
1-280 pdf (1)
.pdf
Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
throughout the ascending limb of the loop of Henle. The drugs in this group have the most strong action, increasing diuresis by 100% or more from the original. The effect of loop diuretics persists even in patients with renal insufficiency at a rate of glomerular
filtration less than 5 ml/min. Acetazolamide inhibits the activity of carbonic anhydrase,
as a result, the formation of carbonic acid decreases, tubular reabsorption of bicarbonate and sodium ions is disturbed, and hydrogen ions accumulate. It leads
to a small (by 10-15%) increase in diuresis and a shift in the acid-base state towards acidosis. According to the severity of the diuretic effect under normal conditions
acid-base state, acetazolamide is inferior to loop and thiazide diuretics.
However, with the development of alkalosis, which often develops with prolonged use thiazide and loop diuretics, weakening their effect, the effect of acetazolamide is enhanced. Under these conditions, its addition to diuretics of other pharmacological groups
may significantly enhance the diuretic effect. Competitive aldosterone antagonists
acting on specific receptors located in the distal tubule, prevent the excretion of potassium in the urine. Their effect on sodium reabsorption is negligible, therefore
the diuretic effect is much weaker than the effect of loop and thiazide diuretics.
Diuretic therapy begins only in the presence of symptoms of congestion (stage IIA, II functional class of chronic HF) with the use of the weakest drug effective in this patient. Torasemide (2.5-5 mg/day) or hydrochlorothiazide are preferred
(25 mg/day). With their insufficient effectiveness, they switch to the use of loop diuretics - furosemide, ethacrynic acid, bumetanide, torasemide in higher doses.
In the case of decompensation of chronic HF, accompanied by severe edematous syndrome, a combination of thiazide and loop diuretics is used.
Treatment begins with small doses, increasing them to the optimum in the course of therapy. Dehydration therapy in chronic HF includes two phases: active and maintenance. In the active phase, the task of which is to remove excess fluid accumulated in the body, the excess
diuresis over the drunk fluid should be 1–2 l / day, and
weight loss of about 1 kg / day. After reaching optimal dehydration, they move on to the maintenance phase of treatment, the task of which is to ensure a balanced
diuresis and stable body weight.
An important condition for effective and safe diuretic therapy is the regular daily intake of diuretic drugs in individually selected doses. The use of high doses of diuretics for rapid dehydration and taking drugs once a day
several days are dangerous and unjustified due to the increased risk of electrolyte disturbances, thromboembolism and deterioration in the quality of life of the patient. In
addition, the irregular use of diuretics is an additional factor in the hyperactivation of neurohormones and leads to rebound fluid retention in the body.
Due to the fact that neurohumoral disorders play an important role in the development
of edematous syndrome, it is recommended to combine diuretic therapy with the use of neurohumoral drugs modulators - ACE inhibitors, competitive aldosterone antagonists. The neuromodulatory
effect of spironolactone and eplerenone is manifested when they are used at a dose of 25 - 50 mg/day
In cases of insufficient effectiveness of combination therapy with thiazide, pet
left diuretics and competitive aldosterone antagonists to increase sensation
the patient'ssensitivity to diuretics, it is advisable to supplement the treatment with an inhibitor carbonic anhydrase with acetazolamide (0.25 mg 3 times a day for 3-4 days). A course of treatment acetazolamide is recommended once every 2 to 3 weeks.
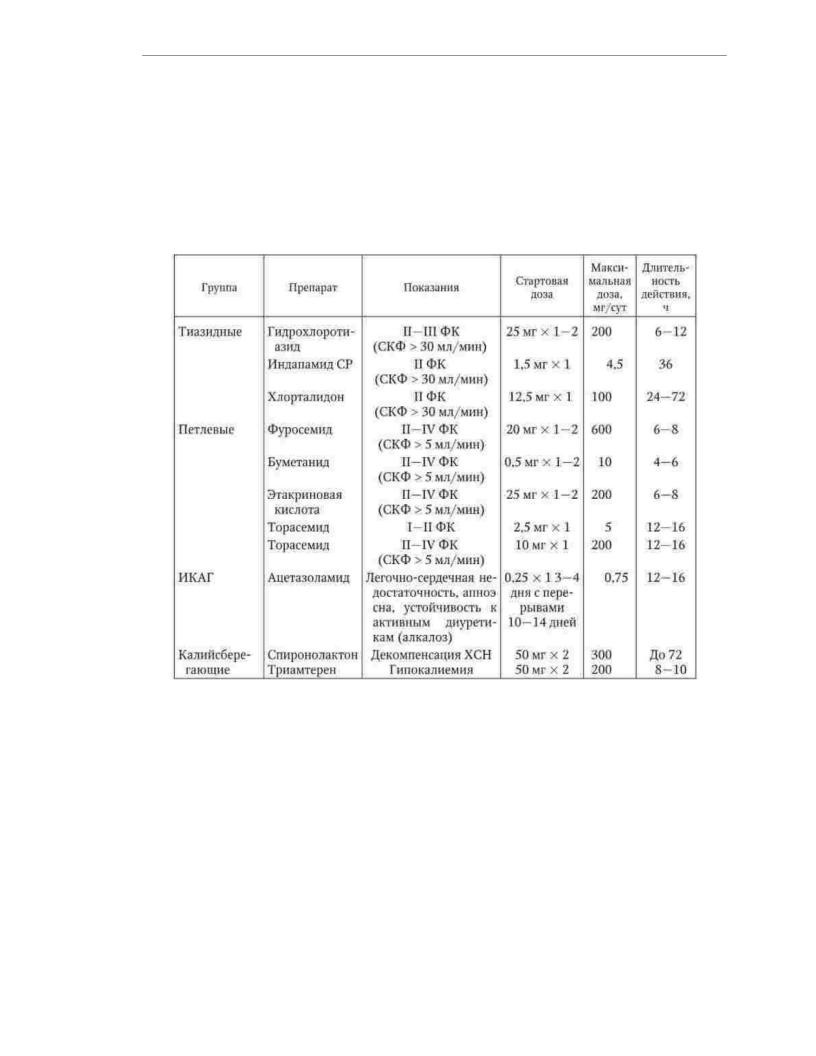
Indications and doses of diuretics for the treatment of patients with chronic HF are presented in tab. 1.34.
191
Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
Cardiac glycosides remain among the main treatments for chronic HF. despite the fact that drugs of this class do not slow the progression of the disease
and do not improve the prognosis of patients. The main effects of cardiac glycosides are to reduce severity of clinical symptoms, improving the quality of life of patients and reducing
need for hospitalizations for decompensation of chronic HF.
Table 1.34
Indications for use, doses and duration of action of diuretics in the treatment of patients with chronic heart failure
By blocking sodium-potassium ATPase, cardiac glycosides prevent ion exchange intracellular sodium to extracellular potassium. As a result, sodium-calcium metabolism is activated and the entry of calcium ions into the cell is enhanced. An increase in the concentration of free calcium in the cytoplasm of cardiomyocytes
leads to an increase in the interaction of contractile proteins and a positive inotropic effect. Over 20 the use of cardiac glycosides, along with the advantages, there were also
disadvantages of drugs of this class, the main of which is a relatively weak inotropic the effect of low and medium doses with a small breadth of therapeutic action. The
special position of cardiac glycosides among inotropic agents is due to the fact that they not only affect myocardial contractility, but also have negative chronotropic and
neuromodulatory effects. Thus, the use of cardiac glycosides for the treatment of patients with chronic HF (in low doses) does not contradict the currently dominant time concept of neurohumoral unloading of the heart.
Digoxin is the only drug from the class of cardiac glycosides recommended for clinical use as part of the complex therapy of chronic HF.
192

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
In the treatment of patients with a combination of chronic heart failure and atrial fibrillation
(especially with tachycardia), digoxin is the basic drug of pharmacotherapy. In patients of this kind, the therapeut digoxin is mainly due to a decrease in heart rate due to a slowdown in AV conduction, and not
its effect on myocardial contractility. Due to the negative chronotropic effect of digoxin in patients with AF, there is a decrease in myocardial demand for
oxygen, which is expressed the more, the higher was the initial heart rate. When saved sinus rhythm digoxin is recommended for use in cases of insufficient effectiveness of ACE inhibitors, ÿ- blockers, aldosterone antagonists and diuretics. To
predictors of success in treating patients with chronic heart failure with digoxin include a low fraction left ventricular ejection (less than 25%), cardiomegaly (cardiothoracic index more
55%) and non-ischemic HF etiology.
The recommended dose of digoxin for patients with chronic heart failure is 0.25 mg/day. In this dose, the drug acts mainly as a neurohumoral modulator, has a weak inotropic effect and does
not stimulate the development of arrhythmias. In patients weighing more than
85 kg, it is possible to use digoxin at a dose of 0.375 mg / day. For elderly and senile patients, the recommended dose of digoxin is 0.125 mg/day. In patients with impaired renal function, the dose of digoxin is selected individually depending on the clearance
creatinine. The combination of digoxin with ÿ- blockers is preferable, since the use of this combination allows better control of heart rate, reduces the risk of life-threatening ventricular arrhythmias and acute coronary insufficiency.
Omega-3 polyunsaturated fatty acids reduce the risk of death and
hospitalization needs of patients with chronic heart failure. These results were obtained in a large study evaluating the clinical efficacy of the drug
omakor, containing highly purified omega-3 polyunsaturated fatty acids. The clinical effect of this drug is associated with a reduced risk of ventricular
heart rhythm disturbances. The recommended dose of Omacor is 1 mg/day against the background of a complete complex therapy for chronic HF.
Complementary medicines. The category of additional drugs includes drugs, the efficacy and safety of which in chronic
SN have been investigated, but require clarification. This group includes statins and anticoagulants. Statins are considered as effective means of preventing the development of chronic HF in
patients with coronary artery disease. In addition, drugs of this class can reduce the number of hospitalizations of patients suffering from chronic heart failure due to coronary artery disease. In the same time The use of statins in already developed chronic HF is not accompanied by improvement
prognosis of patients, regardless of etiology. As part of the complex therapy of patients with chronic HF of ischemic etiology, the use of rosuvastatin at a dose of 10 mg / day is recommended. days at a total cholesterol level of at least 3.2 mmol / l.
Anticoagulants are recommended for use as part of the complex therapy of patients with chronic heart failure who are on bed rest in order to prevent thrombosis and embolism. Low molecular weight heparins (enoxaparin 40 mg/day for 2–3 weeks) are considered the most effective means of solving this problem. Oral
anticoagulants (warfarin, dabigatran etexilate, rivaroxaban, apixaban) should be used in the treatment of patients in whom chronic HF is associated with AF and an increased risk thromboembolism. The factors of increased risk of thromboembolism include: advanced age, a history of thromboembolism, a stroke or transient cerebrovascular accident, the presence of an intracardiac thrombus, a sharp decrease in the fraction
ejection (less than 35%) or dilatation of the left ventricle of the heart (end-diastolic size more than 6.5 cm), undergone heart surgery.
193
Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
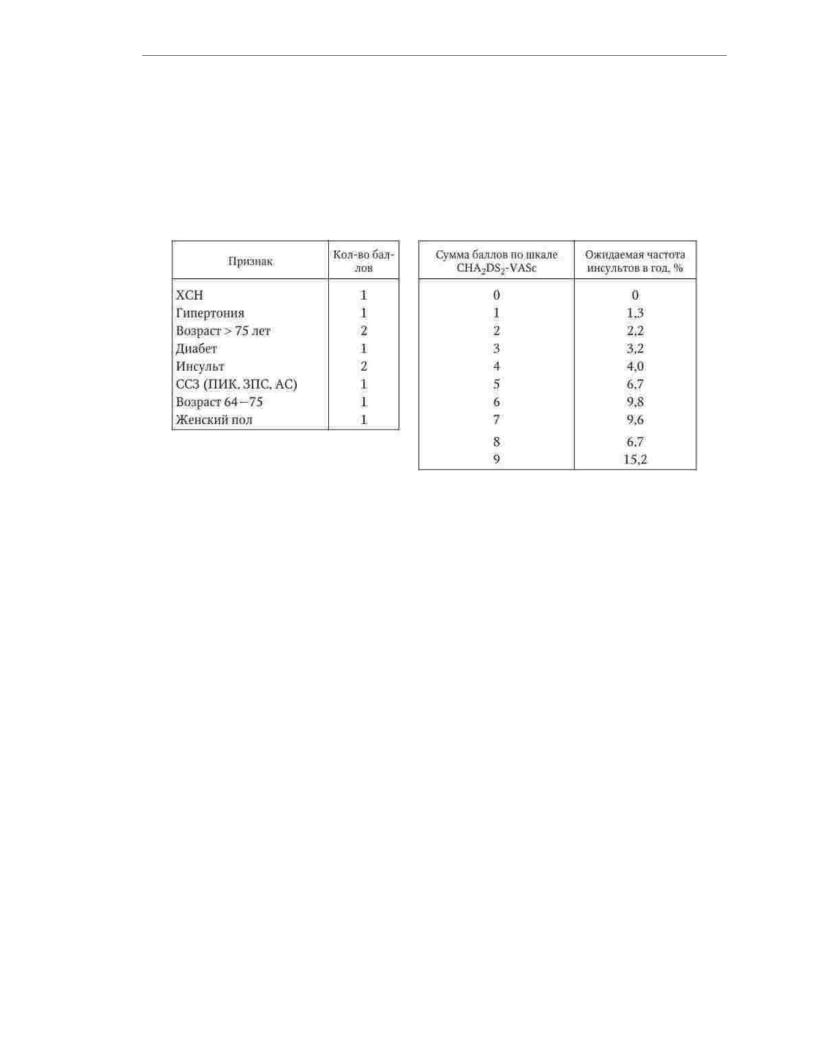
To calculate the risk of stroke in patients with AF, it is recommended to use a scale
CHA2DS2-VASc, whose name is an English abbreviation for factors
risk of thromboembolism (stroke / transient ischemic attack / systemic thromboembolism history, chronic heart failure, hypertension, age 75 years, diabetes mellitus, vascular disease, age 65 - 74 years and female) (Table 1.35).
Table 1.35
Calculation of stroke risk in patients with AF using the CHA2DS2-VASc scale
For patients with a risk of more than 1 point, the use of oral anticoagulants is considered preferable, and for patients with a risk of 2 points or more, it is mandatory.
The individual bleeding risk can be assessed using the HAS-BLED scale (Table 1.36). The risk is conside the score on this scale is 3 or more. A high risk of bleeding does not rule out
the use of anticoagulants, but the dose of the prescribed drug should be reduced.
To achieve acceptable efficacy of warfarin treatment, the international normalized ratio (INR) during therapy should be maintained at
level 2.0 - 3.0. The use of new oral anticoagulants - dabigatran etexilate
at a dose of 110 mg 2 times a day or 150 mg 2 times a day, ravaroxaban at a dose of 10 mg one once a day and apixaban at a dose of 5 mg twice a day, in contrast to the use of the
traditional indirect anticoagulant warfarin, does not require monitoring of INR, a special indicator of the blood coagulation system that reflects the adequacy of anticoagulant therapy. At AF in patients with chronic heart failure and artificial valves, regardless of the type of prosthesis, new oral anticoagulants should not be used. The only drug
the choice in these cases remains warfarin (the value of INR during therapy should vary within 2.5 - 3.5). With a decrease in the glomerular filtration rate less than 30 ml / min
the use of newer oral anticoagulants is strongly discouraged, and the use
warfarin is possible. Oral anticoagulants cannot be replaced by antithrombotic agents, as this reduces the effectiveness of treatment, and the risk of bleeding
remains the same.
Table 1.36
HAS-BLED Bleeding Risk Scale
194

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
Auxiliary medicines. This category includes drugs
the impact of which on the prognosis of patients with chronic heart failure is unknown. Their use
is due not to the presence of chronic HF in the patient, but to the underlying disease and its other complications
opinions.
Peripheral vasodilators do not affect the prognosis, number of hospitalizations and progression of chronic heart failure. Moreover, nitrates may even adversely affect the prognosis of patients with chronic HF and hinder the use of ACE inhibitors. It is
recommended to prescribe nitrates only to patients with coronary artery disease in cases where preven angina attacks are not provided by other antianginal agents. As arteriolar vasodilators,
when indicated, it is recommended to use only long-acting dihydropyridine calcium antagonists.
Calcium antagonists that reduce heart rate (verapamil and diltiazem) are recommended for use only in patients with the initial stages of chronic HF (I - II functional
class) due predominantly to diastolic myocardial dysfunction. Short-acting dihydropyridine drugs are contraindicated in patients with chronic HF. From the group of long-acting dihydropyridines, only amlodipine and felodipine
have a proven ability not to worsen the prognosis of patients with chronic heart failure. Their use (necessarily in combination with the main means of treating chronic HF) is
possible in the presence of persistent angina pectoris, concomitant persistent hypertension, high pulm hypertension, severe valvular regurgitation.
Antiarrhythmic drugs are recommended for use in patients with chronic HF only in cases of life-threatening ventricular arrhythmias
hearts. Class I and IV antiarrhythmics are contraindicated in patients with chronic heart failure. ÿ- blockers are the treatment of choice for ventricular arrhythmias. When they are ineffective, class III drugs (amiodarone, sotalol, dofetilide) are used. Due
with a high risk of side effects, the most effective antiarrhythmic
the drug amiodarone should be used in small doses - 100 - 200 mg / day. The optimal method for the prevention of sudden death in patients with chronic heart failure is the implantation of a cardioverter-defibrillator.
With the development of AF, in most cases, the restoration of sinus rhythm has no advantages over the therapeutic tactics of heart rate control. For this purpose, it is recommended to use a combination of cardiac glycosides and ÿ- blockers. If there is at least one
195

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
risk factor for thromboembolic complications, this combination should be supplemented
oral anticoagulants.
Antiplatelet agents are a class of drugs that are used as part of
therapy for chronic HF is not mandatory. Aspirin and other non-steroidal anti-inflammatory drugs, by blocking the enzyme cyclooxygenase, weaken the effect of ACE inhibitors. Confirmation of the clinical efficacy of clopidogrel, a drug with another
mechanism of antiaggregation effect - in the treatment of chronic heart failure is not. Aspirin is recommended for the treatment of patients with chronic HF when its prescription may have a positive effect on the prognosis due to the underlying disease (for example, in patients who have had a myocardial infarction).
Non-glycoside inotropic agents are used to treat patients with chronic
HF in the phase of decompensation. The drug of choice in critical illness is the calcium sensitizer levosimendan, which improves hemodynamic parameters, but unlike dobutamine has no negative interactions with ÿ- blockers. The drug is injected
IV bolus of 12 mcg/kg, and then slowly at a rate of 0.1-0.21 mcg/kg/min. Electrophysiological and surgical methods of treatment. In the treatment of some
patients with chronic HF successfully apply EF-methods. Patients with disorders rhythm and conduction, if indicated, implantable devices are installed - pacemakers, cardioverter-defibrillators, which reduce the risk of death
from arrhythmias. The method of resynchronization therapy (three-chamber or biventricular stimulation) allows you to set the optimal AV delay for each patient and eliminate asynchrony in the work of the ventricles. This improves hemodynamic parameters and reduces the severity of clinical manifestations of chronic HF. The use of resynchronization therapy reduces the number of hospitalizations and improves prognosis
patients with chronic heart failure. Resynchronization therapy is indicated for patients with chronic HF III - IV functional class with a QRS complex > 120 ms, ejection fraction
less than 40% and the absence of the effect of optimal pharmacotherapy.
Surgical methods for the treatment of chronic HF, as a rule, are used when conservative treatment tactics are ineffective. The effectiveness and safety of surgical methods for the treatment of chronic HF in general have a low level of evidence. The condition of patients with severe mitral regurgitation can be temporarily improved in
as a result of plasty (or prosthetics) of the mitral valve. In patients with coronary artery disease with low ejection fraction of the left ventricle, partly due to the presence of hibernated
myocardium, improvement of systolic function of the heart can be facilitated by myocardial revascularization surgery. The cardinal method of surgical treatment of patients with endstage chronic HF is heart transplantation. In recent years, more and more
actively in the treatment of patients with chronic heart failure began to use auxiliary devices circulation. Artificial ventricles of the heart are constantly being improved. Modern models are miniature turbines that are installed in the cavity
left ventricle. There is now evidence that implantation of an artificial left ventricle improves the prognosis of patients with severe HF. To prevent
progressive dilatation of the heart, a restrictive external elastic mesh can be used. Preliminary results of using this technique in patients with dilated cardiomyopathy show that it can reduce the severity of clinical symptoms of HF and increase the effectiveness of pharmacotherapy.
Prevention. Any heart disease, even in the absence of quantitative criteria for its systolic or diastolic dysfunction, should be considered as a prerequisite for the development of chronic HF and serve as a basis for preventive measures. In this regard, an important direction in the prevention of chronic HF
196

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
is the impact on its cause: medical and surgical treatment of coronary artery disease,
temporary surgical correction of valvular heart disease, treatment of cardiomyopathy, termination action of toxic factors.
An important condition for the success of secondary prevention of chronic HF is the conscious participation of the patient in this process. The patient must be aware of the reasons
the main mechanisms of development and clinical manifestations of chronic HF, trained in methods self-control, and should also have an idea about the acceptable level of physical and
emotional stress, optimal diet, mechanisms of action, direct and side effects of prescribed drugs. When these conditions are met, the treatment process
chronic HF becomes an act of cooperation between the doctor and the patient, which increases the likelihood of achieving the desired result.
197

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
1.12. RHYTHM DISORDERS AND
HEART CONDUCTIVITY
According to the definition of the working group of WHO experts (1978), cardiac arrhythmias (arrhythmias) are any deviations from normal sinus rhythm (SR).
Arrhythmias (it is customary to include not only rhythm disturbances, but also cardiac
conduction disturbances in this concept) are the most common complication of cardiovascular diseases (IH hypertension, heart defects, cardiomyopathy, myocarditis, etc.), but can complicate the
course of diseases of other systems and organs (diseases of the lungs, nervous system, gastrointestinal tra etc.). Arrhythmias can be genetically determined (arrhythmogenic cardiomyopathy / dysplasia
right ventricle, long QT syndrome, Brugada syndrome, etc.). Approximately every 10th patient, their cause remains unknown. Accordingly, when formulating
arrhythmia diagnoses take their place in the "complications" section.
But if the cause is unknown or absent (the so-called idiopathic arrhythmias), the heart rhythm disturbances themselves become the main diagnosis. arrhythmias may be completely asymptomatic, but can significantly reduce the quality of life
sick. On the other hand, rhythm disturbances may be perfectly harmless, but may
cause the patient'sdeath. At the same time, the "symptoms" of arrhythmias and their danger
do not always fall.
It is customary to distinguish supraventricular (supraventricular) and ventricular arrhythmias. The sources of supraventricular arrhythmias can be the sinus node (SU), atria, atrioventricular (AV) node and the trunk of the bundle of His, and ventricular - the legs of the bundle of His
and their branches, Purkinje fibers, ventricular myocardium.
When studying arrhythmias, the following basic terms and concepts may occur. Extrasystole is a premature electrical impulse with a source in the atria, AV node, His-
Purkinje system, ventricles. Extrasystole can be single
and a steam room (2 in a row).
Rhythm (in addition to SR) is three or more electrical impulses of non-sinus origin in a row. If the heart rate is less than the previous HR, the rhythm is called a replacement (slip-
out), more than the previous HR - accelerated. With a heart rate of more than 100 in 1 min, the rhythm called tachycardia (tachyarrhythmia). Tachycardias can be paroxysmal (paroxysmal),
persistent (long-term), continuously recurring
(periodically interrupted by one or more sinus contractions) and chronic (permanent).
Asystole is the absence of electrical activity in the atria and/or ventricles. Sinus bradycardia - SR with a heart rate of less than 60 beats per minute. Sinus tachycardia - SR with a heart rate of more than 100 per 1 min.
Flutter - regular electrical impulses of the atria or ventricles with heart rate more than 250 in 1 min.
Fibrillation - arrhythmic unorganized electrical impulses of the atria or ventricles with a frequency of more than 300 per 1 min.
Blockade - a violation (slowdown or termination) of the conduction of impulses on any
the level of the conducting system.
198

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
1.12.1. Anatomy and physiology of the conduction system hearts. Mechanisms of formation of arrhythmias
The normal electrical activation of the heart (sinus rhythm) is initiated by cells located in the SU region and capable of spontaneous depolarization. SU is in
the confluence of the superior vena cava into the right atrium (Fig. 1.16). It consists of many cells - pacemakers. Cells capable of pacemaker activity, or
P-cells (from the English pale - pale, as they are seen with electron microscopy), generate electrical impulses, and different groups of cells do this at different frequencies. As a rule, cells with a higher frequency of depolarization dominate over others. At
a change in the autonomic tone (the predominance of sympathetic or, conversely, parasympathetic tone), a change in the dominant group of cells can be observed.
Rice. 1.16. conduction system of the heart
From the SU through the atria to the AV node, excitation spreads through three internodal tracts: anterior (Bachmann), middle (Wenckebach) and posterior (Torel). From su to left
atrial excitation spreads along a large interatrial bundle, which also bears the name of Bachmann.
The AV node is located to the right of the interatrial septum, above the site of attachment leaflets of the tricuspid valve, near the mouth of the coronary sinus. In a normal heart
The AV node and the specialized conduction system of the heart only transmit
impulse from the SU and atria to the ventricles. The main feature of the AV node is the slowing of the conduction of excitation, which contributes to the fact that the ventricles begin to be excited only after the end of a full atrial contraction. AV node is normal
"passes" from the atria to the ventricles no more than 180 - 220 imp / min. He'sinfiltrated
sympathetic and parasympathetic nerve endings.
The continuation of the distal part of the AV node is the trunk of the bundle of His, about 10
mm. The AV node and trunk bundle of His together are often described as the AV junction. beam barrel Gisa is divided into legs: right and left. The left leg of the bundle of His, in turn, is divided
on branches: anterior superior and posterior inferior. Many additionally distinguish the anterior septal branch of the left leg. More and more branching, the legs of the bundle of His end in a network Purkinje fibers, which are the last link in the specialized conductive
199

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
systems and connect directly to the cells of the contractile myocardium of the ventricles.
The part of the conduction system of the heart, including the bundle of His and Purkinje fibers, is called
by the His-Purkinje system.
According to the classification of V. F. Hoffman and MR Rosen (1981), the causes of arrhythmias can be
divided into two categories: pulse formation anomalies and excitation conduction anomalies. Both anomalies can be combined.
Anomalous pulse shaping may be associated with accelerated normal
automatism (sinus tachycardia), abnormal automatism or trigger activity (atrial focal tachycardia). The difference between trigger activity and abnormal
automatism is the need for an initiating potential (trigger).
An example of abnormal conduction of excitation is any AV block or blockade of the bundle of His.
One of the most common mechanisms of arrhythmogenesis, reentry (re-entry of the excitation wave), is also associated with abnormal conduction of excitation. The following conditions are necessary for the occurrence of reentry: 1) the presence of a zone of unidirectional
holding block; 2) the possibility of pulse circulation around the zone of the block with its capture retrograde and return to the area of origin of the impulse. Time of excitation
in the reentry chain should be greater than the refractoriness of its constituent tissue. Obviously, that low conduction velocity and a short refractory period contribute to the occurrence
nyu reentry.
An example is the occurrence of paroxysmal reciprocal AV tachycardia in the classic manifesting WPW (Wolf-Parkinson-White) syndrome. As you know, this syndrome is characterized by the presence of an abnormal pathway
- a muscular bridge leading from the atria to the ventricles and having (in comparison with AV connection) greater speed of conduction of excitation and greater refractoriness.
Therefore, during SR, the excitation propagates precisely along the Kent beam. If an atrial premature
beat occurs in a patient so early that it catches the Kent'sbundle in a state of refractoriness (unidirectional block), excitation can spread to the AV junction, which is less refractive. By the time the excitation has spread to the ventricles, the Kent bundle is out of refractory and the excitation
spreads retrograde, i.e. from the ventricles to the atria. Thus, excitation begins to circulate through the loop, one link of which is the Kent bundle, and the other is the AV junction, which is the basis of paroxysmal tachycardia. The initiation of such
tachycardia, by the way, can serve as an example of a combination of abnormal impulse formation (extrasystole) and excitation (reentry). The reentry chain can be large and
form around any anatomical formations in the atria or ventricles, but may be small and due to different EF properties of neighboring areas
myocardium, as is the case with AF, which is based on multiple microreentries in the atria.
1.12.2. The main methods of examination of patients with arrhythmias
Inquiry, examination. In violations of the rhythm and conduction of the heart, questioning is of paramount importance; it allows not only to establish the correct diagnosis, but sometimes
determine the treatment strategy. A conversation with a patient always begins with his complaints. Often
there are complaints corresponding to the most common arrhythmia - extrasystole. First of all,
these are interruptions in the work of the heart. However, many patients are concerned about the feeling of a paus
injury, cardiac arrest.
200
