
Practical Plastic Surgery
.pdf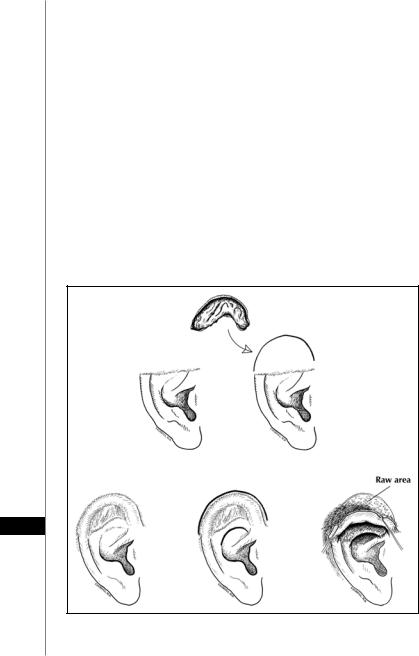
172 |
Practical Plastic Surgery |
This flap is based anterosuperiorly in the auriculocephalic sulcus. In the first stage, a cartilage graft is procured, carved and placed in the area of missing cartilage in the upper-third of the ear. The flap is then raised and inset over the cartilage at the edges of the defect. Presence of cartilage for support ensures long-term stability. A split-thickness skin graft covers the donor site defect. In the second (and final) stage several weeks later, the base of the flap is divided leaving sufficient nonhairy skin to reconstruct the ascending helix. The remainder of the hair-bearing flap is sutured to the scalp to reestablish the hairline.
Contralateral Conchal Cartilage Graft Procedures (Adams and Brent)
Application: Upper-third (Adams) and lower-third (Brent) defects of the ear Defect size: Large
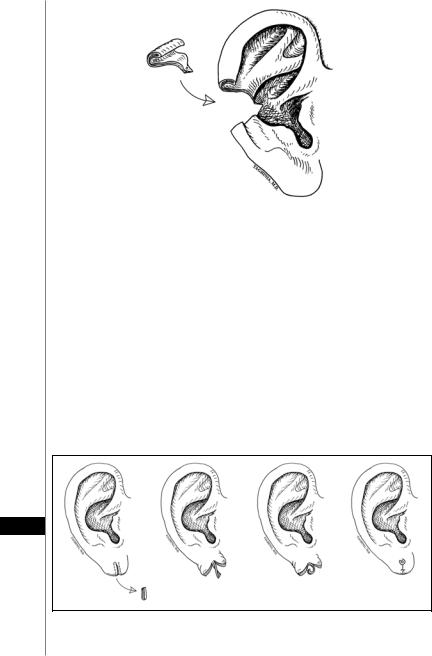
Illustration: Figures 30.6 (upper-third, Adams), 30.7 (lower-third, Brent) Initially described for upper-third defects, this method was then used by Brent
for reconstruction of lower-third losses. The success of these procedures relies on supple, intact temporal and mastoid skin. Initially, a conchal cartilage graft is removed from the other ear using an anterolateral or posterior approach. For reconstruction of the upper-third, the cartilage graft is implanted under mastoid skin in the upper ear and anchored to the remnant of the helical root. Anchoring of the
30
Figure 30.6. Contralateral conchal cartilage graft procedure for upper-third deformities (Adams flap).
Ear Reconstruction |
173 |
|
|
|
|
|
|
|
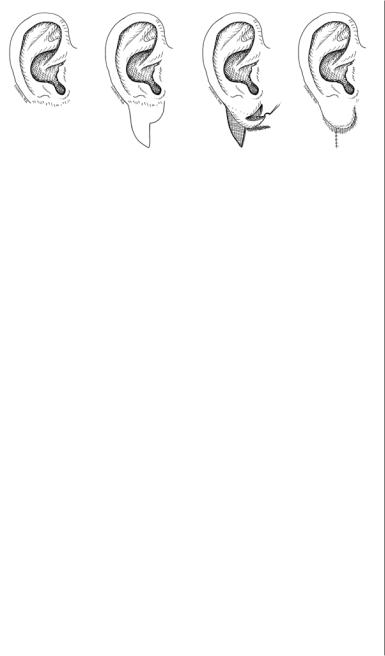
Figure 30.7. Contralateral conchal cartilage graft procedure for lower-third deformities described by Brent. A bipedicle flap is outlined in a second stage, and a ‘valise handle’ is raised. The raw surface underneath is skin grafted.
cartilage graft ensures stability and long-term helical continuity. At a second stage, an incision is made in the hair margin and the upper ear is undermined, lifted, and the raw area is skin grafted. Brent (1977) prefers to make another incision in the proposed posterior conchal wall and inferior crus so the entire upper ear bipedicled flap can be lifted as a ‘valise handle’. This maneuver elevates and defines the inferior crus and gives depth to the superior concha.
A similar approach is used for large defects of the lower third of the ear (Brent). Creation of a bipedicle flap, lifted as a ‘valise handle’ gives definition to the posterior conchal wall. A tube skin flap can be used for reconstruction of the lower helix and earlobe.
Conchal Chondrocutaneous Transposition Flap (Davis)
Application: Upper-third defects of the ear Defect size: Large
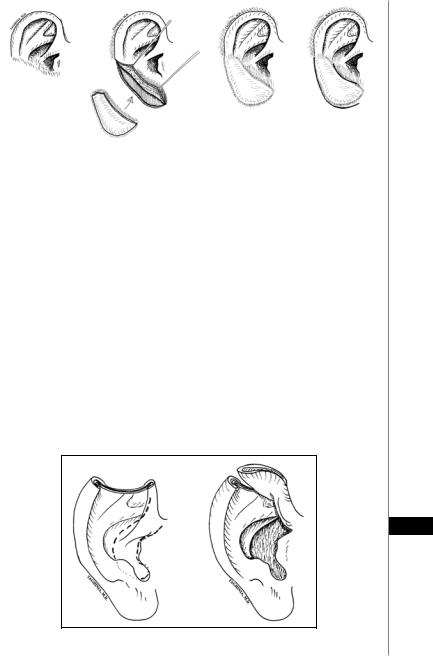
Illustration: Figure 30.8.
If the mastoid skin is unfavorable for flap reconstruction, a conchal transposition flap may be used for large defects of the upper ear. This flap is technically
30
Figure 30.8. Conchal transposition flap (Davis technique).
174 |
Practical Plastic Surgery |
difficult but ideal for burns because the upper ear and mastoid skin are frequently destroyed, but the central ear is spared. The entire concha (composite flap of cartilage and skin) is rotated upward on a small anterior pedicle of the crus helicis. Irregularities in contour are tailored and the lower part of the flap is inset into the defect. The conchal donor bed and the newly created rim are skin grafted.
Tunnel Procedure (Converse)
Application: Upperand middle-third of the ear Defect size: Moderate to large
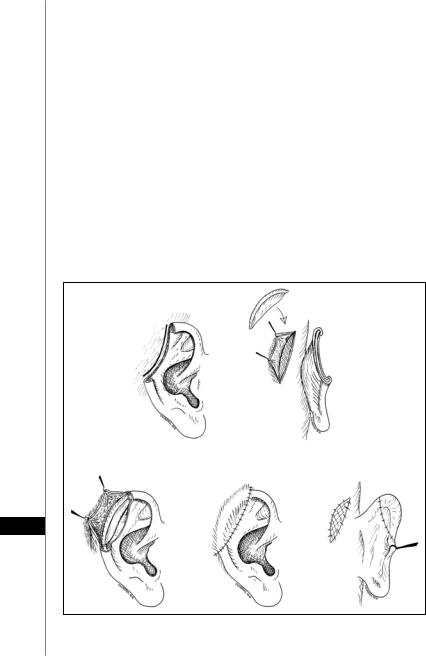
Illustrations: Figure 30.9.
Converse’s techniques for upperand middle-third reconstructions are similar. Interestingly, most textbooks incorrectly refer to Converse’s middle-third reconstructive method as the ‘tunnel’ procedure, presumably because a subcutaneous tunnel (for a cartilage graft) is created between the two edges of the middle-third defect. In fact, Converse called his technique for upper-third reconstruction the ‘tunnel’ procedure. A tunnel is created in the superior auricular sulcus as the upper ear is apposed to the edge of the mastoid skin pocket (see below). This tunnel is lined by native skin epithelium and ultimately gets opened at the second stage operation. It needs frequent cleansing by the patient to prevent infection. For simplicity, we will refer to both of these procedures as the ‘tunnel’ procedures.
30
Figure 30.9. Tunnel procedure (Converse flap) for upper-third losses.
Ear Reconstruction |
175 |
When applied for upper-third defects (Fig. 30.9), Converse’s method has the advantage of preserving the superior auricular sulcus. The ear is pressed against the scalp, and incisions are planned and made along the edge of the ear defect and the mastoid skin. A mastoid skin flap is then raised posterosuperiorly. The medial edge of the ear incision is sutured to the anterior edge of the mastoid skin incision, thus creating a pocket where a carved costal cartilage graft can be placed and secured. The mastoid skin flap is then advanced to cover the cartilage graft. In a second stage, the ear is separated from the mastoid area and the raw areas (on the back of the ear and the mastoid donor site) are skin grafted.
For middle-third defects, a pocket is created in the mastoid skin flanking the edges of the defect and a cartilage graft is placed in the pocket. The edges of this pocket are approximated to the edges of the defect. A few weeks later, an incision posterior to the cartilage graft is made and the retroauricular sulcus is created. The raw areas on the mastoid and posterior ear are skin grafted. For large defects, tissue expansion may be needed to get additional nonhairy, thin skin.
Retroauricular Flap with Cartilage Graft (Dieffenbach)
Application: Middle-third defects of the ear Defect size: Moderate to large
Illustration: Figure 30.10.
Similar to the Converse tunnel procedure, this method relies on a skin flap and a cartilage graft. The defect is drawn out and a posterior skin flap is planned in the mastoid skin. The flap is raised and a cartilage graft is placed and covered by the flap. At a second stage, the base of the flap is divided and the flap is folded around the cartilage graft. A skin graft then covers the mastoid donor site.
Chondrocutaneous Composite Graft
Application: Upperand middle-third defects of the ear Defect size: Small to moderate
Illustration: Figure 30.11.
Composite grafts from the contralateral ear may be used for reconstruction of small to moderate defects. A wedge-shaped graft of 1.5 cm width can be harvested from the helix/scapha of the unaffected ear. The success of these grafts is enhanced by converting part of the composite graft to a full-thickness skin graft (i.e., by excising some skin and cartilage). In this manner, more of the skin component is in direct contact with a vascular bed, thereby improving plasmatic imbibition. These grafts have a tendency to shrink in the long-term.
30
Figure 30.10. Retroauricular flap (Dieffenbach procedure).
176 |
Practical Plastic Surgery |
|
|
|
|
|
|
|
Figure 30.11. Contralateral composite graft for middle-third reconstruction. This method can also be applied to small to moderate defects of the upper-third. Brent recommends increasing chance of graft ‘take’ by creating more raw surface contact.
Earlobe Reconstruction
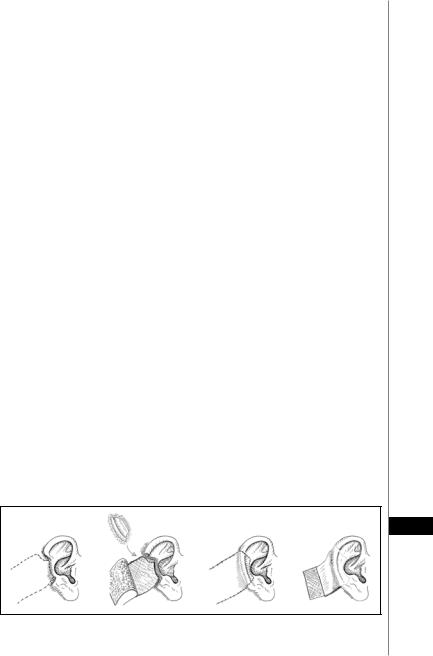
Application: Earlobe defects Defect size: Small to large Illustration: Figures 30.12, 30.13
The most common acquired earlobe deformities are keloids and traumatic clefts. Keloids are treated with steroid therapy and pressure-spring earrings. Radiation can sometimes be effective for recurrent or recalcitrant keloids. When a keloid is excised, the skin overlying the keloid can be harvested as a split-thickness skin graft and used to cover the remaining defect.
Earlobe clefts can be repaired using a variety of methods. Straight-line excision and closure of these defects is not recommended because the scar contracts upwards, creating a notch in the inferior contour. Most surgeons prefer to repair these clefts
30
Figure 30.12. Earlobe cleft reconstruction (Pardue technique). A clever method using a rolled-up skin flap to allow continued wearing of earrings.
Ear Reconstruction |
177 |
|
|
|
|
|
|
|
Figure 30.13. Earlobe reconstruction (Alanis technique).
by elongating the incision using Z-plasties. Pardue suggested a clever method whereby patients can continue wearing earrings (Fig. 30.12). Multiple methods have been devised to reconstruct missing earlobes. Most of these methods use mastoid skin flaps that roll or fold to create an earlobe (Fig. 30.13). These earlobe constructs are prone to shrinking, especially if the blood supply is tenuous.
Pearls and Pitfalls
Cartilage is the key aesthetic element of the ear; it creates the hills and valleys that make an ear look like an ear. During ear reconstruction, replacing missing cartilage is important for construct stability and aesthetic contour. Without cartilaginous support, skin and soft tissue constructs do not uphold in the long term.
Recreation of the helix is one of the more important tasks in aesthetic ear reconstruction. Our brain is trained to visualize a ‘normal’ ear as one with a smooth, uninterrupted outer contour. Any slight deviation from this outline is strikingly obvious. Symmetry is less important in ear reconstruction because both ears are rarely seen at the same time. As long as the ears look normal, great discrepancies in ear size can go unnoticed.
Suggested Reading
1.Alanis SZ. A new method for earlobe reconstruction. Plast Reconstr Surg 1970; 45(3):254.
2.Antia NH, Buch VI. Chondrocutaneous advancement flap for the marginal defect of the ear. Plast Reconstr Surg 1967; 39(5):472.
3.Adams WM. Construction of upper half of the auricle utilizing composite concha cartilage graft with perichondrium attached on both sides. Plast Reconstr Surg 1955;
|
16(2):88. |
30 |
4. |
Brent B. The acquired auricular deformity. Plast Reconstr Surg 1977; 59(4):475. |
|
5. |
Brent B. Reconstruction of the auricle. In: McCarthy JG, ed. Plastic Surgery. New |
|
|
York, NY: WB Saunders Co., 1990:2094. |
|
6. |
Crikelair GF. A method of partial ear reconstruction for avulsion of the upper portion |
|
|
of the ear. Plast Reconstr Surg 1956; 17(6):438. |
|
7. |
Converse JM. Reconstruction of the auricle, Part I. Plast Reconstr Surg 1958; 22(2):150. |
|
8. |
Donelan MB. Conchal transposition flap for postburn ear deformities. Plast Reconstr |
|
|
Surg 1989; 83(4):641. |
|
9. |
Dujon DG, Bowditch M. The thin tube pedicle: A valuable technique in auricular |
|
|
reconstruction after trauma. Br J Plast Surg 1995; 48(1):35. |
|
Chapter 31
Eyelid Reconstruction
Amir H. Taghinia and Bernard T. Lee
Introduction
Surgical excision of eyelid tumors often produces large defects that can cause significant visual impairment and cosmetic stigma if not treated properly. Reconstruction requires thorough knowledge of anatomy and precise technical execution. Although there are many reconstructive options in the form of flaps and grafts, the basic principles are: 1) replace lining, support and skin cover; 2) restore corneal protection and lubrication; and 3) optimize the aesthetic outcome. This chapter briefly summarizes eyelid reconstruction while providing a useful, quick-reference algorithm (Table 31.1).
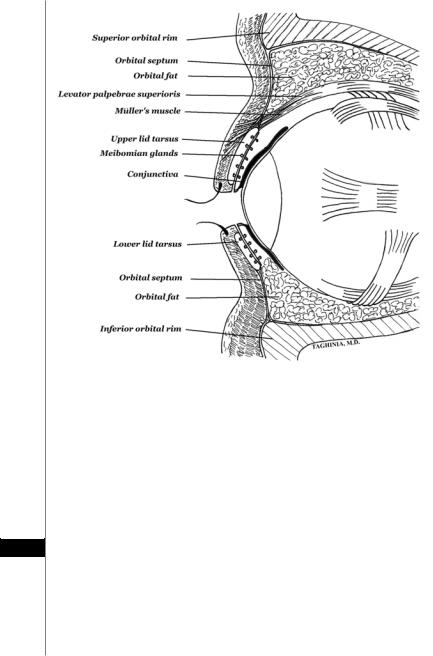
Relevant Anatomy
The cross-sectional anatomy of the upper and lower eyelids is shown in Figure 31.1. The eyelids consist of skin, orbicularis muscle, tarsal plate and conjunctiva. The upper lid also contains slips of the upper eyelid retractors (see below). The orbicularis oculi muscle consists of three separate divisions: pretarsal, preseptal and orbital. The pretarsal orbicularis is primarily responsible for involuntary blinking. The preseptal orbicularis pumps tear through the lacrimal system and aids in voluntary lid closure. The orbital orbicularis depresses the medial brow and performs protective forced eyelid closure.
Eyelid layers have been arbitrarily divided into the anterior and posterior lamellae. The anterior lamella contains the skin and orbicularis oculi muscle while the posterior lamella contains the tarsus, eyelid retractors and conjunctiva.
The tarsal plates contain vertically oriented Meibomian glands that exit on the lid margin. These glands secrete oils that mix with tears to provide lubrication for the conjunctiva. Medially and laterally, the tarsal plates narrow into fibrous bundles that ultimately converge to form the medial and lateral canthal tendons. The medial aspects of the upper and lower lids host the upper and lower punctae, respectively. Tears generated from the lacrimal gland drain via the punctae into the lacrimal canaliculi and ultimately into the lacrimal sac. The lacrimal sac empties into the inferior meatus via the nasolacrimal duct. Blinking enhances tear drainage by squeezing the lacrimal sac and forcing tears down the nasolacrimal duct.
Upper eyelid positioning is achieved through the action of the levator palpebrae superioris and Müller’s muscles (the upper eyelid retractors). The levator muscle originates from the orbital cone and is innervated by the oculomotor nerve (CN III). As it approaches the upper lid, it broadens into the levator aponeurosis and becomes closely approximated with Müller’s muscle before attaching to the upper tarsal plate. Müller’s muscle is controlled by sympathetic nervous fibers.
Practical Plastic Surgery, edited by Zol B. Kryger and Mark Sisco. ©2007 Landes Bioscience.
Eyelid Reconstruction |
179 |
 Table 31.1. A basic algorithmic approach to eyelid reconstruction
Table 31.1. A basic algorithmic approach to eyelid reconstruction
>2/3 |
FTSGorlocalflap |
Uppereyelidtarsoconjunctivalflap |
(modifiedHughes)coveredbylocal |
flaporFTSG |
Chondromucosalgraftcoveredby |
localflaporcheekadvancement |
flap(Mustarde) |
|
FTSG |
Lowereyelidbridgingfull-thickness |
flap(Cutler-Beard) |
Lowereyelidswitchflap |
(Mustarde) |
|
DefectSize 1/3to2/3 |
FTSGorlocalflap |
Lateralcanthotomyandcantholysiswith |
primaryclosure |
|
Semicircular(Tenzel)flapwith |
primaryclosure |
|
LateraladvancementwithZ-plasty (McGregor)andprimaryclosure |
FTSG |
Lateralcanthotomyandcantholysiswith |
primaryclosure |
Semicircularflap(Tenzel)with |
primaryclosure |
LateraladvancementwithZ-plasty (McGregor)andprimaryclosure Slidinguppereyelidtarsoconjunctival flap(modifiedHughes)coveredby localflaporFTSG |
Upto1/3 |
PrimaryClosure |
PrimaryClosure |
|
|
|
|
|
|
PrimaryClosure |
PrimaryClosure |
|
|
|
|
|
PartialThickness |
FullThickness |
|
|
|
|
|
|
PartialThickness |
FullThickness |
|
|
|
|
|
LowerEyelid |
|
|
|
|
|
|
|
UpperEyelid |
|
|
|
|
|
31
180 |
Practical Plastic Surgery |
|
|
|
|
|
|
|
Figure 31.1. Cross-sectional anatomy of the upper and lower eyelids. Note that the levator palpebrae superioris and Müller’s muscle are intimately associated. Müller’s muscle attaches to the tarsal plate. The levator gives rise to distal fibers termed the levator aponeurosis. These fibers insert on the tarsal plate and the pretarsal orbicularis.
These fibers synapse in the superior cervical ganglion and intertwine as they ascend along the internal carotid artery into the cranium.
Eyelid Lesions
The skin and glands of the eyelids are susceptible to development of benign and malignant neoplasms. There is a higher preponderance of eyelid tumors in the lower
31eyelids (90% vs. 10% in upper eyelids). The most common malignant eyelid tumor is basal cell carcinoma. Squamous cell carcinoma of the eyelid is rare. Basal cell carcinoma has a high recurrence rate after excision and should be treated aggressively. Malignant melanoma in situ (lentigo maligna), though rare, also warrants wide excision; 5 mm margin is recommended. Eyelid reconstruction after surgical excision of tumors should be delayed until final pathological diagnosis and evaluation of margins is completed. The surgeon treats the open wound with dressings during this time.
Eyelid Reconstruction |
181 |
Lower Eyelid Reconstruction
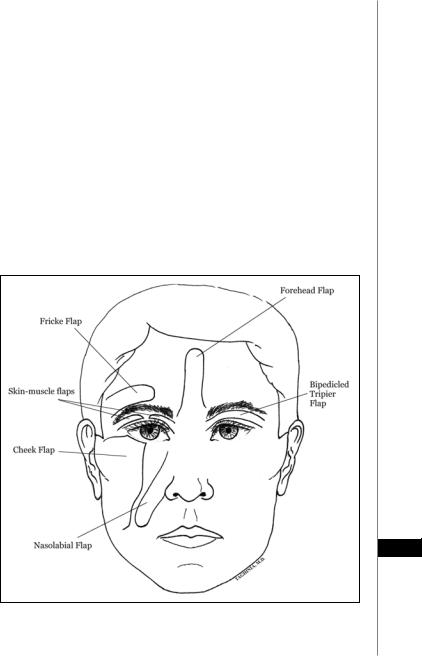
Partial-thickness defects of the lower eyelid may involve just skin or a combination of skin and orbicularis muscle. The reconstructive options for these defects include primary closure, local flap, full-thickness graft and split-thickness graft. Small defects can usually be closed primarily thereby avoiding excessive tension that may lead to ectropion (eversion of the eyelid). Larger defects may require one of a wide variety of local flaps that are available for lower eyelid reconstruction (Fig. 31.2). The bipedicled Tripier flap and medial/lateral skin-muscle flaps rely on ipsilateral upper eyelid tissue that provides excellent color match. The cheek flap also provides a good match in color and quality. The Fricke temporal brow flap, nasolabial flap and midline forehead flap are occasionally useful but provide mediocre color and texture matches.
If local flap coverage of a defect is not possible, the surgeon may use a full-thickness or split-thickness graft. Full-thickness grafts are superior to split-thickness grafts for eyelid reconstruction; they provide little or no contracture with better color and texture match. A full-thickness graft from the upper lid can cover small defects with excellent graft take and minimal donor site scar. For larger defects, skin from both upper eyelids can be used. For defects that involve skin and orbicularis muscle, a composite graft from the upper eyelids usually heals well. Full-thickness grafts may also be harvested from behind the ear and above the clavicle.
31
Figure 31.2. Local facial flaps for eyelid reconstruction. The medial and lateral skin-muscle flaps and the bipedicled Tripier flaps are mainly used for lower eyelid reconstruction.
