
1-280 pdf (1)
.pdf
Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
With latent WPW syndrome along the Kent bundle, only retrograde conduction of
excitation from the ventricles to the atria is possible, therefore, the appearance of characteristic signs pre-excitation with this type of WPW syndrome is impossible. The presence of a hidden
WPW syndrome manifests itself when orthodromic reciprocal AV tachycardia occurs, when excitation from the atria to the ventricles propagates along the AV junction, and retrogradely along the Kent bundle.
Patients with WPW syndrome may have several abnormal conduction pathways and, accordingly, several orthodromic tachycardias or orthoand antidromic
tachycardia.
The so-called vagal
techniques (deep breath with breath holding, massage of the carotid sinus, pressure on eyeballs, straining, artificially induced vomiting, etc.). If they don'thelp
SR can be restored medically. Bolus intravenous administration of ATP 10-20 mg is optimal (about 98% efficiency). It is strictly contraindicated
the introduction of verapamil and cardiac glycosides. Tachycardia can also be stopped
with a transesophageal pacemaker in almost 100% of cases, but there is a risk of AF provocation. with anterograde conduction of excitation along the Kent bundle and very high (up to 300 per 1 min.
and more) the frequency of contractions of the ventricles.
To prevent paroxysms, antiarrhythmic therapy has practically not been used recently, since the effectiveness of ICHKD in this type of arrhythmia is 95 -
98%. The presence of AF is an absolute indication for ICHD due to high heart rate and
the likelihood of transformation into ventricular fibrillation. HFKD for people of extreme professions (pilots, climbers, parachutists, athletes of other "specializations", rescuers, etc.)
carried out even in the absence of tachyarrhythmias (with the WPW phenomenon).
Paroxysmal reciprocal
atrioventricular nodal tachycardia
Paroxysmal reciprocal AV nodal tachycardia is one of the most common supraventricular tachycardia. This tachycardia is caused by
functional separation, dissociation of the AV node into zones with fast and slow
conduction of excitation. These zones are located in the upper part of the AV node and differ not only speeds of conduction, but also refractoriness: near the zone of rapid conduction of excitation
it is greater than that of the slow one. Paroxysmal reciprocal AV nodal tachycardia is initiated by atrial extrasystole. Due to the refractoriness of the fast conduction zone, excitation reaches the ventricles through the slow conduction zone. By the time it
reaches the lower part of the AV node, the refractoriness of the fast conduction zone ends, which makes retrograde conduction of excitation to the atria possible and closes the circuit reentry. Thus, for the initiation of tachycardia, it is necessary that the refractoriness and speed of excitation conduction along the fast and slow parts of the AV node differ.
Difficulties in the diagnosis of paroxysmal reciprocal AV nodal tachycardia can
be associated with the abundance of her ECG manifestations. In particular, it is the only AV reciprocal tachycardia, in which excitation to the ventricles can be carried out not only with a
multiplicity of 1: 1, but also 2: 1 (blockade occurs below the reentry chain, in the trunk of the bundle of His)
against the background of tachycardia, ventricular extrasystoles may appear. With various
variants of the WPW syndrome, neither one nor the other is possible: and the blockade of the conduction of excit any part of the AV junction and a ventricular extrasystole will immediately interrupt the
tachycardia. Finally, there is an atypical course of reciprocal AV nodal tachycardia with reverse (“antidromic”) movement of excitation in the reentry loop. In this case, retrograde
211

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
on the atrium, P waves will not be recorded immediately after the QRS complex, but immediately before it. Such atypical tachycardia is called "fast-slow" (fast-slow).
It is more common in children, can be continuously relapsing.
Therapeutic tactics for paroxysmal reciprocal AV nodal tachycardia are few differs from the tactics of treating patients with various variants of the WPW syndrome.
Tachycardia is stopped by vagal techniques. Highly effective intravenous administration of ATP. The use of verapamil, ÿ- blockers and novocainamide to restore CR is possible,
but less effective and safer. Radical treatment - ICHKD. FP is less dangerous.
Atrial fibrillation
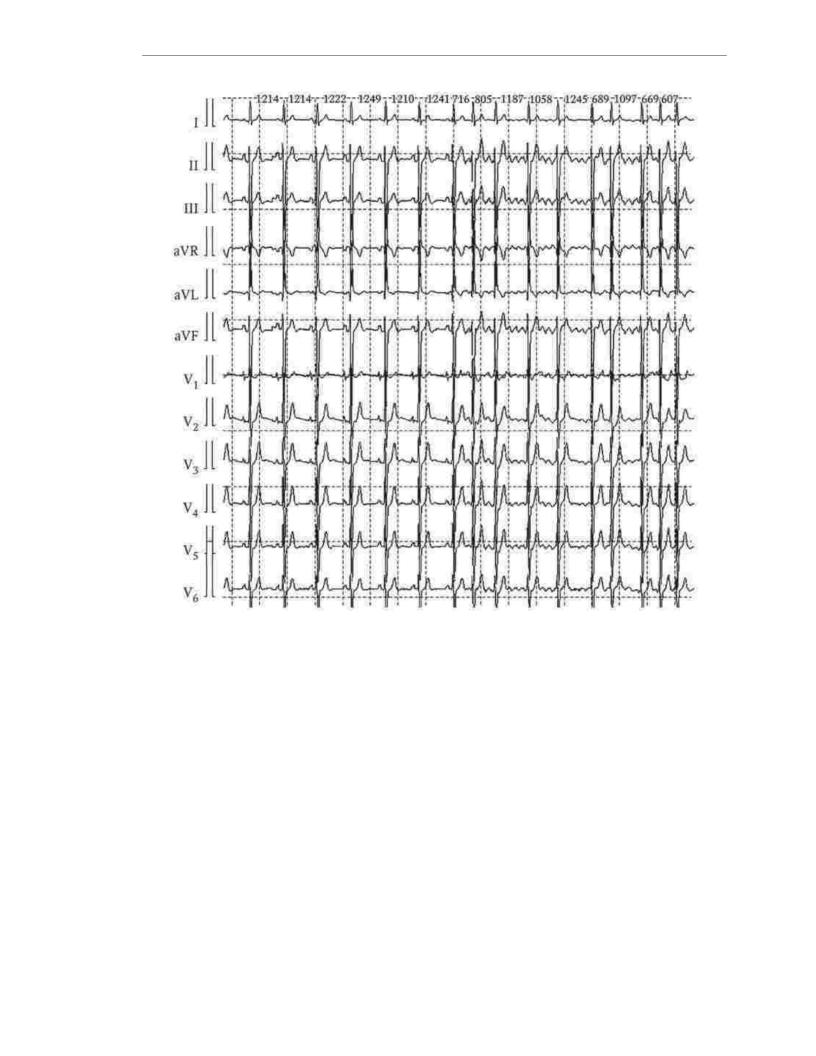
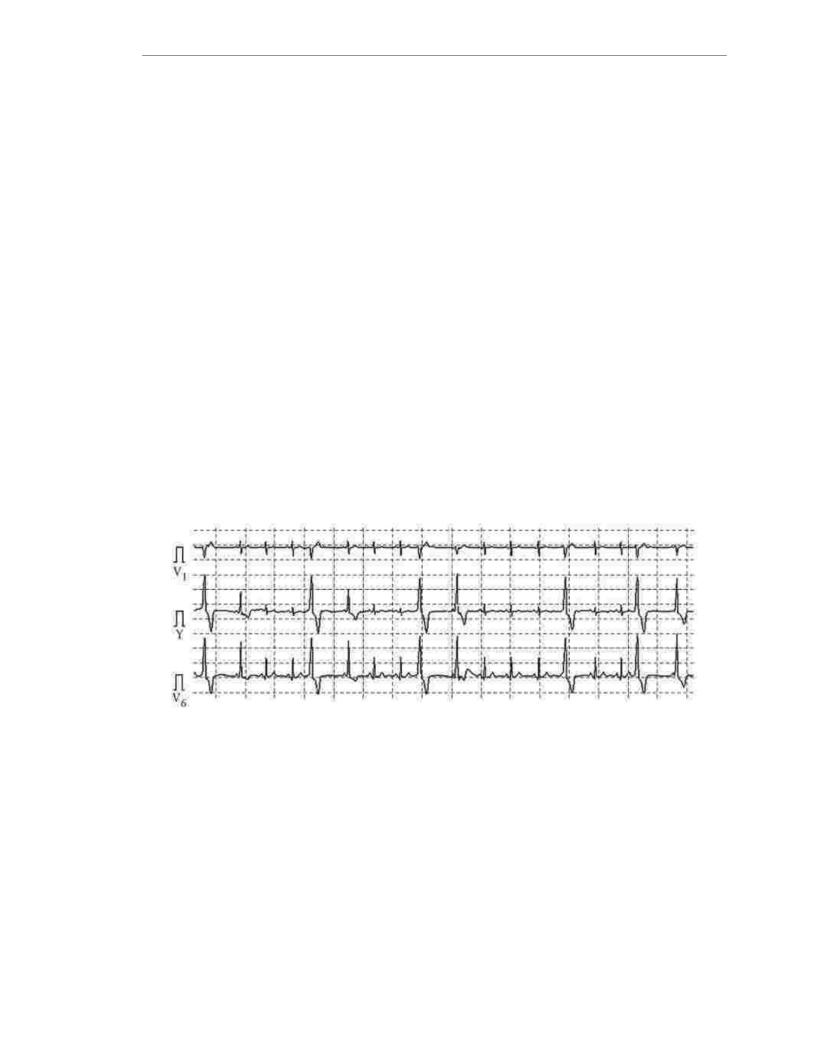
AF is the most common of all supraventricular tachyarrhythmias, characterized by uncoordinated atrial electrical activity with subsequent deterioration of their contractile function. On the ECG during AF, one can see fibrillation waves f, which are frequent oscillations of various sizes and unequal shapes in combination
with non-rhythmic contractions of the ventricles (Fig. 1.23). Isolate bradysystolic AF (ventricular rate less than 60 beats per minute), normosystolic (from 60 to 100 beats) 1 min) and tachysystolic (more than 100 in 1 min).
The causes of AF are divided into cardiac and non-cardiac. Most
frequent cardiac causes are hypertension, ischemic heart disease, valvular heart disease.
Less often - pericarditis, heart tumors, SSS, dilated and hypertrophic cardiomyopathy. From non-cardiac causes, it is necessary to single out pulmonary (chronic obstructive pulmonary disease,
pneumonia, thromboembolism of the branches of the pulmonary artery), metabolic (thyrotoxicosis) and toxic. The most common among the latter is AF at the height of
alcohol intoxication (holiday heart syndrome). In addition, idiopathic AF is distinguished in patients with structural heart disease.
212
Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
Rice. 1.23. Paroxysm of atrial fibrillation
In accordance with the modern classification, paroxysmal AF is distinguished (duration does not exceed 7 days, more often - no more than 48 hours), persistent (duration of more than 7 days), long-term persistent (duration of more than 1 years) and permanent (chronic, permanent). A FP is called constant, at which
It was decided not to restore the SR, or it cannot be done. If the patient has had 2 or more attack, AF can be called recurrent. In paroxysmal AF, SR is usually
recovers on its own, with persistent it rarely happens.
The prevalence of AF is 0.4% of the general population, in people over 60 years of age it occurs in 6% of cases. Population studies show that with
AF mortality increases by 2 times or more. Its main causes are thromboembolic complications, progression of CHF and the initiation of life-threatening ventricular
arrhythmias.
AF is most often triggered by focal impulses from the orifices of the pulmonary veins. The mechanism for maintaining AF is multiple microreentry loops in the atria.
The main complaints of patients with AF are palpitations, shortness of breath, weakness, increased fatigue, pain in the chest area like cardialgia (sometimes angina pectoris), dizziness. Syncope (presyncope) conditions are rarely noted.
213

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
There are 2 clinical variants of AF: vago-dependent and sympathetic-dependent. The rather rare vagodependent AF is typical for young and middle-aged men.
age without structural changes in the heart, occurs at rest (in the evening or at night), on the background of sinus bradycardia. It can be triggered by overeating or
alcohol, responds poorly to AARP treatment. Sympathetic-dependent AF occurs more often in
patients of any gender and age with structural changes in the heart, in the daytime, against the background of sinus tachycardia (provoked by physical or emotional stress). Antiarrhythmic therapy in this
variant of AF is more effective.
In the treatment of a patient with AF, the main problems are the following: thromboembolic complications (primarily ischemic stroke) due to the presence of
blood clots in the left atrial appendage; urgent hospitalizations associated with the deterioration of the patient'scondition; the need for many patients to take oral anticoagulants;
the appearance and progression of CHF due to a violation of atrioventricular synchronization,
loss of atrial "contribution" and an increase in heart chambers against the background of high heart rate; chronic disease with a decrease in the quality of life.
In the antiarrhythmic treatment of patients with AF, it is advisable to adhere to the following algorithm. The first (newly detected) paroxysm of AF is stopped spontaneously, using pharmacological or electrical cardioversion. Antiarrhythmic therapy is not
is prescribed because it is difficult to assess the likelihood of AF recurrence. In case of recurrent paroxysms of atrial fibrillation, occurring less frequently than once every 3 months, accompanied
by clinical symptoms, attacks are stopped, but permanent antiarrhythmic therapy is not prescribed. If a attacks are asymptomatic, then the heart rate is controlled (normalized). With more frequent paroxysms of AF, accompanied by clinical symptoms, permanent antirhythmic therapy is
prescribed. With asymptomatic paroxysms, heart rate control is necessary. Finally, if antiarrhythmic therapy is ineffective or ineffective (1 - 3 antiarrhythmics),
non-drug treatment is prescribed (IPKD - isolation of the orifices of the pulmonary veins) or the heart rate is controlled. In patients with minimal or no structural changes in the heart, nonpharmacological treatment may, with their consent, become a priority (without
attempts at antiarrhythmic therapy).
SR should be immediately restored in paroxysmal AF with a high ventricular rate due to acute MI, hypotension, angina pectoris or HF, as well as in
severe intolerable symptoms. Restoration of SR was also shown for the first time identified AF, persistent AF with low chance of early recurrence, with relapse
AF in patients who have not previously taken AARP. Cardioversion is not indicated for patients with frequent
transitions from SR to AF and vice versa, as well as in cases where patients receiving AAP,
repeated attempts at cardioversion have already been made.
Propafenone is the drug of choice for medical recovery of SR (pharmacological cardioversion) in paroxysmal AF in patients with minimal or no structural changes in the heart. It can be given as a single oral
at a dose of 450 - 600 mg (3 - 4 tablets). With proven safety of the drug (first dose
in a hospital setting!) the patient can stop the attacks on his own if he does not receive constant antiarrhythmic therapy. It is possible to restore CP with intravenous administration of propafenone (2 mg/kg for 10 minutes), amiodarone (5 mg/kg for
1 hour) and procainamide (usually 500-1000 mg). In paroxysmal AF against the background of structural changes in the heart, as well as in persistent AF, amiodarone and -
only in the intensive care unit - nibentan (0.125 - 0.25 mg / kg).
It should be emphasized that digoxin, sotalol, ÿ- blockers (propranolol) and calcium antagonists (verapamil) do not have a stopping effect in AF.
214

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
Electrical cardioversion is also used to restore HR in AF, especially in unstable hemodynamics. It is performed on an empty stomach under general anesthesia. short acting drugs. The electrical discharge must be synchronized with
QRS complex. The energy intensity of the first shock is usually 200 J, the second and third shocks (with an interval of at least 1 min) are 300 and 400 J, respectively. The
efficiency of electrical cardioversion is inversely proportional to the duration of AF. It also decreases with obesity, chronic pulmonary pathology, large (more than 45 - 50 mm) sizes of the left
atrium. The defibrillation threshold is increased when taking AARP.
Both electrical and pharmacological cardioversion must be preceded oral anticoagulants (warfarin, dabigatran etexilate, rivaroxaban,
apixaban) in the event that the duration of AF exceeds 48 hours, and the absence of blood clots in the left atrial appendage is not proven by the data of the thoracic water
echocardiography. The duration of their reception is 3 weeks. When prescribing warfarin, the INR by the time be around 2.0. After cardioversion, oral anticoagulants should be continued for another
4 weeks. In the presence of thrombi in the left atrium, a 6-week oral anticoagulants followed by transesophageal monitoring
echocardiography. In case of urgent indications for cardioversion, the patient is preliminarily injected with direct anticoagulants: heparin, fraxiparin, enoxaparin.
Contraindications to cardioversion in AF are atrial thrombi (according to transesophageal echocardiography), hyperthyroidism, digitalis intoxication, acute infectious or inflammatory diseases, decompensated chronic heart failure.
Protective (preventing AF paroxysms) therapy is not an easy task. In chronic HF, only amiodarone can be prescribed. Start with IHD
treatment is possible with ÿ- blockers, but their protective efficacy is low. The recommended AAPs are dronedarone (with caution) and sotalol. If they fail, amiodarone
may be prescribed. The tactics of treating patients with hypertension depends on the presence of left ventricular hypertrophy. With existing hypertrophy, dronedron can be prescribed
(with caution), with inefficiency - amiodarone.
In the absence of structural changes in the heart and in AH without left ventricular hypertrophy, antiarrhythmic therapy can be considered much safer, since the likelihood of arrhythmogenic effects of drugs is much less. As a first line
treatment for this group of patients are recommended allapinin, dronedarone, propafenone, sotalol, etatsizin, etmozin; the second line is amiodarone.
It should be noted that for primary and secondary prevention of AF paroxysms (primarily in patients with structural changes in the heart) in recent years, nonantiarrhythmic drugs that have proven their effectiveness have also been used: inhibitors ACE, angiotensin II receptor blockers, statins. Treatment with these drugs has been
the name of upstream therapy.
In addition to pharmacological prevention of AF attacks, there are nonpharmacological methods of treatment. Pulmonary vein isolation is currently the most common and fairly effective non-drug treatment for AF.
(sources of focal impulsation) with the help of VChKD. The success of catheter ablation is inversely related to patient age, left atrial size, incidence, and
FP duration. Thus, the most effective non-drug treatment
is in patients with idiopathic AF or minimal structural changes hearts.
An alternative to HR preservation is heart rate control. A number of multicentre studies have shown that SR preservation has no significant benefit.
before heart rate control, at least for people over 65 years of age. In the absence of expression
215

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
symptoms of AF, less strict control of heart rate is carried out: heart rate is considered acceptable at rest within 110 in 1 min. In the presence of severe symptoms of AF, more
tight control: heart rate at rest 60 - 80 per 1 min, with physical activity - 90 - 140 per 1 min. To control heart rate, it is customary to use 3 groups of drugs: ÿ- blockers,
calcium antagonists (verapamil, diltiazem) and cardiac glycosides (digoxin). ÿ- blockers are the drugs of choice. Common (especially for the treatment of patients with CHF) is their combination with digoxin. Holter monitoring is the optimal method for monitoring the effectiveness and safety of therapy. Exactly the same
This is how heart rate is controlled in chronic AF.
In those rare cases when it is not possible to achieve correction of heart rate in AF with drugs, perform IVKD of the AV node, after which the pacemaker is implanted. Stimulation
in paroxysmal and persistent AF should be two-chamber, in chronic AF - ventricular, but necessarily rate-adaptive (see below).
The most important in the treatment of AF is antithrombotic therapy, for which antiplatelet agents (aspirin, clopidogrel) have practically ceased to be used.
The main group of drugs for the prevention of systemic thromboembolism and ischemic strokes are oral anticoagulants (apixaban, dabigatran etexilate, warfarin, rivaroxaban). The dose of warfarin is selected under the control of the INR, which should, as
as a rule, be in the range from 2.0 to 3.0 (in the presence of a mechanical valve prosthesis -
2.5 - 3.5). The nature of antithrombotic therapy is selected in accordance with the presence and the nature of risk factors for thromboembolic complications in accordance with the special CHA2DS2 -VASc scale. According to this scale, two risk factors are estimated at 2 points: previous stroke/transient ischemic attack and age 8–75 years. Other factors
risks are worth one point each. The maximum score on this scale is 9.
but already in the presence of 2, the appointment of oral anticoagulants is mandatory. If available 1 score, it is possible to prescribe antiplatelet agents (aspirin 75–325 mg / day) or oral anticoagulants, but preference should be given to the latter. In the absence of risk factors
it is possible to prescribe antiplatelet agents, but it is better to do without them. If there are contraindications to taking oral anticoagulants (high creatinine level, severe
anemia, etc.) it is possible to take a combination of aspirin 100 mg/day and clopidogrel 75 mg/day.
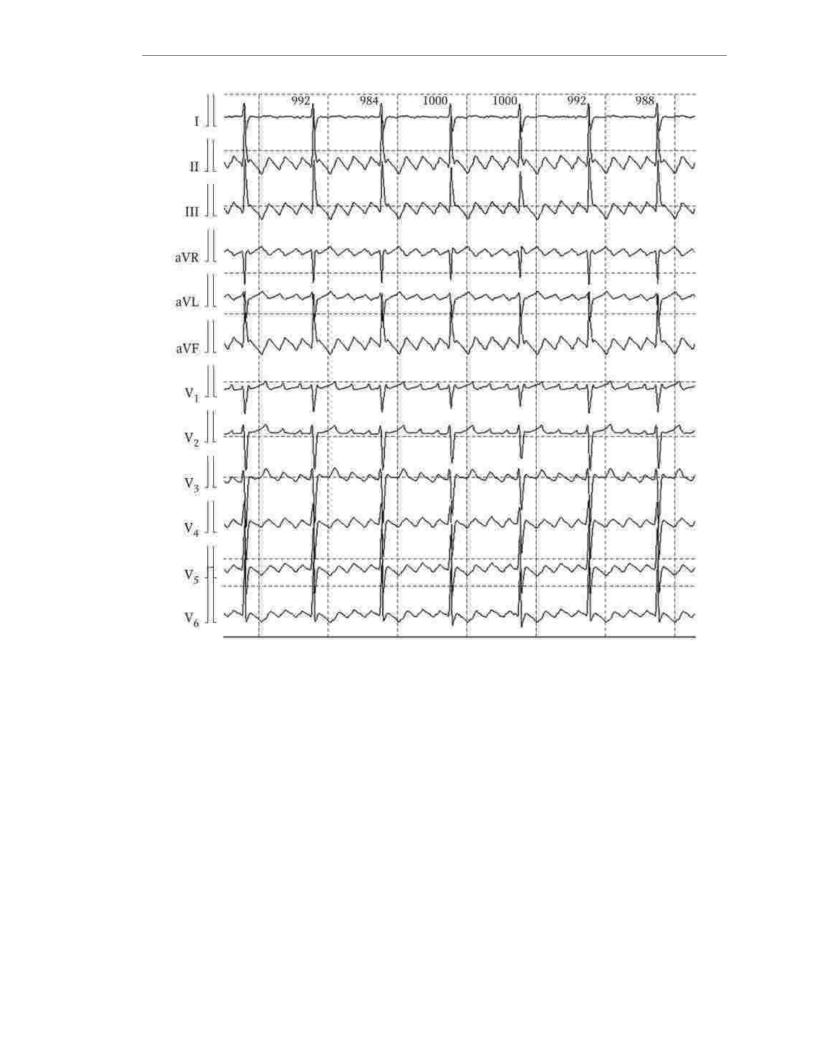
atrial flutter
Atrial flutter is often the patient'sonly tachyarrhythmia, but often combined with FP. The main mechanism for the occurrence of atrial flutter is reentry around large anatomical structures in the right or left atrium. Frequency atrial contraction is less than with AF, and is 250 - 400 per 1 min. Wherein
on the ventricles, excitation is usually carried out with a multiplicity of 2: 1 or more, often irregularly. Like AF, atrial flutter can be paroxysmal, persistent, and
chronic. A common variant of atrial flutter is right atrial (Fig. 1.24), which is called typical. Its fundamental difference is
the fact that excitation necessarily spreads through the so-called cavotricuspid isthmus (between the superior vena cava and the annulus of the tricuspid valve). On the ECG at right atrial flutter, sawtooth waves F are visible without an isoline between
them with maximum amplitude in leads II, III and aVF. Optimal (radical)
The treatment for right atrial flutter is ICP in the cavotricuspid isthmus zone. All other variants of atrial flutter are usually left atrial and
called atypical. The tactics of their treatment does not differ from that in AF.
216
Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
Rice. 1.24. Atrial flutter (right atrial) with 4:1 AV conduction
The risk of thromboembolic complications in atrial flutter is somewhat less, than with AF, but the prevention is the same.
1.12.4. Ventricular arrhythmias
The most important ventricular arrhythmias are ventricular extrasystole,
ventricular tachycardia, flutter and ventricular fibrillation. Mechanisms for the formation of ventricular arrhythmias can be pathological automatism (rarely), trigger
activity and re-entry of the reentry excitation wave. In addition, the causes of ventricular arrhythmias can be combined. Most often from the ventricles
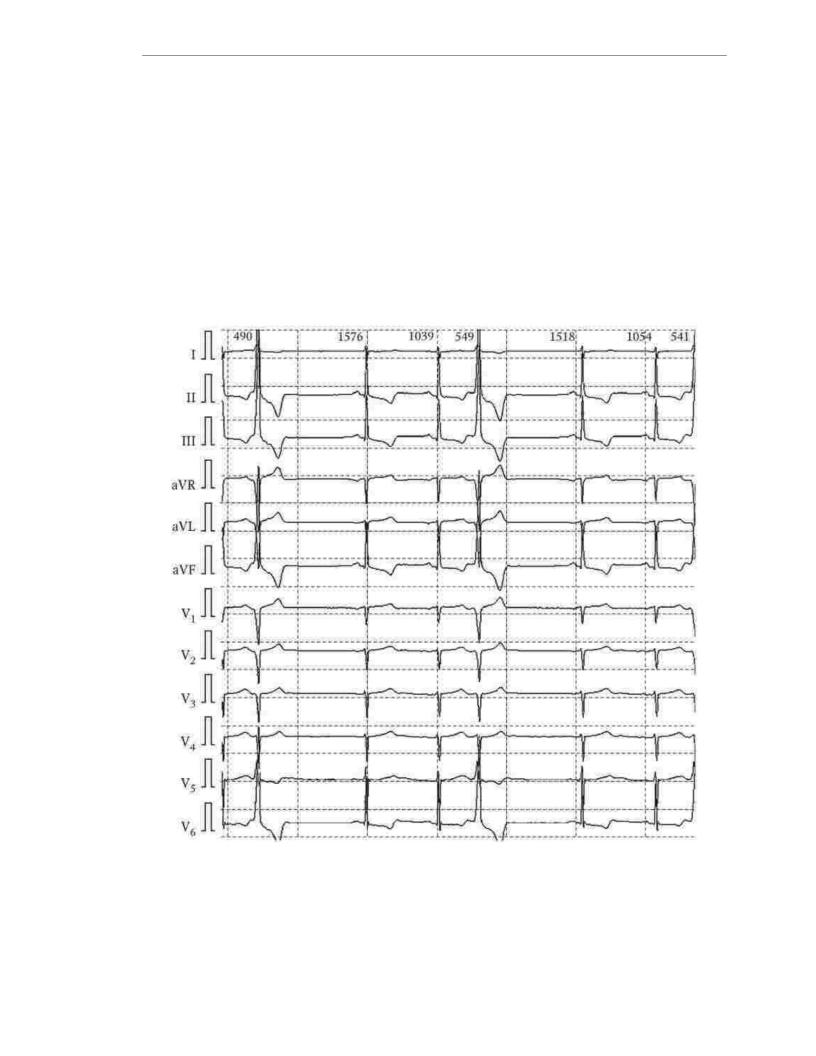
arrhythmias occur extrasystole. Ventricular extrasystole is called premature contraction, the source of which is located below the trunk of the bundle of His (pedicles of the bundle of His, Purkinje fibers, contractile myocardium of the ventricles). The main distinguishing features of ventricular extrasystole are a wide deformed QRS complex.
and the absence of a P-tooth (Fig. 1.25).
217
Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
Unlike atrial extrasystole, with ventricular compensatory pause
usually complete (the interval from the QRS complex before the extrasystole to the QRS complex following the extrasystole is approximately equal to the two R-R intervals
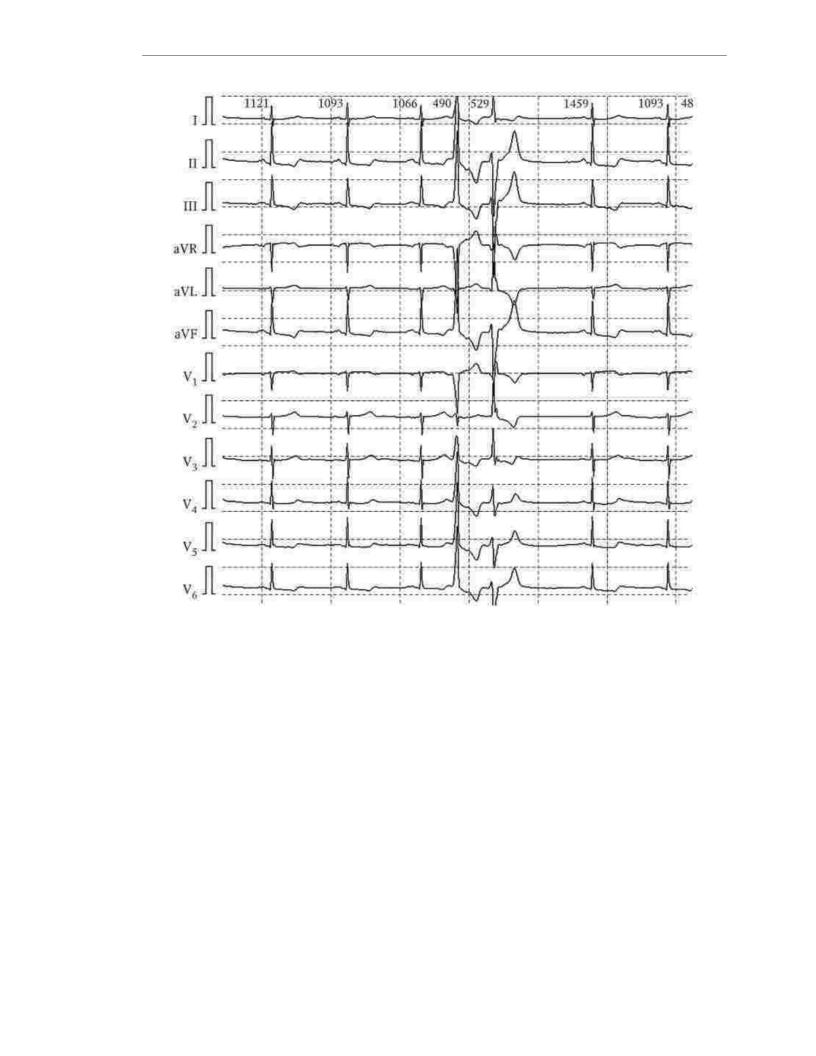
preceding the extrasystole). It is customary to single out single and pair (2 in a row) extrasystole (Fig It can be monotopic (from the same source, identical in form) and polytopic (from
different sources, different in form). At the same time, the coupling interval (the
distance between the extrasystolic QRS complex and the preceding QRS complex) with monotopic extrasystole is approximately the same, with polytopic - different. If the clutch interval
an extrasystole so short that it overlaps with the T wave of the previous QRS complex, it is called early, or "R on T". Under conditions of electrical instability
myocardium (for example, acute coronary syndrome, acute myocardial infarction), it is early extrasystole that triggers life-threatening ventricular arrhythmias.
Rice. 1.25. Ventricular extrasystole
218
Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
Rice. 1.26. Pair polymorphic ventricular extrasystole
In some cases, extrasystoles periodically occur after each sinus
contraction (bigeminy), two (trigeminy) or three (quadrigeminy) sinus contractions. The common name for such extrasystole is allorhythmia.
Sometimes the source of ventricular extrasystole is protected from external influences, in first of all SR, the so-called blockade of the entrance and generates impulses with its own
frequency. Obviously, in the absence of blockade of the entrance, it would be suppressed by more frequent SR.
Such an extrasystole is called parasystole, and its source is a paracenter. It is a competitive pacemaker and causes depolarization of the ventricles when they are not in
state of refractoriness after depolarization from sinus excitation. Classic signs of parasystole are the following: identical in morphology, ventricular
complexes arise with different intervals of adhesion; spacing between two adjacent
parasystoles are characterized by a multiplicity (common divisor), reflecting the frequency of impulses from the paracenter; there are drain complexes arising from the simultaneous depolarization emanating from the SU and the paracenter (Fig. 1.27). Self Clinical
parasystole does not matter, its treatment corresponds to the treatment of ventricular extrasystole
century.
Three or more premature contractions in a row are called ventricular tachycardia. In this case, the heart rate should be 100 in 1 min or more. Ventricular tachycardia continued
219
Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
with a life of up to 30 s is called unstable, from 30 or more - paroxysmal. Allocate monomorphic (Fig. 1.28) and polymorphic (Fig. 1.29) ventricular tachycardia. Polymorphic ventricular tachycardia can also be bidirectional and spindle-shaped (such as
"pirouette", torsade de pointes). Tachycardia with a heart rate of 250 - 300 in 1 min is called flutter
ventricles, but uncoordinated asynchronous contractions of individual myocardial fibers
or their groups with the cessation of systole - ventricular fibrillation (Fig. 1.30). Ventricular tachycardia, ventricular flutter and ventricular fibrillation are called life-
threatening arrhythmias. The provoking factor (trigger) for them is
ventricular extrasystole. There is a certain relationship between the nature of extrasystole and the likelihood of life-threatening arrhythmias. In accordance with the clinical and prognostic significance, extrasystoles are divided into gradations. In Russia
the classification proposed by B. Lown and M. Wolf (1971) has become widespread, reflecting an increase in the risk of extrasystoles from the 1st gradation to the 5th:
0 - no ventricular extrasystoles;
1 - 30 or less ventricular extrasystoles in 1 hour;
2 - more than 30 ventricular extrasystoles in 1 hour; 3 - polymorphic ventricular extrasystoles;
4A - paired ventricular extrasystoles;
4B - three in a row or more ventricular extrasystoles (unstable ventricular tachycardia);
5 - ventricular extrasystole type "R to T" (early).
It should be noted that the authors of the classification did not count on its being so broad. distribution, since it was developed in relation to patients in the acute period of MI.
Rice. 1.27. Ventricular parasystole
220
