 cm. At the end of the vertical limbs, a line creating a 90˚ angle is drawn and extended to the line marking the inframammary fold, completing the horizontal limb (Fig. 46.1). These horizontal lines define the future inframammary fold. These markings should be placed while supporting the weight of the breast or the nipple-areola will end up too high on the final reduced breast.
Intraoperative Considerations
46
Wise Pattern/Inferior Pedicle
The inferior pedicle is marked vertically below the nipple-areolar complex and should be 8-9 cm wide at the base centered on a line from the nipple to the inframammary fold. This base can be widened with longer pedicles. The superior portion should extend in a curvilinear fashion 1 cm around the nipple-areolar complex. With the breast under moderate tension, a 38 or 42 mm cookie cutter is centered over the nipple and used to mark the areola for reduction. This should match with the keyhole pattern chosen. An incision is then made along this mark to the level of the dermis. Another incision is made along the marks for the inferior pedicle and the skin over the pedicle is deepithelialized (Fig. 46.1).
The breast tissue is resected in a systematic fashion. Tissue will be removed from the medial, lateral and superior aspects of the breast. Starting with the medial aspect of the pedicle, the breast tissue is dissected just superficial to the pectoralis fascia. Beveling the dissection away from the pedicle will aid in preserving the vascularity of the pedicle. A good base should remain attached to the chest wall. A skin incision is made along the lines previously marked in the inframammary fold and the medial aspect of the breast. The breast parenchyma is dissected down to the same level as performed previously. Once all the dissection has occurred, a small medial wedge of breast tissue is excised and weighed.
In a similar fashion the lateral breast tissue is excised. In general, more tissue is removed from the lateral aspect of the breast than the medial aspect since medial fullness is aesthetically more desirable. Attention is then turned to the superior aspect of the breast. The skin of the vertical limbs of the keyhole pattern is incised. Some surgeons will not incise the curvilinear pattern (or center) initially. Rather, they recommend extending the vertical limbs to form a triangle at the apex of the keyhole. This allows the surgeon to sit the patient up and determine the exact location of the nipple-areolar complex prior to committing to a specific location. A superior flap approximately 2 cm thick is created and dissected to the level of the pectoralis fascia. The remaining superior breast tissue is then removed from the breast. This creates the pocket allowing the pedicle to be placed in the more superior position. All tissue is weighed together from each breast and sent to pathology for evaluation.
