
- •Preface
- •Contents
- •Procedures, Assays, and Normal Values
- •Normal Cells of the Blood and Hematopoietic Organs
- •The Individual Cells of Hematopoiesis
- •Bone Marrow: Cell Composition and Principles of Analysis
- •Abnormalities of the White Cell Series
- •Predominance of Mononuclear Round to Oval Cells
- •Prevalence of Polynuclear (Segmented) Cells
- •Erythrocyte and Thrombocyte Abnormalities
- •Hypochromic Anemias
- •Normochromic Anemias
- •Hyperchromic Anemias
- •Erythrocyte Inclusions
- •Thrombocyte Abnormalities
- •Cytology of Organ Biopsies and Exudates
- •Lymph Node Cytology
- •Branchial Cysts and Bronchoalveolar Lavage
- •Cytology of Pleural Effusions and Ascites
- •Cytology of Cerebrospinal Fluid
- •Introduction to the Physiology and Pathophysiology of the Hematopoietic System
- •Cell Systems
- •Principles of Regulation and Dysregulation in the Blood Cell Series and their Diagnostic Implications
- •Procedures, Assays, and Normal Values
- •Taking Blood Samples
- •Erythrocyte Count
- •Hemoglobin and Hematocrit Assay
- •Calculation of Erythrocyte Parameters
- •Red Cell Distribution Width (RDW)
- •Reticulocyte Count
- •Leukocyte Count
- •Thrombocyte Count
- •Significance of the Automated Blood Count
- •Bone Marrow Biopsy
- •Lymph Node Biopsy and Tumor Biopsy
- •Step-by-Step Diagnostic Sequence
- •The Individual Cells of Hematopoiesis
- •Eosinophilic Granulocytes (Eosinophils)
- •Basophilic Granulocytes (Basophils)
- •Monocytes
- •Lymphocytes (and Plasma Cells)
- •Megakaryocytes and Thrombocytes
- •Bone Marrow: Medullary Stroma Cells
- •Abnormalities of the White Cell Series
- •Predominance of Mononuclear Round to Oval Cells
- •Reactive Lymphocytosis
- •Relative Lymphocytosis Associated with Granulocytopenia (Neutropenia) and Agranulocytosis
- •Monocytosis
- •Acute Leukemias
- •Neutrophilia without Left Shift
- •Reactive Left Shift
- •Osteomyelosclerosis
- •Elevated Eosinophil and Basophil Counts
- •Clinically Relevant Classification Principle for Anemias: Mean Erythrocyte Hemoglobin Content (MCH)
- •Hypochromic Anemias
- •Iron Deficiency Anemia
- •Hypochromic Infectious or Toxic Anemia (Secondary Anemia)
- •Hypochromic Anemia with Hemolysis
- •Normochromic Anemias
- •Normochromic Hemolytic Anemias
- •Cytomorphological Anemias with Erythrocyte Anomalies
- •Bone Marrow Aplasia
- •Hyperchromic Anemias
- •Erythrocyte Inclusions
- •Hematological Diagnosis of Malaria
- •Thrombocyte Abnormalities
- •Thrombocytopenia
- •Lymph Node Cytology
- •Sarcoidosis and Tuberculosis
- •Non-Hodgkin Lymphoma
- •Metastases of Solid Tumors in Lymph Nodes or Subcutaneous Tissue
- •Branchial Cysts
- •Cytology of Pleural Effusions and Ascites
- •Cytology of Cerebrospinal Fluid
- •References
- •Index

128 Erythrocyte and Thrombocyte Abnormalities
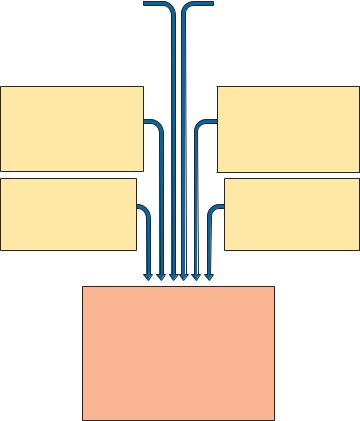
Clinically Relevant Classification Principle for Anemias: Mean Erythrocyte Hemoglobin Content (MCH)
In current diagnostic practice, erythrocyte count and hemoglobin content (grams per 100 ml) in whole blood are determined synchronously. This allows calculation of the hemoglobin content per individual erythrocyte (mean corpuscular hemoglobin, MCH) using the following simple formula (p. 10):
Hb (g/dl) · 10
Ery (106/µl)
The mean cell volume, hematocrit, MCH, and erythrocyte size can be used for various calculations (Table 22; methods p. 10, normal values Table 2, p. 12). Despite this multiplicity of possible measures, however, in routine diagnostic practice the differential diagnosis in cases of low Hb concentration or low erythrocyte counts relies above all on the MCH, and most forms of anemia can safely be classified by reference to the normal data range of 26–32 pg Hb/cell (1.61–1.99 fmol/cell) as normochromic (within the normal range), hypochromic (below the), or hyperchromic (above the norm). The reticulocyte count (p. 11) provides important additional pathophysiological information. Anemias with increased erythrocyte production (hyper-regenerative anemias) suggest a high reticulocyte count, while anemias with diminished erythrocyte production (hyporegenerative anemias) have low reticulocyte counts (Table 22).
It should be noted that hyporegenerative anemias due to iron or vitamin deficiency can rapidly display hyper-regeneration activity after only a short course of treatment with iron or vitamin supplements (up to the desirable “reticulocyte crisis”).
The practical classification of anemia starts with the MCH:
—26–32 pg = normochromic
—Less than 26 pg = hypochromic
—More than 32 pg = hyperchromic
Hypochromic Anemias
Iron Deficiency Anemia
Most anemias are hypochromic. Their usual cause is iron deficiency from various causes (Fig. 44). To distinguish quickly between real iron deficiency and an iron distribution disorder, iron and ferritin levels should be determined.
|
|
|
|
|
Hypochromic Anemias |
129 |
|
|
|
|
|
|
|||
|
|
|
|
|
|||
|
Insufficient iron absorption: |
|
Chronic bleeding and pathological |
|
|||
|
● |
Lower than normal acidity, no |
|
loss of iron in the following diseases: |
|
||
|
|
|
|
|
|
||
|
|
acidity, stomach resection, |
|
● |
Disorders of the stomach and |
|
|
|
|
accelerated passage from |
|
|
intestines (positive benzidine |
|
|
|
|
stomach to intestines |
|
|
test) |
|
|
|
● |
Substances that inhibit ab- |
|
● |
Diseases of the urethra |
|
|
|
|
sorption of iron, such as citric |
|
|
(hematuria!) |
|
|
|
|
acids and lactic acids, mucus and |
|
● |
Diseases of the female repro- |
|
|
|
|
similar materials |
|
|
ductive cycle (menorrhagia, |
|
|
|
● |
Substances that facilitate iron |
|
|
metrorrhagia) |
|
|
|
|
absorption are missing |
|
|
|
|
|
|
|
(e.g. vitamin C) |
|
|
|
|
|
|
|
|
|
|
|
|
|
Insufficient iron supplementation:
●Iron-deficient diet
●In newborns: insufficient iron transfer from the mother during gravidity
Increased iron requirement:
●Growth/maturation
●Increased production of the new blood cells
Endogenous redistribution:
●Tumors, infections, lung hemosiderosis
Physiological iron loss in females:
●Menses
●Lactation
●Pregnancy
Iron deficiency:
●Fatigue, koilonychia, infectious angle (angulus infectiosus oris), PlummerVinson syndrome, possibly “iron deficiency fever”
●Anemia
●Hypochromy, ring-shaped erythrocytes
●Light serum, deficient in color components
●Serum iron very reduced
Fig. 44 The most important reasons for iron deficiency (according to Begemann)

130 Erythrocyte and Thrombocyte Abnormalities
Table 22 Diagnostic findings and work-up for the most important disorders of the red cell series
Clinical |
Hb |
MCH |
Erythro- |
Reti- |
Leuko- |
Seg- |
Lym- |
Other cells |
Throm- |
findings |
|
|
cyte mor- |
culo- |
cytes |
mented |
pho- |
|
bocytes |
|
|
|
phology |
cytes |
|
nuclei |
cytes |
|
|
|
|
|
|
|
|
(%) |
(%) |
|
|
Fatigue, |
! |
! |
Ring-shaped |
! |
n |
n |
n |
- |
n/" |
pallor |
|
|
erythrocytes, |
|
|
|
|
|
|
(dysphagia) |
|
|
anisocytosis |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Possibly |
! |
! |
Anisocytosis, |
! |
n/" |
n |
n |
Possibly |
n |
fever, weight |
|
|
poikilocytosis |
|
|
|
|
eosinophils |
|
loss |
|
|
|
|
|
|
|
" |
|
|
|
|
|
|
|
|
|
monocytes " |
|
|
|
|
|
|
|
|
|
left shift |
|
Diffuse |
! |
!/n/" All sizes, |
! |
n/! |
n |
n |
- |
n/! |
|
symptoms |
|
|
dimorphic |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Acute |
! |
n |
n |
n |
n |
(") |
(!) |
- |
n/!/" |
hemorrhage |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Subjaundice |
! |
n |
n or pathol., |
"" |
n/! |
n |
n |
Possibly nor- |
n/! |
|
|
|
possibly |
|
|
|
|
moblasts |
|
|
|
|
spherocytes |
|
|
|
|
|
|
Spleen " |
! |
! |
Target cells |
" |
n |
n |
n |
Possibly nor- |
n |
|
|
|
|
|
|
|
|
moblasts |
|
|
|
|
|
|
|
|
|
|
|
Paller |
! |
n |
n |
!! |
! |
! |
" |
Possibly |
!! |
possibly |
|
|
|
|
|
|
|
monocytes" |
|
infections |
|
|
|
|
|
|
|
|
|
and bleeding |
|
|
|
|
|
|
|
|
|
tendency |
|
|
|
|
|
|
|
|
|
Pallor |
! |
" |
Macrocytes, |
! |
! |
! |
" |
Possibly |
!/n |
possibly |
|
|
megalocytes |
|
|
|
|
hyperseg- |
|
alcohol his- |
|
|
|
|
|
|
|
mented |
|
tory |
|
|
|
|
|
|
|
granulocytes, |
|
|
|
|
|
|
|
|
|
possibly nor- |
|
|
|
|
|
|
|
|
|
moblasts |
|
Plethora, |
" |
n |
n |
n |
n/" |
n |
n |
- |
n/" |
possibly |
|
|
|
|
|
|
|
|
|
spleen |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Acute bleed- |
! |
n |
n |
(") |
n |
n |
n |
- |
!! |
ing tendency |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Diagnostic steps proceed from left to right. The next step is usually unnecessary; :. the next step is optional; #the next step is obligatory. n = normal value, != lower than normal, "= elevated, ( ) = test not relevant, BSG = erythrocyte sedimentation rate.
|
|
|
|
|
|
|
Hypochromic Anemias |
131 |
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
BSG |
Elec- |
Iron |
Ferritin |
Trans- |
|
Tentative |
Evidence/ |
|
Bone marrow |
Ref. |
|
||
|
tro- |
|
and |
ferrin |
|
diagnosis |
further diag- |
|
|
page |
|
||
|
pho- |
|
others |
|
|
|
nostics |
|
|
|
|
||
|
resis |
|
|
|
|
|
|
|
|
|
|
|
|
n |
n |
! |
Ferritin |
" |
|
Iron deficiency |
Determine |
|
Erythropoiesis " p. 132 |
|
|||
|
|
|
! |
|
|
anemia |
source of bleed- |
sideroblasts !, |
|
|
|||
|
|
|
|
|
|
|
ing; check iron |
|
iron in macro- |
|
|
||
|
|
|
|
|
|
|
absorption |
|
phages ! |
|
|
||
|
|
|
|
|
|
|
|
|
|
. |
|
|
|
" |
? α2" ! |
Ferritin |
! |
|
Acquired/sec- |
Search for |
|
Erythropoiesis !, |
p. 134 |
||||
|
γ" |
|
n/" |
|
|
ondary anemia |
trigger |
|
sideroblasts ! |
|
|
||
|
|
|
|
|
|
(infectious/ |
|
|
|
|
iron in macro- |
|
|
|
|
|
|
|
|
toxic, paraneo- |
|
|
|
|
phages" |
|
|
|
|
|
|
|
|
plastic) |
|
|
|
. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
n |
n |
" |
n/" |
! |
|
Sideroachrestic |
|
|
# |
|
Erythropoiesis ", |
p. 106 |
|
|
|
|
|||||||||||
|
|
|
|
|
|
anemia, |
|
|
|
|
ring sideroblasts |
|
|
|
|
|
|
|
|
myelodysplasia |
|
|
|
|
present |
|
|
n |
n |
n/! – |
n/" |
|
Anemia due to |
Search for |
|
(Erythropoiesis |
p. 140 |
|
|||
|
|
|
|
|
|
hemorrhaging |
source and |
|
") |
|
|
||
|
|
|
|
|
|
|
reason for |
|
|
|
|
||
|
|
|
|
|
|
|
hemorrhages |
|
|
|
|
||
n |
n |
n |
Hapto- |
(n/!) |
|
Hemolytic |
Osmotic |
|
(Erythropoiesis |
p. 140 |
|
||
|
|
|
globu- |
|
|
anemia |
resistance, |
|
", right shift) |
|
|
||
|
|
|
lin !! |
|
|
|
Coombs test, |
|
increased storage |
|
|
||
n |
n |
n |
Hapto- |
|
|
Especially: |
Hb electro- |
|
of iron |
|
|
||
|
|
|
|
p. 138 |
|||||||||
|
|
|
globu- |
|
|
thalassemia |
phoresis and |
|
|
||||
|
|
|
|
|
|
|
|
|
|||||
|
|
|
lin !! |
|
|
|
further tests |
. |
|
|
|
||
" |
n |
"/(n) |
n/" |
(!/n) |
|
Aplastic ane- |
Search for trig- |
|
Hypoplasia of all |
p. 146, |
|
||
|
|
|
|
|
|
mia or bone |
ger or tumor |
|
cell series, or car- |
148, 150 |
|
||
|
|
|
|
|
|
marrow carci- |
|
|
|
|
cinoma cells |
|
|
|
|
|
|
|
|
nosia |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
n |
n |
n/" Vitamin |
(!) |
|
Megaloblastic |
Gastroscopy, |
|
Erythropoietic |
p. 152 |
||||
|
|
|
B12 |
|
|
anemia |
determination |
|
megaloblasts |
|
|
||
|
|
|
folic acid |
|
|
|
of antibodies, |
|
|
|
|
||
|
|
|
! |
|
|
|
possibly |
|
|
|
|
||
|
|
|
|
|
|
|
Schilling test |
|
|
|
|
||
n/! n |
! |
" |
" |
|
Polyeythemia, |
ALP, progress- . |
Erythropoiesis " p. 162 |
|
|||||
|
|
|
|
|
|
DD: hypergam- |
ion |
|
|
|
|
||
|
|
|
|
|
|
maglobuline- |
|
|
|
|
|
|
|
|
|
|
|
|
|
mia |
|
|
|
|
|
|
|
n |
n |
! |
duration |
– |
|
Thrombocyto- |
Search for trig- |
|
Elevated mega- |
p. 166 |
|
||
|
|
|
of |
|
|
penic purpura |
gers, possibly |
|
karyocyte count |
|
|
||
|
|
|
hemor- |
|
|
(ITP) |
also for anti- |
|
|
|
|
||
|
|
|
rhaging |
|
|
|
bodies |
|
|
|
|
||
""
PTT n

132 Erythrocyte and Thrombocyte Abnormalities
Table 23 Normal ranges for physiological iron and its transport proteins
|
Old units |
SI units |
Serum iron |
150–200 µg/dl |
27–36 µmol/l |
Newborns |
||
Adults |
|
|
Female |
60–140 µg/dl |
11–25 µmol/l |
Male |
80–150 µg/dl |
14–27 µmol/l |
TIBC |
300–350 µg/dl |
54–63 µmol/l |
Transferrin |
250–450 µg/dl |
2.5–4.5g/l |
Serum ferritin |
|
30–300 µg/l |
|
(15–160 µg/l premenopausal) |
|
|
|
|
TIBC = Total iron binding capacity.
This usually renders determination of transferrin and total iron binding capacity (TIBC) unnecessary. If samples are being sent away to a laboratory, it is preferable to send serum produced by low-speed centrifugation, since the erythrocytes in whole blood can become mechanically damaged during shipment and may then release iron. Table 23 shows the variation of serum iron values according to gender and age.
It is important to note that acute blood loss causes normochromic anemia. Only chronic bleeding or earlier serious acute blood loss leads to iron deficiency manifested as hypochromic anemia.
Iron Deficiency and Blood Cell Analysis Focusing on the erythrocyte morphology is the quickest and most efficient way to investigate hypochromic anemia when the serum iron has dropped below normal values. In hypochromic anemia with iron and hemoglobin deficiency (whether due to insufficient iron intake or an increased physiological iron requirement), erythrocyte size and shape does not usually vary much (see Fig. 45). Only in advanced anemias (from approx. 11 g/dl, equivalent to 6.27 mmol/l Hb) are relatively small erythrocytes (microcytes) with reduced MCV and MCH and grayish stained basophilic erythrocytes (polychromatic erythrocytes) seen, indicating inadequate hemoglobin content. Cells with the appearance of relatively large polychromatic erythrocytes are reticulocytes. The details of their morphology can be seen after supravital staining (p. 141). A few target cells (p. 139) will be seen in conditions of severe iron deficiency.
In severe hemoglobin deficiency (! 8 g/dl, equivalent to 4.96 mmol/l) the residual hemoglobin is found mostly at the peripheral edge of the erythrocyte, giving the appearance of a ring-shaped erythrocyte.
 Small, hemoglobin-poor erythrocytes indicate iron deficiency
Small, hemoglobin-poor erythrocytes indicate iron deficiency
a 
 b
b
c 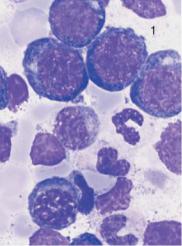
 d
d
Fig. 45 Iron deficiency anemia. a and b Erythrocyte morphology in iron deficiency anemia: ring-shaped erythrocytes (1), microcytes (2) faintly visible target cells (3), and a lymphocyte (4) for size comparison. Normal-sized erythrocytes (5) after transfusion. c Bone marrow cytology in iron deficiency anemia shows only increased hematopoiesis and left shift to basophilic erythroblasts (1). d Absence of iron deposits after iron staining (Prussian blue reaction). Megakaryocyte (1).
133
