
1-280 pdf (1)
.pdf
Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
Ethacizin. A phenothiazine derivative, a diethylamine analogue of etmozine. Trade name: etacizin. Available in tablets of 50 mg. It is prescribed in a daily dose of 100 - 150 mg, the maximum dose is 200 mg / day (3 times). Elimination half-life of ethacizine is about 2.5 hours. One of the most effective class I AARP, which at the same time has a small therapeutic breadth, a pronounced proarrhythmic effect. In connection with this should not be used in patients with structural changes in the heart, including
in the acute period of MI. Has found its application in the treatment of supraventricular tachyarrhythmias and ventricular arrhythmias in patients without structural changes in the heart. Can be
used to prevent AF paroxysms. It is possible to prescribe to patients with moderate
dysfunction of the SU, as it slightly increases the rate of SR. II class.
ÿ- blockers are of paramount importance due to their ability to significantly reduce the risk of life-threatening ventricular arrhythmias in patients with a high risk of sudden death (after myocardial infarction, with chronic heart failure, etc.). They are the drugs of choice for heart rate control in patients with continuously relapsing AF. and chronic atrial tachycardia; are prescribed for sympathicotonia, accompanied by severe sinus tachycardia, including sympathetic-adrenal crises. The general rule of their appointment is a gradual increase in dose to individually
portable.
Among many others, drugs in this class include those commonly used in arrhythmias atenolol, betaxolol, bisoprolol, metoprolol, nebivolol, propranolol, esmolol.
Atenolol. Selective hydrophilic (water-soluble) ÿ- blocker. Trade names: atenol, atenolol, tenormin, etc. Tablets of 25, 50 and 100 mg. Given in a daily dose
12.5 - 200 mg. Currently, it is used quite rarely, since for the prevention
sudden death, only lipophilic (fat-soluble) ÿ- blockers have been proven effective. The half-life of atenolol is 6-10 hours, which requires twice a day.
Betaxolol. Selective lipophilic ÿ- blocker. Trade names: betak,
kerlon, lokren, etc. Tablets of 20 mg. It is prescribed in a daily dose of 5-20 mg, the maximum dose - 40 mg. The half-life is 12 - 24 hours. It is prescribed once a day.
Bisoprolol. Selective ÿ- blocker with lipophilic and hydrophilic properties. Trade names: Bidop, Bisogamma, Concor, Concor Core, etc. Tablets
2.5, 5 and 10 mg. It is prescribed in a daily dose of 1.25 - 20 mg. Half-life 10 - 12 hours,
given once a day.
Metoprolol. Reference selective lipophilic ÿ- blocker. Trade names: protein, betalok, betalokzok, corvitol, metoprolol, egilok, egilok-retard, etc. Metoprolol tartrate with a half-life of 3-4 hours,
slow release) daily action and metoprolol succinate daily action. Tablets of 25, 50, 100 and 200 mg. It is prescribed in a daily dose of 12.5 - 200 mg (up to 400 mg): metoprolol tartrate - 3-4 times a day, slow-release metoprolol tartrate
and metoprolol succinate - once a day. For intravenous administration - 5.0 ml ampoules 0.1% solution. Enter slowly jet or drip 5 mg, total no more than 20 mg / day.
It is used in the acute period of myocardial infarction, sometimes - to control heart rate during AF.
Nebivolol. The most selective lipophilic ÿ- blocker. It has additional vasodilating properties. Trade name: non-ticket. Tablets of 5 mg. It is prescribed in a daily dose of 2.5-5 mg, the maximum dose is 10 mg. The half-life of nebivolol is 10 hours, of metabolites - 20 hours. It is prescribed once a day.
Propranolol. Non-selective lipophilic ÿ- blocker. Trade names: ana prilin, inderal, obzidan, etc. In Russia, it is available in tablets of 10 and 40 mg. Appointed in
daily dose of 40 - 240 mg, the maximum dose is 320 mg. Half-life of propranolol
241

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
- 2 - 5 hours. It is prescribed 3 - 4 times a day. Rarely used for scheduled reception in communication short half-life, side effects (non-selective drug). In Russia
it is common to prescribe propranolol at a dose of 20–40 mg sublingually for paroxysm FP. It does not have a stopping effect, however, a decrease in heart rate, of course, brings
relief to the patient, while more |
3/4 paroxysms of AF stop spontaneously in |
within a few hours. |
|
Esmolol. Selective lipophilic ÿ- blocker of ultrashort action. Trade name: breviblok. Available only in solution for intravenous administration in
vials of 10 ml (10 mg / ml). Used in the acute period of MI, as well as to control heart rate with FP. There is evidence of a possible reversal effect of esmolol in catecholaminergic paroxysmal AF. It is customary to administer a loading dose of 500 mcg/kg/min.
for 1 min followed by a maintenance infusion of 50 mcg/kg/min for 4 min. At
in the absence of effect, a loading dose is re-introduced, followed by an infusion of 100 ÿg / kg /
min for 4 min. The half-life is 9 minutes. III class.
This class of drugs includes amiodarone, bretylium tosylate, nibentan, sotalol.
and etc.
Amiodarone. Trade names: amiodarone, amiocardin, cardiodarone, cordarone, etc. It is quite reasonably considered the most effective AARP. Available in 200 mg tablets
and ampoules of 150 mg. Amiodarone is slowly absorbed when taken orally and is found in
blood after 0.5 - 4 hours. The maximum concentration is observed after 5 - 6 hours. It is excreted from the body is extremely slow, the half-life is 30 days or more. At continuous reception cumulates.
The therapeutic effect usually occurs within a few days from the onset
intake and reaches a maximum after 2 to 4 weeks, but when using large doses, the effect
comes faster. It is prescribed during the saturation period for 10-14 days at a dose of 600-800 mg/day. day When switching to maintenance therapy, the dose is reduced to 200 - 400 mg / day (2-
multiple admission). Reception with a two-day break per week and without it is possible. At If necessary, the drug is administered parenterally: intravenously drip at a dose of 5-7 mg/kg. Amiodarone is highly effective in all arrhythmias; its use is most justified
in the treatment of patients with structural heart disease. Is the drug of choice
for the treatment of life-threatening ventricular arrhythmias in patients at high risk of sudden death, including in combination with lipophilic ÿ- blockers. His appointment is not
contradicts the ICD. In the treatment of ventricular arrhythmias and paroxysmal AF in patients with chronic heart failure III - IV f. class there is practically no alternative.
Bretylium tosylate. Trade names: bretilat, bretilol, ornid, etc. Available
in ampoules (5% solution - 1.0 ml). The scope of bretylium tosylate is limited to life-threatening ventricular arrhythmias in the acute period of MI. The drug has a pronounced antifibrillatory effect. Without eliminating the actual ventricular fibrillation,
it increases the fibrillation threshold, increases the efficiency of electrical cardioversion.
It is usually administered intravenously in a slow stream at a dose of 5-7 mg/kg of body weight. maybe repeated intravenous administration of the drug at a rate of 1–2 mg/min or its intramuscular administration until a total dose of 30 mg/kg is reached.
Nibentan. Trade name: nibentan. The first domestic AARP III class. Available in ampoules (1% solution of 2.0 ml). Designed for pharmacological cardioversion in AF and other supraventricular tachyarrhythmias. The most appropriate use
with persistent AF. Efficiency exceeds 80%. The half-life is
10 - 12 hours. Introduced only in intensive care units, under monitor control, intravenously drip at a dose of 0.125 mg / kg for 5 minutes. If there is no effect and QT prolongation is more than 500 ms, administration can be repeated after 20 minutes.
242

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
Sotalol. Trade names: darob, sotahexal, sotaleks, etc. Produced in Russia in tablets of 80 and 160 mg, in ampoules of 40 mg. Sotalol is a non-racemic
a mixture of dextrorotatory and levorotatory stereoisomers. 60% of sotalol consists of a levorotatory isomer (l-sotalol), which is half a non-selective ÿ- blocker,
half a potassium channel blocker. The remaining 40% of sotalol is dextrorotatory
isomer (d-sotalol), fully possessing the properties of an antiarrhythmic of the third class. So Thus, a mixture of two stereoisomers (d-, l-sotalol), which is commonly called sotalol, on 30% has beta-blocking activity, and 70% increases the duration of the action potential. The half-life of the drug is 7-15 hours, it is administered twice a day. The average daily dose is 160 - 320 mg, the maximum - 480 mg /
day The parenteral form of sotalol is not widely used.
It is used in the treatment of supraventricular tachyarrhythmias and ventricular
arrhythmias in patients with and without structural changes in the heart. One of the most common AARP for the prevention of AF, but does not have a stopping effect. Not assigned
patients with chronic heart failure IV f. class
IV class.
This class of drugs includes verapamil and diltiazem.
Verapamil. Trade names: verapamil, verogalide, isoptin, lecoptin, finoptin and etc. Available in tablets, dragees and capsules of 40 and 80 mg, tablets and capsules of
prolonged action of 120, 180 and 240 mg. It is usually prescribed in a daily dose of 120-240 mg, the maximum dose is 480 mg / day (3-4 times). Long-acting verapamil is prescribed once a day. The half-life of conventional verapamil is 3-7 hours. It is also available in injection solutions (5 and 10 mg ampoules). Administered intravenously by stream
at a dose of 5 mg for 5 - 10 minutes, less often - 10 mg. Currently used in arrhythmology (not being the drug of choice) only to control heart rate in chronic and persistent AF. The value of verapamil as a drug for stopping AV reentry tachycardias has been lost with the advent of safer and more effective agents (ATP). With paroxysmal
FP is ineffective. It is absolutely contraindicated in AF in patients with manifesting WPW syndrome, since, by blocking the conduction of excitation along the AV node, it contributes to the spread of excitation along an additional pathway and an increase in heart rate. Maybe be used to stop paroxysmal ventricular tachycardia caused by cAMP-triggered activity (from the outflow tract of the right or left ventricle).
Diltiazem. Trade names: altiazem, dilzem, diltiazem, cardizem, cardil, etc. Available in 30 and 60 mg tablets, extended release tablets and capsules
with delayed release (with different duration of action) at 60, 90, 120, 180,
240, 300 mg. Usually prescribed in a daily dose of 90 - 360 mg, the maximum dose is 600 mg / day (3 - 4 times reception). Long-acting diltiazem is given once or twice a day.
The half-life of conventional diltiazem is 3-4.5 hours.
diltiazem are reduced to prescribing it for heart rate control in chronic and persistent FP.
Common side effects for antiarrhythmic drugs are dyspepsia, hypotension, headache and dizziness, visual disturbances, agranulocytosis,
anemia, elevated liver transaminases, lupus-like syndrome (procainamide)
etc. In the treatment with amiodarone, pigment deposition (lipofuscin) in the cornea, skin pigmentation, pneumonitis, hypoand hyperthyroidism, paresthesia, insomnia, etc. are also possible.
The most common variants of the arrhythmogenic action of antiarrhythmics are dysfunction of the SU and conduction up to asystole, an increase in the Q-T interval and life-threatening ventricular tachyarrhythmias (polymorphic ventricular tachycardia, ventricular fibrillation).
243

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
It should be noted that there are a number of drugs that have remained outside the EM Vaughan Williams classification, but are used as antiarrhythmics for the treatment of rhythm and conduction disorders of the heart. The main ones have already been repeatedly mentioned above.
These are potassium and magnesium preparations, cardiac glycosides, ATP and atropine.
Of the cardiac glycosides, digoxin is commonly used. It is used to control Heart rate in persistent and chronic AF, continuously recurrent or chronic atrial tachycardia, usually in patients with chronic heart failure.
ATP, as a drug that blocks AV conduction, is the drug of choice for AV reentry tachycardia, for the relief of which it is administered as a bolus at a dose of 10–20 mg (maximum 30 mg).
Atropine, which is a racemic mixture of active levorotatory and
inactive dextrorotatory isomer of hyoscyamine, used to increase the rhythm during
dysfunction of the SU and proximal AV blockades, for which, in urgent situations, it is administered intravenously by stream or drip. Preparations containing belladonna alkaloids, belloid, bellataminal, etc., which are also capable of increasing HR, are almost never used at present, since pacemakers are implanted in patients with symptomatic bradycardia.
Non-pharmacological treatment of arrhythmias. catheter methods. A radical change in approaches to the treatment of tachyarrhythmias occurred after the development of catheter methods of treatment. The development of the IVKD technique has led to a revolution in surgical
arrhythmology. In combination with the development of 3D non-fluoroscopic mapping techniques, catheter methods are leading in the treatment of most supraventricular and many ventricular
tachyarrhythmias. Operations for supraventricular tachyarrhythmias account for more than 90% of all catheter procedures currently. Along with ICHKD, in recent years, it has been used
and cryoablation.
The most common forms of reciprocal supraventricular tachycardia
are paroxysmal reciprocal AV tachycardia involving an extranodal abnormal pathway and paroxysmal reciprocal AV nodal tachycardia due to
dissociation of the AV node into fast and slow parts. In ventricular preexcitation syndrome (WPW), the target of the catheter is Kent'sbundle. The complexity and efficiency of the operation depends on the location and structural features of the accessory AV junction. The level of connection of the atria and ventricles varies from subendocardium to subepicardium,
including options for combining pre-excitation syndrome and anomalies in the structure of the coronary sinus. The efficiency of operations to eliminate abnormal conduction reaches 95% and
more.
With functional and anatomical division of the AV node into "slow" and "fast" pathways, selective destruction is oriented towards its slow part. Efficiency
interventions - more than 95%, the risk of iatrogenic AV block - less than 1%. Substrate elimination tachycardia with anomalies of the conduction system of the heart leads to complete recovery.
Significant progress has been made in recent years in the catheter treatment of
supraventricular tachyarrhythmias not associated with anomalies of the cardiac conduction system: automatic and reentry of atrial tachycardias, AF, and atrial flutter.
Until recently, in the overwhelming majority of cases, catheter treatment of AF was palliative in nature and was reduced to the creation of a complete AV block followed by implantation of a pacemaker: a dual-chamber rate-adaptive pacemaker for paroxysmal and persistent AF, single-chamber (for ventricular stimulation) frequency-adaptive - in chronic AF.
However, catheter operations are now increasingly used to isolate trigger zones.
activity in the area of the pulmonary veins and modification of the substrate of the left (and right) atria. With focal or reentry atrial tachycardias, the point of application of ICHKD is a zone of abnormal automatism, trigger activity or reentry around anatomical or functional
244

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
rational barriers. Highly effective is ICHKD of the zone of the cavotricuspid isthmus in right atrial flutter.
IVKD in paroxysmal ventricular tachyarrhythmias is used significantly
less often. This is due to the insufficiently high efficiency of the technique in ventricular arrhythmias
against the background of structural changes in the heart, especially coronary artery disease, chronic heart failure. Prefe
usually given by ICD. The same applies to arrhythmogenic cardiomyopathy of the right ventricle. But in "idiopathic" ventricular tachyarrhythmias in patients without structural changes in
the heart, ICH is often the method of choice. This applies to ventricular tachycardia from the outflow tract of the right (rarely left) ventricle associated with trigger activity or (less often) pathological automatism, as well as the so-called fascicular
left ventricular tachycardia with involvement in the reentry circuit of the bundle branch of His. Implantation of pacemakers. The main reason for pacemaker implantation
(see color incl., fig. 1.38) are bradyarrhythmias due to the presence of dysfunction of the sinus node and / or AV conduction. Detailed indications for the implantation of the pacemaker and antiarrhythmic devices are set out in the relevant Guidelines. In general, the main reason
to the implantation of an artificial pacemaker is the presence of syncope or presin
digging states. However, even in the absence of such a pacemaker, it should be implanted in patients with CVD and chronotropic insufficiency, with stage III AV block. or AV block each II st. Mebits 2 with pauses 8 3 s or replacement rhythm with a frequency of < 40 in 1 min, s Frederick'ssyndrome and pauses 8 5cidr.
All modern EKS operate in demand mode (on demand), i.e., they turn on
only when needed. The pacemaker can be single chamber (atrial or ventricular) or dual chamber (atrial and ventricular). In addition, stimulants can
be frequency adaptive, i.e., change the frequency of stimulation depending on the physiological needs of the patient. There are also more complex functions of stimulants, for example, the function of preventing (treatment) of AF paroxysms, antitachycardia function
(stopping of AF and other supraventricular tachyarrhythmias), etc. Implantable cardioverter-defibrillators. Automatic ICD (see col.
on, fig. 1.39) is a multi-programmable device capable of recognizing
ventricular tachycardia and ventricular fibrillation and having the ability to perform high-energy defibrillation and relief of ventricular tachycardia
antitachycardic (frequent) electrical stimulation. In addition, any ICD is at the same time a pacemaker: single-chamber, two-chamber, or even three-chamber.
Traditional absolute indications for the use of ICD are: ventricular tachyarrhythmia, which was at least once the cause of circulatory arrest;
spontaneous or induced during the EF study sustained ventricular tachycardia or ventricular fibrillation in patients with structural changes in the heart (CHD,
chronic heart failure, arrhythmogenic cardiomyopathy of the right ventricle, etc.). Life-threatening ventricular
arrhythmias in some patients without structural changes in the heart (long Q-T interval syndrome, Brugada syndrome, etc.) are also indications for ICD. Patients with low ejection fraction - less than 30 - 35% (left ventricular dysfunction and chronic HF after myocardial infarction
or due to dilated cardiomyopathy) ICD is indicated even in the absence of ventricular arrhythmias due to the high risk of sudden cardiac death.
Biventricular pacing (cardiac resynchronization therapy). The biventricular pacemaker is indicated for the treatment of patients with drug-resistant clinically significant chronic HF with low ejection fraction and
concerns primarily patients with blockade of the conduction of excitation along the leg (usually
left) bundle of His. It is generally accepted that a decrease in the pumping function of the heart in them in a large
degree due to dyssynchrony of contraction of the left and right ventricles of the heart. Arrange
245

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
The thread of this dyssynchrony is called biventricular EX. Resynchronization of the ventricles is achieved by simultaneously applying an electrical stimulus to both ventricles.
heart with special electrodes.
Biventricular pacemakers can be three-chamber (with the function of atrial stimulation, including for the relief of AF paroxysms). In addition, modern devices
the function of a biventricular pacemaker can be combined with the function of a cardioverterdefibrillator, since it is in patients with severe CHF that the risk of life-threatening
ventricular arrhythmias are particularly high.
Surgical methods. The value of open-heart surgery under cardiopulmonary bypass for the treatment of arrhythmias has been largely lost with the development
catheter technologies. Only a small number of patients with a subepicardial location of the arrhythmogenic substrate can be operated on in this way or using thoracoscopic techniques. The relevance of "large" operations is preserved in those
cases when, in order to eliminate ventricular tachycardia that occurs according to the rien
three mechanism at the border of the contractile myocardium and postinfarction aneurysm of the left ventri the latter is excised. In addition, surgical treatment of AF (operations such as "corridor" or
"Labyrinth") is performed as an addition to the main operation for valve prosthetics heart or repairing an atrial septal defect.
246

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
QUESTIONS
1.For what purpose and in which category of patients is the SCORE scale used?
2.What is the target level of LDL-C for a patient with coronary artery disease without exacerbation.
3.Name the 3 main drugs from the statin class and arrange them in order of
increase in the strength of the hypolipidemic effect.
4. The presence of what factor makes additional cardiovascular risk in patients
AH is very high even with a moderate increase in blood pressure?
5. Specify the target level of blood pressure and the lower limit of safe blood pressure reduction in patients with hypertension.
6.What classes of antihypertensive drugs are absolutely contraindicated in pregnant women?
7.What is the main difference between the conditions for the onset of an angina attack that develops as a result of coronary artery spasm and fixed coronary obstruction?
8.Specify the main biochemical markers of myocardial necrosis.
9.Name the classes of drugs, the use of which can improve
prognosis of patients with stable angina pectoris.
0. List the main electrocardiographic signs of transmural MI in acute phase.
1. Name the drugs that should be used in the treatment of a patient with non-ST elevation acute coronary syndrome as early as possible after the onset of clinical symptoms.
symptoms.
2.What rules should be observed when taking blood samples from a patient with suspicion for acute infective endocarditis?
3.What antibacterial drugs are recommended to start treatment of the patient
with natural valve infective endocarditis?
4.What disease should be suspected in a patient with the following symptoms, appearing 2 weeks after SARS: general malaise, subfebrile temperature
body, shortness of breath, heart failure?
5.In what cases are patients with acute myocarditis prescribed glucocorticoids?
6.Name the early electrocardiographic signs of acute pericarditis.
7.What are the differences between the auscultatory picture of mitral stenosis and mitral insufficiency?
8.List the indications for surgical treatment of a patient with aortic stenosis.
9.List the indications for surgical treatment of a patient with aortic insufficiency.
ness.
10.What medications are used as basic therapy for non-obstructive hypertrophic cardiomyopathy?
11.Indicate the purpose of the appointment and list the indications for the use of indirect antico agulants in patients with dilated cardiomyopathy.
12.Name the main drugs used to stop edema
lung due to acute myocardial infarction.
13.By the value of what physiological indicator can one confidently differentiate What about cardiogenic and hypovolemic shock?
14.What test results can confidently exclude the diagnosis of chronic HF?
15.Which drugs in the absence of contraindications must be prescribed
cheny to a patient with chronic heart failure III f. class?
247

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
16.What classes of drugs can be replaced in case of intolerance to inhibition? ACE tori and ÿ- blockers in the treatment of chronic HF?
17.What part of the conduction system of the heart is called the "His-Purkinje system"? 18. What are the main electrocardiographic manifestations of WPW syndrome? 19. How is it customary to divide atrial fibrillation by duration? 20.
Prevention of what complications is the most important in the treatment of atrial
fibrillation? 21. What heart rhythm disturbances most often cause sudden cardiac death? 22. Which drug class is absolutely indicated for patients with coronary
artery disease and ventricular arrhythmias? 23. What is the main method of treating patients with atrioventricular blockade II -
III degree and syncope (Morgagni-Adams-Stokes syndrome).
248

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
TESTS
Task 1. A 48-year-old man considers himself practically healthy, but knows about a tendency to a moderate increase in blood pressure over the past 3 years (the maximum blood
pressure level is 150/100 mm Hg). During a preventive examination, the following features were revealed:
– height 176 cm, weight 96 kg, waist circumference 95 cm; - smoking about 20 cigarettes a day for 25
years; - pulse 76 beats / min, rhythmic, blood pressure (average of 3 measurements) 148/92 mm Hg. Art.; - a clinical blood test without deviations from the norm; – test for microalbuminuria is negative; – plasma creatinine – 102 µmol/ l; - total cholesterol - 6.0 mmol / l, TG - 2.20 mmol / l, HDL cholesterol -
0.98 mmol / l, LDL cholesterol - 4.02 mmol / l, KA - 5.1; – blood plasma glucose – 5.8 mmol/l; – ECG is a normal variant. – the fundus of the eye without signs of hypertensive
retinopathy. 1. Establish and justify the diagnosis. 2. Assess the risk of adverse cardiovascular events. Task 2. A man, 62 years old, called an ambulance to his house. Complaints of pressing pain in the sternum with irradiation to the left half of the chest
and left arm. The pain appeared 2 hours ago, at about 7 am, immediately after waking up. The pain attack was accompanied by a feeling of severe weakness
and sweating. The patient took validol and analgin, after which the feeling of weakness decreased, but the pain syndrome intensified.
The condition is relatively satisfactory. The skin is pale, moderately moist. Pulse 82 beats / min, rhythmic, blood pressure - 140/90 mm Hg. Art. The limits of relative cardiac
dullness were within the normal range. Breathing is harsh, no wheezing. The liver is not enlarged. The patient has been suffering from hypertension for the past 7 years. The maximum
level of blood pressure is 200/100 mm Hg. Art. Constantly takes enalapril at a dose of 20 mg / day. During therapy, blood pressure is 150 - 160/90 mm Hg. Art.
Never experienced pain in the chest before. Smokes around 10 cigarettes a day for 30 years, does not abuse alcohol. After
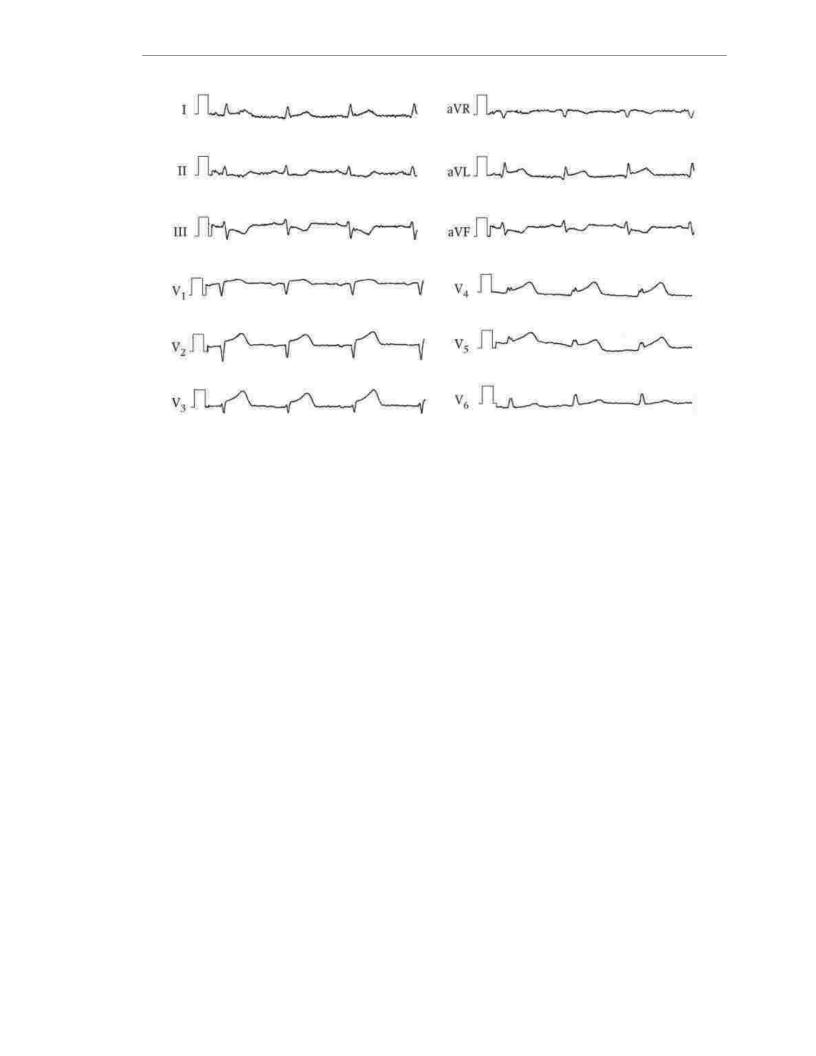
examination, an ECG was recorded.
249
Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
1.Establish and justify the diagnosis.
2.Specify the mandatory drug therapy that should be carried out by an ambulance doctor.
3.Specify the optimal tactics for further treatment of the patient.
Task 3. Woman, 76 years old, hospitalized in a planned manner. Complaints about shortness of breath and palpitations with little physical exertion (moving around the apartment, talking on the phone), increased fatigue, swelling in the legs, worse in the evening.
The patient notes a progressive worsening of the condition during the last month. Moderate condition. The skin is clean, moderate symmetrical edema
on the back of the feet. Pulse 86 beats/min, rhythmic. BP - 140/70 mm Hg. Art. Relative borders heart dullness expanded mainly to the left: to the midclavicular line in the III intercostal space and 2 cm outward from the midclavicular line in the V intercostal space. I tone at the top weakened, accent II tone on the pulmonary artery, weak systolic murmur at the apex and in
the Botkin point. Respiratory rate - 24 per minute. Over the lungs, dullness of the percussion tone is not is determined, breathing is harsh, in the subscapular areas on both sides there are crepitant
rales. The abdomen is enlarged in volume due to the subcutaneous fat layer, not tense. edge liver - 3 cm below the costal arch, soft, painless.
From the anamnesis: hypertension for 20 years with a maximum level of blood pressure 220/110 mmHg Art. At the age of 66 and 72, she suffered 2 myocardial infarctions. After the second myocardial infarction, anginal pain does not bother, blood pressure has stabilized at 130 -
150/70 - 80 mm Hg. Art., but there was shortness of breath on exertion and episodic edema
on foot.
The results of electrocardiographic and echocardiographic studies carried out for 3 months are presented. back. ECG shows sinus rhythm, cicatricial changes in the myocardium of the anterior wall, septum, apex, and lateral wall of the left ventricle ( QS form in leads V1–
V5 ). Echocardiography showed left atrial dilatation and
of the left ventricle, a decrease in the ejection fraction of the left ventricle up to 38%, local contractility disorders of the anterior wall, apex and lateral wall of the left ventricle.
Before admission to the hospital, the patient took nitrosorbide 10 mg 2 times a day.
and hypothiazide 25 mg on an empty stomach every other day. Twice attempts were made to appoint
250
