
1-280 pdf (1)
.pdf
Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
2.3. ACUTE BRONCHITIS
Definition. Acute bronchitis is an acute inflammation of the bronchial mucosa. The prevalence of acute bronchitis among the adult population is the same among
men and women, little dependent on age. There is no reliable data on the true prevalence of acute bronchitis, since often patients do not go to the doctor or the disease
treated as an acute respiratory viral infection. However, according to some authors, acute bronchitis with temporary disability account for about 38% of all bronchopulmonary diseases.
The etiology of acute bronchitis is diverse. The causes of this disease include viral and bacterial infections, allergens, toxic effects, chemical agents, physical factors (cold or, conversely, hot air), and radiation. Viral infections are the most common cause of acute bronchitis.
or viral-bacterial infections, and with a mixed nature of the infection, along with viruses that are detected in 70% of cases, pneumococcus (in 60%), mycoplasma (38%), Haemophilus influenzae (16% of cases) are detected.
Pathogenesis. The inflammatory process in acute viral bronchitis is descending character, as in acute respiratory diseases, affecting the nasopharynx, larynx, trachea, large bronchi. Viral infection damages the epithelial lining of the mucosa
bronchi, leads to the death and desquamation of epithelial cells, impaired mucociliary
clearance. At the same time, irritant receptors are exposed, which increase the sensitivity of the bronchi to the impact of nonspecific environmental factors (cold or hot dry air, tobacco smoke, etc.),
which contributes to the appearance of such a symptom as cough. In parallel with the death of the epithelium, the number and size of goblet cells increase. In allergic bronchitis, a large amount of biologically active substances (histamine,
cytokines, leukotrienes) secreted by mast and other inflammatory cells occurs increased vascular permeability, mucosal edema and bronchospasm develop.
Morphology. Respiratory viruses cause focal or diffuse degeneration
and desquamation of cells of the cylindrical epithelium already in the first three days of illness. maybe damage to the submucosal layer. In bacterial infection, it becomes infiltrated
neutrophils and lymphocytes. The involvement of the allergic mechanism of inflammation is manifested vasomotor edema of the mucous membrane, the predominance of eosinophils among the cells penetrating the walls of the bronchi.
Classification. In our country, a classification has become widespread, suggesting
wife A. N. Kokosov in 1984, according to which, according to the etiology, bronchitis is divided into:
1.Infectious (viral, mycoplasmal, bacterial, mixed).
2.Caused by physical or chemical factors.
3.Radiation.
4.Mixed.
By pathogenesis, primary and secondary bronchitis are distinguished (against the background of previous
diseases in the upper (sinusitis, tonsillitis) and lower respiratory tract (more often posttuberculosis changes in the bronchi, bronchiectasis).
The classification of acute bronchitis, presented in the International Classification of Diseases of the 10th revision, is based on the etiological principle. There are acute bronchitis caused by: mycoplasma, Haemophilus influenzae, streptococci, various viruses, other specified agents and acute bronchitis, unspecified.
271

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
According to the characteristics of the course of the disease, it is proposed to distinguish between acute and subacute bronchitis: with bronchospasm, with tracheitis, fibrinous, membranous, purulent, septic and tracheal bronchitis.
Allergic bronchitis is classified under the heading "Asthma". clinical picture. Acute bronchitis often occurs after acute
respiratory disease or at the same time. Therefore, the clinical picture of acute
bronchitis consists of symptoms of viral intoxication: chilling, increased body temperature
(up to 38 ° C, less often above 38 ° C), general weakness, muscle pain, hyperemia of the pharynx; and symptoms of tracheobronchitis: hacking dry cough, chest pain associated with
damage to the trachea. Then sputum appears, usually mucous; when a bacterial infection is attached, the sputum becomes mucopurulent.
Physical examination data are scarce. Harsh breathing usually attracts attention, in smokers suffering from chronic bronchitis, you can listen to
dry dry wheezing.
Laboratory and instrumental diagnostics. Results of laboratory and
instrumental examination of patients is of little help in the diagnosis of acute bronchitis. AT a clinical blood test most often shows a normal number of leukocytes or
tendency to leukopenia. However, neutrophilia with a moderate stab shift is often noted
in the blood formula; severe eosinophilia is possible in allergic bronchitis. The erythrocyte sedimentation rate does not change significantly.
An x-ray may show an increase in lung
pattern, blurring of the roots of the lungs. Bronchoscopy reveals signs of catarrhal
less often purulent inflammation, diffuse hyperemia and swelling of the bronchial mucosa. Sputum, as a rule, the mucous membrane contains a large number of desquamated epithelial
cells, macrophages, and often single erythrocytes. With the addition of a bacterial infection, sputum becomes mucopurulent, contains a moderate (up to 40 - 50%) number of neutrophils;
with allergic bronchitis, eosinophils appear, often in large numbers. In clarifying the nature of the etiological agent, virological, bacteriological
and serological testing.
Diagnosis. In the formulation of the diagnosis, it is recommended to include the etiological factor and
reflect in it the features of the course of the disease.
Diagnosis examples:
1.Acute bronchitis, viral (caused by rhinovirus).
2.Acute bronchitis, unspecified.
3.Acute chemical bronchitis.
Differential diagnosis of acute bronchitis has to be carried out with pneumonia, ingress of a foreign body into the bronchi, exacerbation of chronic bronchitis. Anamnesis data (presence of chronic respiratory diseases) helps to clarify the diagnosis.
ways, duration of cough), x-ray examination (the presence of shading in the lungs pneumonia), bronchoscopy.
Course, prognosis, outcomes. The course of acute bronchitis of infectious etiology in mostly easy. Gradually, within two to three weeks, the cough disappears, the temperature
returns to normal. Sometimes the disease takes a protracted character, lasting more than three weeks. In cases of repeated acute bronchitis in a patient (more than three during the year), one
can speak of recurrent bronchitis. The prognosis for acute bronchitis is usually favorable. Recovery occurs within 2 - 3 weeks.
Treatment of patients with acute bronchitis is most often carried out at home and includes the following activities:
272

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
1. Fight against viral intoxication (plentiful warm drink with the use of diaphoretic and antipyretic agents: honey, raspberry, lime blossom). 2. Maintaining
the drainage function of the bronchi: warm steam inhalations, inhalations of herbal infusions (up to 6-8 times a day), expectorants and mucolytics (bromhexine 1-2 tablets 3 times a day, lazolvan, acetylcysteine, solutan, broncholithin).
3.Etiotropic therapy, which is used as antiviral drugs (rimantadine, arbidol, amixin) for viral etiology of bronchitis. Antibacterial therapy is carried out with the addition of a bacterial infection (mucopurulent sputum, recurrence of fever). Recommended: amoxicillin (250-500 mg 2 times a day), clarithromycin (250-500 mg 2 times a day) for 5-7 days.
4.Symptomatic therapy, which includes bronchodilators (if necessary) - salbutamol (1 inhalation 3-4 times a day), berodual in the same dose, with allergic bronchitis - ditek (1-2 inhalations 4 times a day ).
273

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
2.4. PNEUMONIA
Definition. Pneumonia is a group of acute infectious (mainly bacterial) diseases of different etiology, pathogenesis, morphological characteristics, characterized by focal lesions of the respiratory sections of the lungs with the obligatory presence of intraalveolar exudation, detected during physical and/or instrumental examination, and also expressed in varying degrees of febrile reaction and toxicity.
Prevalence. Pneumonia is one of the most widespread diseases. According to the calculated data, the incidence of community-acquired pneumonia in Russia is 14– 15 ‰, and the total number of patients annually exceeds 1.5 million people. In the United States, more than 5 million cases of community-acquired pneumonia are diagnosed each year, in which more than 1.2 million people require hospitalization, and more than 60,000 patients die directly from pneumonia.
Mortality in community-acquired pneumonia is the lowest in young and middleaged people without concomitant diseases (1-3%). On the contrary, in patients over 60 years of age with serious concomitant pathology of various organs and systems, this figure reaches 15–30%.
The classification that most fully reflects the features of the course of pneumonia and allows justifying etiotropic therapy is based on the etiological principle. In this regard, the following main types of pneumonia are distinguished: 1.
Bacterial. 2. Viral. 3. Mycoplasma. 4. Chlamydia. 5. Legionella. 6. Fungal. 7.
Parasitic. 8. Mixed. 9. Pneumonia without specifying the pathogen. Unfortunately, in practice, the implementation of timely etiological diagnosis of pneumonia is
difficult due to insufficient information content and the significant duration of traditional microbiological studies. Therefore, taking into account the conditions
in which the disease developed, the characteristics of infection of the lung
tissue, as well as the state of the immunological reactivity of the patient'sbody, a classification of pneumonia was proposed.
1. Community-acquired (primary, home), acquired. 2. Hospital (secondary, nosocomial, nosocomial). 3. Aspiration pneumonia. 4. Pneumonia in persons with severe immunity defects (congenital immunodeficiency,
HIV infection, iatrogenic immunosuppression). According to the prevalence and localization of pneumonia, they are divided into: 1. Lobular. 2.
Subsegmental. 3. Segmental. 4. Equity. 5. Unilateral. 6. Bilateral. In terms of severity:
274
Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
1.Easy.
2.Moderate. 3. Heavy. By the
nature of the flow to: 1. Acute. 2. Protracted. There are also the most
frequent complications of pneumonia: 1. Infectious-
toxic shock. 2. Exudative pleurisy. 3. Distress syndrome. 4. Syndrome of disseminated intravascular coagulation. 5. Infectious destruction. 6. Infectious-
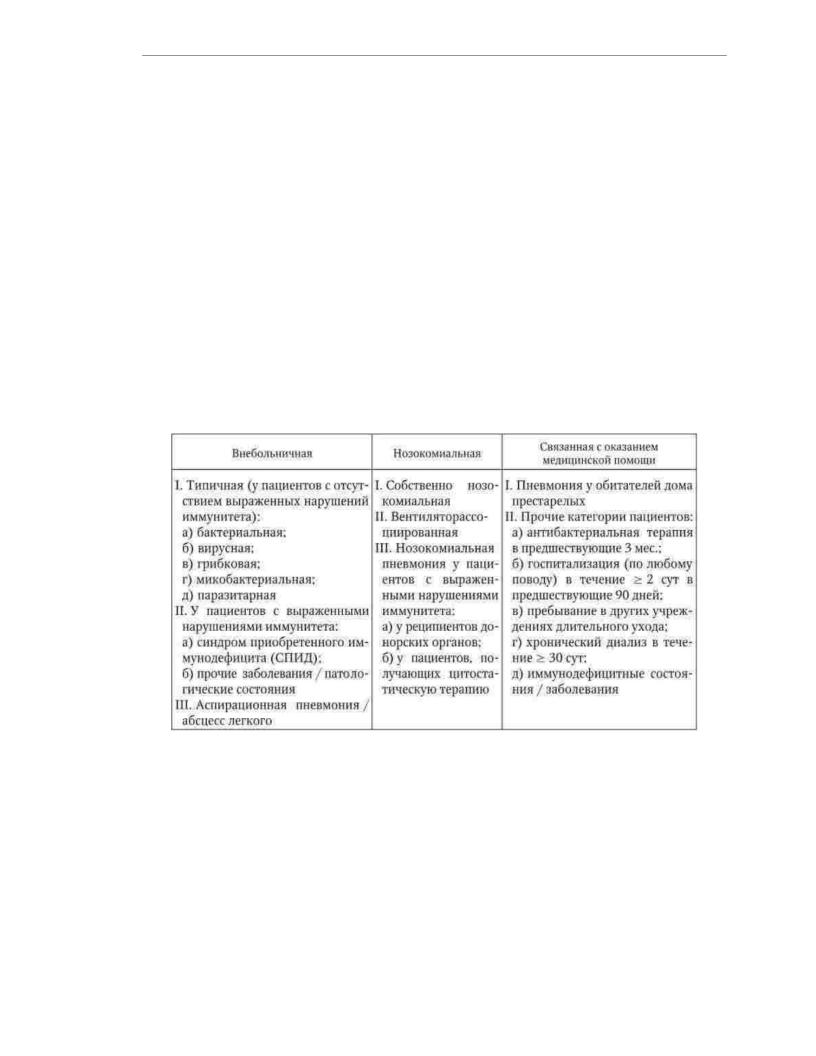
allergic myocarditis. 7. Bronchospasmic syndrome. In 2006, a classification was proposed with a more detailed indication of the conditions for the occurrence of pneumonia (Table 2.2).
Table 2.2
Classification of pneumonias (Winderink RG, Multu GM, 2006, as amended)
In the practice of a doctor, community-acquired pneumonia is most common, which should be understood as an acute disease that occurs in a communitythatis, outsidesetting,the hospital, or later than 4 weeks. after discharge from it, or diagnosed in the first 48 hours from the moment of hospitalization, or developed in a patient who was not in nursing homes of the long-term care unit 8-14 days, accompanied by symptoms of a lower respiratory tract infection (fever, cough, sputum production, possible, purulent, chest pain, shortness of breath) and radiological signs of "fresh" focal-infiltrative changes in the lungs in the absence of an obvious diagnostic alternative. Etiology. Various infectious agents can cause pneumonia. The etiology of primary pneumonia
is directly related to the normal microflora of the "non-sterile" parts of the upper respiratory tract (oral cavity, nose, oropharynx and nasopharynx). Of the many
275

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
species of microorganisms that colonize the upper respiratory tract, only a few with increased virulence are capable of penetrating into the respiratory sections
lungs to cause an inflammatory reaction even with minimal violations of protective mechanisms. Typical causative agents of bacterial pneumonia are:
–Streptococcus pneumoniae (pneumococcus) – gram-positive cocci, the most common pathogens of pneumonia in all age groups; – Haemophilus influenzae (haemophilus influenzae)
–gram-negative rods that cause pneumonia in 5–18% of adults, more often in smokers and patients with chronic obstructive bronchitis; – Moraxella (Branhamella) catarrhalis – gramnegative coccobacteria, relatively
rarely causing pneumonia (1 - 2% of patients) in patients with concomitant chronic bronchitis;
- Mycoplasma pneumoniae - a microorganism devoid of an outer membrane - causes pneumonia in 20 - 30% of people under 35 years of age and 1 - 9% of patients in older age groups. This microorganism is characterized by membranotropism, and it is also possible intracellular
localization;
- Chlamidophila pneumoniae - a microorganism that is exclusively an intracellular parasite, similar in structure to gram-negative bacteria; causes pneumonia in 2-8% of cases, usually mild.
Some microorganisms are normally rarely found in the composition of the microflora of the upper respiratory tract. They are detected and can cause the development of pneumonia in
persons of older age groups with concomitant severe chronic diseases other organs and systems. These microorganisms include:
–Escherichia coli, Klebsiella pneumoniae – causative agents of primary pneumonia (less than 5% cases) in patients with diabetes mellitus, renal, hepatic insufficiency, etc.
–Staphylococcus aureus – relatively rare (less than 5% of cases) causes pneumonia
in the elderly, drug addicts, who are on chronic hemodialysis, who carry the flu.
The causative agents of primary pneumonia usually include microorganisms of the genus Legionella - gram-negative rods, which are obligate pathogens. Legionella spp. (before
total, Legionella pneumoniae) is a relatively rare causative agent of pneumonia (2-10% of cases), however, legionella pneumonia ranks second (after pneumococcal) in terms of death rate of the disease.
Respiratory viral infections, primarily epidemic influenza, are by far the main risk factor for developing pneumonia, however, according to most scientists, they rarely cause pneumonia in adults. At the same time, in children of early
age viruses can cause pneumonia, which is morphologically characterized damage to the interstitial tissue of the interalveolar septa.
In secondary (hospital) pneumonia, the role of gram-negative microorganisms and conditionally pathogenic flora is great. This is primarily Staphylococcus aureus, the occurrence which is 2.7 - 30%. Klebsiella pneumoniae accounts for 2.7–12.6% of pneumonias. The specific gravity of Escherichia coli is 17.3 - 32.3%, Proteus vulgaris - 8.1 - 24%. Very
Pseudomonas aeruginosa plays an important role in the etiology of nosocomial pneumonia. (Pseudomonas aeruginosa) - 17% of cases. Legionella pneumoniae is very often the causative agent of nosocomial pneumonia (up to 33% of cases).
The etiology of aspiration pneumonia is characterized by the participation of nonclostridial anaerobes (Bacteroides spp., Micoplasma spp., Candida spp.), often in combination with aerobic Gram-negative microflora (Haemophilus influenzae, Enterobacterioceae).
276

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
In the development of pneumonia in people with severe immunological disorders involved cytomegalovirus infection, Pnemocystis carinii, pathogenic fungi, mycobacterium tuberculosis, along with other microorganisms found in other pneumonias.
Pathogenesis. There are four main ways of penetration into the lungs of causative agents of pneumonia: aspiration of oropharyngeal secretions; inhalation of an aerosol containing microorganisms; hematogenous spread of microorganisms from an extrapulmonary focus of infection; direct spread of infection from adjacent diseased tissues (eg,
liver abscess) or as a result of infection with penetrating wounds of the chest.
Aspiration of the contents of the oropharynx is the main route of infection of the respiratory parts of the lungs and, therefore, the main pathogenetic mechanism for the development of pneumonia. It should be noted that microaspiration of oropharyngeal secretions is a physiological
a phenomenon that is observed in 70% of healthy individuals during sleep. However, under normal conditions, the cough reflex, mucociliary clearance, antibacterial activity of alveolar macrophages and secretory immunoglobulins provide elimination
(removal) of infected secretions from the lower respiratory tract. In the case of damage to the mechanisms of "self-cleaning" of the tracheobronchial tree, for example, with respiratory viral infection, when the function of the cilia of the bronchial epithelium is impaired and the
phagocytic activity of alveolar macrophages decreases, favorable conditions are created for the development of pneumonia. After bacteria enter the lower respiratory tract, they
adhesion on the surface of epithelial cells, penetration into the cytoplasm and reproduction.
The adhesion factors are fibronectin and sialic acids contained in epithelial cells. cheek cells.
The first line of defense of the lower respiratory tract against the bacterial flora are alveolar macrophages, which attract polymorphonuclear leukocytes and blood monocytes to the site of inflammation by chemotaxis, with the participation of complement and Fc receptors. Then
the activation of the complementary cascade occurs after damage to epithelial and endothelial cells, which leads to increased migration of polymorphonuclear leukocytes and erythrocytes to the inflammation site. Complement factors (C5a and C3b) promote extravasation of immunoglobulins, albumin, and other serum factors. All this is accompanied
increased production of pro-inflammatory cytokines, enzymes, procoagulants, increased
exudation of the liquid part of the plasma into the alveoli and ends with the formation of an inflamed focus
niya.
Inhalation of an aerosol containing microorganisms is a less frequently observed route
development of pneumonia.
The hematogenous route of infection is observed in sepsis, septic endocarditis, some infectious diseases.
Morphology. For different types of pathogens, features of the macroand microscopic picture of pneumonia are characteristic.
With pneumococcal pneumonia, as a rule, lobar pleuropneumonia develops, in
the classic version - with the presence of stages of hot flashes, red and gray hepatization (croupous pneumonia). In the initial stage, hyperemia and serous exudation develop, and
exudate contains pneumococci. This is followed by the stage of erythrocyte migration with the development red hepatization, followed by migration of leukocytes (gray hepatization),
pneumococcal phagocytosis and fibrin shedding. In the future, after the death of microbes, resorption of the exudate occurs. However, in practice, a combination of morphological features of all stages is found in the lungs. Pneumococcal pneumonia rarely develops
gangrene and abscesses, but foci of pneumosclerosis (carnification) are frequent. Microscopically in the first two stages are dominated by erythrocytes and fibrin in the alveoli, subsequently appear polymorphonuclear leukocytes, and then macrophages.
277

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
Hemolytic streptococcus leads to the development of secondary postviral pneumonia, often associated with sepsis or being its manifestation. Pneumonia wears like
as a rule, focal (lobular) character, less often the process extends to the whole lobe. Microscopically determined hyaline membranes in the alveoli at an early stage of the process, in the infiltrate, polymorphonuclear leukocytes predominate, often lysed by bacterial enzymes, which gives the alveolar exudate a pulverulent character. Often formed
necrosis of the central part of the inflammatory infiltrate, followed by abscess formation and
development of pleural empyema.
Staphylococcus aureus causes primary and secondary pneumonia, often associated with epidemics of influenza A and B, which develops in patients after neurosurgical operations in a coma, suffering from cystic fibrosis. Histologically
polymorphonuclear leukocytes predominate in the infiltrate;
many bacteria are found. Pleural empyema occurs in adults in 20% of cases, in children - in 75%.
Pneumonia caused by gram-positive bacteria (aerobes) is mainly
secondary in nature and develop in patients with weakened immunity (with alveolar proteinosis, lymphosarcoma), rarely are primary when ingested with soil aerosol.
Typical for this type of pneumonia is the presence of foci of necrosis, abscesses with a diameter 1 - 10 µm. On the periphery of abscesses, accumulations of epithelioid cells are observed. Such pneumoniae can be either lobular or lobar.
Gram-negative bacteria (enterobacteria) cause pneumonia in patients with alcoholism, diabetes mellitus, and chronic obstructive bronchitis. Pneumonia wears,
as a rule, focal character, abscesses and an empyema of a pleura are frequent.
Klebsiella pneumonias are more often secondary, in terms of prevalence - lobar, they are characterized by carnification. Abscesses are found in 60 - 70% of cases
and gangrene. Histologically, the cellular infiltrate is 50% composed of polymorphonuclear leukocytes.
Yersinia pneumonia is characterized by multiple hemorrhages, edema, and the absence of fibrin in the alveoli. The alveolar exudate mainly consists of macrophages with a meager admixture of polymorphonuclear leukocytes and a large number of bacteria. Often
necrosis of the interalveolar septa occurs.
Haemophilus influenzae causes secondary pneumonia, more common in patients with chronic obstructive pulmonary disease after a viral infection. Such
pneumonia can be lobar, focal or polysegmental. In the lumen of the alveoli, accumulations of polymorphonuclear leukocytes and / or macrophages, fibrin are found; the pathogen is rare. Destruction of the interalveolar septa and fibroplastic proliferation are characteristic. Pleural empyema and abscesses are rare.
Pseudomonas aeruginosa causes secondary pneumonia in patients with cystic fibrosis, leukemia, and HIV infection. This type of pneumonia is characterized by bacteremia, development of necrosis, hemorrhage, focal lesion of the visceral pleura. Macroscopically, pneumonia is defined as yellow peribronchial lesions. Microscopically in the alveoli
detect accumulations of erythrocytes, a small number of polymorphonuclear leukocytes and destruction of interalveolar septa, absence of vascular thrombosis and wall necrosis
alveoli.
clinical picture. Clinical signs of pneumonia differ significantly
variety depending on the severity of symptoms of lung and bronchial lesions, as well as the severity of the course of the disease.
278

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
The clinical picture is most pronounced in the severe course of the disease. The occurrence of croupous pneumonia is mostly associated with hypothermia, although in In some cases, the apparent cause of the disease remains unclear.
The disease begins acutely, pain suddenly appears, more often in the lateral parts of the chest, aggravated by inhalation, pronounced chills, followed by an increase in temperature to 39 ° C and above, a feeling of congestion in the chest, a feeling of "brokenness", general weakness, shortness of breath and dry cough. On the second day, when coughing, sputum of a mucopurulent nature begins to separate, which often has a “rusty” color due to the erythrocytes contained in it. When examining a patient, attention is drawn to his
a pale, haggard face with the wings of the nose swollen with breathing; after 1 - 2 days
after the onset of the disease, herpes may appear on the nose and / or lips, shortness of breath, lagging behind one half of the chest during breathing due to pain (sometimes the patient spares her, holding her hand, trying to lie on her “sore” side). On the side of defeat
a pronounced shortening of the percussion tone (dullness) of various lengths, increased bronchophony and voice trembling are determined. Here the bronchial
breathing and sonorous crepitus at the height of inhalation, which, during the resolution of the inflammatory
process is replaced by wet small and medium bubbling rales.
In the elderly, severe pneumonia can be "masked" by the cerebral disorders (delusions, hallucinations, disorientation).
The temperature response in untreated severe pneumonia is permanent. at the level of 39 - 40 ° C for several days. The length of the febrile period
depends on the adequacy of antibiotic therapy, under the influence of which sometimes there
is a critical decrease in temperature, which may be accompanied by the development of collapse. However, more often the temperature decreases within 2 to 3 days. In parallel with the decrease
in temperature, the symptoms of intoxication (headache, general weakness) disappear, and appetite appears. Community-acquired pneumonia most often has a lower lobe localization, although often
there is damage to the upper and middle lobes.
With timely diagnosis and rational treatment, community-acquired pneumonia,
as a rule, flows favorably, especially in young people, and by the end of the 3rd - 4th week
ends with recovery.
Clinical manifestations of community-acquired pneumonia may be different. In some cases they are typical enough for pneumonia. After several days of being unwell, more often associated with a viral infection, a slight chill (chilling), the temperature rises to 38-39 ° C, a cough appears (or the former one intensifies) with a difficult discharge
mucopurulent sputum, there is a feeling of "congestion" in the chest, symptoms of intoxication (headache, general weakness, loss of appetite). Patients often indicate
the side of the lesion, noting there a feeling of "congestion" or pain with a deep breath. The degree of severity of physical changes depends on the localization and prevalence
process: there may be a shortening of the percussion tone, auscultated wet small
and medium bubbling rales, harsh breathing and dry rales, indicating the presence
bronchitis.
With a mild course of the disease, the clinical picture is dominated by symptoms of acute or exacerbation of chronic bronchitis. In these patients, along with fever
and other symptoms of intoxication, signs of bronchitis appear: severe cough,
with a small (at the beginning of the disease) amount of sputum, shortness of breath, shortness of breath, more often
with difficulty exhaling, indicating the development of bronchial obstruction syndrome, at the same time, a large number of dry scattered rales are heard.
Hospital-acquired (nosocomial) pneumonia is defined as pneumonia developing 48 hours or more after hospitalization (provided there is no infection).
279

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
in the incubation period at the time of admission of the patient to the hospital). In the mechanisms of development of pneumonia, aspiration into the respiratory tract of colonizing pathogenic microorganisms from the oropharynx or stomach plays an important role. The clinical picture most often indicates
severe pneumonia: pronounced intoxication syndrome and respiratory failure. Characterized by high temperature (more than 38 ° C), severe shortness of breath, tachycardia, a coma may develop. In a large percentage of cases, complications such as pyopneumothorax, pleural empyema, exudative pleura develop.
rit, atelectasis.
Close to the group of nosocomial pneumonia are aspiration pneumonia, which most often occurs in people suffering from alcoholism, drug addiction. It should be noted that aspiration pneumonia often proceeds as destructive processes, while often there is a large number of foci of lung tissue decay, the formation of abscesses.
A special group consists of patients in whom pneumonia occurs against the background of an altered immunological status. These are mainly patients with acute and chronic myeloid and lymphoproliferative diseases, persons infected with the AIDS virus. The spectrum of pathogens that cause pneumonia in this category of patients is very wide: viruses (gerpes, cytomegaloviruses), grampositive and gram-negative bacteria, mycobacterium tuberculosis, pneumocysts, fungi. Often, such pneumonia proceeds atypically with a dim clinical picture, which makes it difficult to diagnose. Laboratory and instrumental diagnostics. The leading role in the diagnosis of pneumonia, in addition to
the clinical picture, is played by X-ray examination of patients. A survey radiograph of the lungs (in frontal and lateral projections) in the first days of the disease reveals in 90–95% of patients shading without clear contours, focal or confluent,
which can extend to a segment, several segments, a share, sometimes two or three shares
in one or both lungs (Fig. 2.1).
Rice. 2.1. Plain radiograph of the lungs with pneumonia: a - direct projection; b - lateral projection
The most common localization of pneumonia are the lower lobes, the middle lobe of the right lung, less often the upper lobes. Along with the lesion of the respiratory part of the lungs, changes in the interstitial tissue are detected, which is radiologically manifested by the fuzziness of the pulmonary pattern of the contours of the bronchi and blood vessels. The root of the lung on the side of the lesion is usually enlarged, but enlarged lymph nodes most often cannot be identified. It is often possible to detect a reaction of the pleura (interlobar, diaphragmatic) or fluid in the pleura
280
