
1-280 pdf (1)
.pdf
Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
Rice. 1.15. Algorithm for diagnosing chronic heart failure
If deviations from the norm are found, you should proceed to the assessment of function, morphology and geometry of the heart using imaging techniques. Absence of functional disorders,
normal values of indicators characterizing the size and shape of the heart chambers
and its wall thickness, make the diagnosis of chronic heart failure unlikely. Symptoms and clinical signs of cardiac dysfunction do not have to be present at rest: at initial
stages of chronic heart failure, they appear only during exercise. Meanwhile, objective signs of cardiac dysfunction must be detected at rest, since they
appearance under conditions of exercise is not always directly related to chronic HF. For example, decreased left ventricular ejection fraction during exercise
in patients with coronary artery disease may be due to transient systolic dysfunction due to exacerbation of coronary insufficiency. Diagnosis of chronic HF includes the establishment the causes of its development, as well as the identification of factors contributing to decompensation and progression of heart dysfunction.
When formulating a diagnosis, the underlying disease is indicated first. Characteristic chronic HF includes stage and functional class. In cases of severe HF, the diagnosis
its main manifestations are indicated.
Examples of diagnoses:
1. Chronic rheumatic heart disease. mitral stenosis. Permanent form of atrial fibrillation. Chronic cardiac insufficiency IIA Art., III f. to.
2. IHD: postinfarction cardiosclerosis (MI in 2004), aneurysm left ventricle. Chronic heart failure III stage, IV f. to.
Cachexia, ascites, bilateral hydrothorax.
differential diagnosis. In typical cases, when the necessary diagnostic tests are performed sequentially, the recognition of chronic HF does not cause any particular problems.
181

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
past difficulties. The greatest difficulty is the differential diagnosis of early stages of chronic HF and diseases (conditions) accompanied by a decrease in exercise tolerance, shortness of breath and tachycardia. These are most often diseases of the external respiration system, anemia, thyrotoxicosis, and heart rhythm disturbances. Conducting appropriate studies allows you to establish the correct diagnosis.
It must be reiterated that the absence of a decrease in left ventricular ejection fraction does not rule out HF. In patients of this kind, the leading cause of functional heart failure is not systolic, but diastolic dysfunction of the left ventricle, which is most often associated with myocardial hypertrophy due to hypertension. In the Russian population, more than half of patients with chronic heart failure have a left ventricular ejection fraction greater than 50%. Flow. Chronic HF is characterized by a
progressive course. Modern methods of treatment can only temporarily improve exercise tolerance and reduce the severity of other clinical manifestations of heart failure, but periods of relative well-being of the patient are inevitably replaced by periods of decompensation. With the correct implementation of therapeutic measures, it is possible to slow down the process of cardiovascular remodeling. However, negative changes in the organs caused by chronic heart failure progressively increase and their functional inferiority eventually becomes the cause of the patient'sdeath.
Forecast and outcomes. Despite the fact that in the arsenal of a modern doctor there are several classes of drugs that have been proven to reduce the risk of death in patients with chronic heart failure, the prognosis for this disease remains unfavorable. Approximately 50% of patients die within 5 years of the onset of the first
symptoms of chronic HF. Among patients with chronic heart failure functional class I-IV, annual m 6%, II - IV - 12%, IV - 50%. In patients with chronic HF, mortality increases by 3-5 times
compared with persons of the same age and sex without HF. The risk of death in patients with chronic HF is higher than in patients with underlying cancers. Chronic
HF accounts for 5% of adult hospitalizations and is the most common cause of hospitalization in people over 65 years of age. In the Russian Federation, among patients hospitalized due to cardiovascular diseases, almost 20% of patients are referred to hospitals due to decompensation of chronic HF. Within 60 days of discharge from the hospital, 35% of patients with chronic HF either die or are rehospitalized due to decompensation. The main cause of death in patients with chronic
HF is a progressive disorder of systemic hemodynamics, often leading to dysfunction of internal organs, mainly kidneys and liver. Every third patient dies suddenly, from heart rhythm disturbances. In some cases (more often in patients with AF), thromboembolism becomes the cause of death in patients with chronic HF.
Treatment. Treatment of a patient suffering from chronic heart failure is a complex task, the full solution of which is determined not only by a reasonable combination of pharmacological agents that affect the etiological factors and mechanisms of development of heart dysfunction. To reliably prevent the progression of chronic HF, drug therapy should be combined with non-drug measures: rational nutrition, physical training, and psychological support for the patient. Treatment should begin early in the process, when chronic HF occurs only with exercise, and even better with asymptomatic left ventricular dysfunction. In the course of treatment, conditions that exacerbate chronic HF should not be ignored: hypertension, disorders heart rate, anemia.
The goals of treating a patient with chronic HF are as follows:
182

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
1)prevention of the development of symptomatic chronic HF (for stage I);
2)elimination of symptoms of chronic HF (for stages IIA - III);
3)slowing the progression of the disease by protecting the heart and other target organs (brain, kidneys, blood vessels) from damage caused by chronic HF (for stages I-III);
4)improving the quality of life (for stages IIA - III);
5)reduction in the number and duration of hospitalizations (for stages I-III);
6)improvement of the prognosis (for stages I - III).
Thus, the treatment of a patient with chronic HF should combine the effects,
aimed at preventing the development and elimination of symptoms of cardiac dysfunction, with methods that provide inhibition of the process of cardiovascular remodeling and
slowing down the growth of morphological and functional disorders in the organs. When conducting treatment measures, preference should be given to methods that have a positive impact
which on the survival of patients with chronic heart failure has been proven in large controlled research.
Non-drug treatment. The main directions of non-drug treatment of chronic HF are rational nutrition, compliance with the optimal
physical activity and psychological rehabilitation of the patient.
Diet. The main principle of the diet of a patient with chronic heart failure is to limit table salt. The recommended daily intake of NaCl depends on functional
class of chronic heart failure and is for patients with functional class I, II and III, respectively, no more than 3, 1.5 and 1 g. The implementation of this principle is achieved by restricting products, containing a large amount of salt (functional class I), plus undersalting of food (functional class II), plus cooking without salt (functional class III).
Fluid intake is limited only in cases of decompensation of chronic HF, requiring parenteral administration of diuretics. Average daily fluid intake
for a patient with chronic heart failure should be 1 - 1.5 liters. Since the measurement of quantity drunk and excreted fluid is not always possible, the main way to control water
balance is daily weighing. Weight gain more than 2 kg in 3 days
indicates, as a rule, fluid retention and an increased risk of decompensation
sations.
Chronic HF leads to the development of morphofunctional changes in the mucosa
membranes of the stomach and small intestine, violation of the secretory function of the liver and pancreas
glands. These changes cause malabsorption and loss of nutrients,
which increase in parallel with the increase in the functional class of chronic HF. Food
the patient should be high-calorie and easily digestible, which is achieved by shifting the ratio of nutrients towards carbohydrates. At the same time, it should contain a sufficient amount of protein of animal (meat, fish) and vegetable (legumes, soy) origin,
vitamins and electrolytes (cabbage, carrots, beets, dried apricots). The patient should be fed in small portions 5-6 times a day. With pathological weight loss and
development of cardiac cachexia, patients are prescribed nutritional support in the form of various nutrient mixtures.
Physical activity. As chronic HF progresses, the
morphological changes in peripheral vessels: the relative thickness increases vascular wall mainly due to the muscle layer, the lumen of the vessels decreases,
increased peripheral vascular resistance. Violations of the central and peripheral hemodynamics, closely associated with hyperactivation of neurohumoral systems, lead to weight loss and structural changes in skeletal muscles. Improvement
blood flow and skeletal muscle metabolism can be achieved through physical training
183

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
rovok. Contraindications to physical rehabilitation of patients with CHF are: active myocarditis; pronounced stenosis of the valve openings; cyanotic birth defects
hearts; violations of the heart rhythm of high gradations; angina pectoris in patients with low left ventricular ejection fraction.
The choice of exercise regimen is based on the results of a 6-minute test
walk. Patients who have walked less than 150 m, as well as those with severe underweight
body, at the initial stage, only exercises for training the respiratory muscles with
deepening inhalation and lengthening exhalation. For this purpose, special spirometers are used. or simply inflating a rubber toy several times a day. After improvement in the patient's condition, which is usually observed after 3-4 weeks. regular breathing exercises with
difficult expiration and gymnastics in a sitting position, a second test is performed 6 minute walk. If the distance traveled by the patient is 150 - 300 m, go
to the mode of small loads in the form of dosed walking. Classes are held 5 times a week during 18 - 22 weeks. During this time, a gradual increase in walking speed is carried out. and the distance covered by the patient during each session. Patients who have passed when performing a 6-minute walk test over 300 m, daily dynamic
physical activity - walking with a progressive increase in speed up to 6 km / h for up to 40 minutes per day.
Along with dosed walking during physical rehabilitation of patients with chronic CH II - III functional class, it is possible to use training on a bicycle ergometer. If a
in the process of physical rehabilitation of the patient, his condition worsens in the form of progression of clinical symptoms of heart failure, it is necessary to temporarily switch to the previous stage of physical activity. Complete cessation of physical activity is considered as a last resort. In most patients, regular exercise leads to
to a decrease in the functional class of chronic heart failure, an increase in maximum oxygen consumption, restoration of the structure and function of skeletal muscles, effects of drug therapy. However, the positive effect of physical training
after their interruption, it remains for a short time. For this reason, dosed
physical activity is considered as an obligatory and constant component of complex rehabilitation treatment of patients with chronic heart failure.
Psychological rehabilitation, self-control and self-treatment.
rehospitalization of patients with chronic heart failure is largely due to non-compliance or inaccurate implementation of doctor'srecommendations after discharge from the hospital
and the lack of the possibility of frequent medical monitoring of the patient'scondition at the outpatient s treatment. The low adherence of the patient to the doctor'sprescriptions, in turn, is associated with
the complexity of the therapy protocol, as well as insufficient understanding by the patient and his relatives of the meaning of medical recommendations. Awareness by patients of a high risk of another decompensation is a strong psychotraumatic factor that gives rise to
disbelief in the effectiveness of therapeutic measures, and, consequently, an additional reason for their failure. To reduce the likelihood of an exacerbation of chronic HF, the patient should not
only follow the recommendations for drug and non-drug treatment, but
and actively monitor their condition, assess its changes, take available measures to prevent the progression of negative phenomena, and also be under
supervised by specially trained personnel. This strategy for the treatment of patients with CHF in outpatient settings has been called a multidisciplinary approach.
The technique of self-treatment and self-control provides for teaching the patient methods recognition of chronic HF symptoms, assessment of their significance and acceptance algorithms decisions to change treatment or seek advice
to a healthcare worker. A patient suffering from chronic heart failure should have
184

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
knowledge about the causes of the disease, the main mechanisms of its development and clinical manifestations,
as well as methods of non-drug and drug correction. The patient must understand the meaning of maintaining a low-salt diet and exercise in the recommended
mode, know the names, doses, possible side effects of prescribed drugs drugs and outline their mechanisms of action. The patient must have
skills to control the course of the disease (measurement of body weight, pulse, blood
pressure), to be aware of the need for daily recording of physiological parameters that reflect the function of and severity of heart failure, know how much change should be reported to the medical
to the worker and about the acceptable limits of self-modification of therapy. Education of the patient and his relatives is carried out in group sessions using
literature adapted for the patient, after which the patient is given the opportunity to call a nurse or doctor at a certain time with
questions about their condition and treatment recommendations. In addition, the patient'scondition actively monitored by healthcare professionals. With increased clinical manifestations
chronic heart failure and early medical attention, the patient'scondition may be stabilized at home or in a day hospital, which avoids
hospitalizations. In recent years, in order to increase the effectiveness of self-treatment
and self-control, as well as to provide consultation and education for patients with chronic HF,
use electronic monitoring tools and computer telecommunications
systems.
The formation of the patient'sdesire to actively resist the disease, the transfer to him and his relatives of the necessary knowledge and skills contribute to the creation of a favorable psychological environment in the patient'sfamily and the success of treatment in general.
The use of a multidisciplinary approach in the treatment of patients with chronic HF can reduce the incide and duration of hospitalizations, improve the quality of life of patients, increase patient
adherence to treatment recommendations and reduce the cost of medical care. Medical treatment. In the treatment of patients with chronic heart failure,
several classes of drugs. Some of them have been proven to improve prognosis,
i.e. reduce the risk of death and progression of the disease, some reduce the severity of clinical symptoms and improve the quality of life of patients, some pharmacological agents are used for the treatment and secondary prevention of the underlying and concomitant diseases. Individualization of pharmacotherapy is carried out taking into account the stage and functional class of chronic HF, its etiology and type of cardiac dysfunction, character
and features of therapy of concomitant diseases, tolerability of medicinal preparations
comrade
According to the degree of evidence of the effect on the clinic, quality of life and prognosis All drugs used to treat chronic HF are divided into
3 categories: main, additional and auxiliary.
Basic medicines. To the category of essential medicines include drugs whose positive effect on the clinical condition, quality
life and prognosis of patients with chronic heart failure is proven and beyond doubt. To this group includes ACE inhibitors, angiotensin II receptor blockers, ÿ- blockers, competitive
aldosterone antagonists, diuretics, cardiac glycosides, and omega-3 polynenases
saturated fatty acids.
ACE inhibitors are a class of drugs whose positive effect on the prognosis of patients with chronic HF has been proven in many clinical trials. Restoring
balance of neurohumoral systems involved in the pathogenesis of chronic HF, inhibitors ACE improve the clinical condition and increase the survival of patients. Application
ACE inhibitors can reduce the risk of death in patients with chronic heart failure by 23%, and for
185

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
the first 90 days of treatment - by 44%. Along with an improvement in long-term prognosis and a decrease number of hospitalizations due to progression of chronic heart failure, ACE inhibitors have a beneficial effect on central hemodynamics, tolerance to physical
load and quality of life of patients. The effect of ACE inhibitors does not depend on the age of patients and the severity of chronic HF. This class of drugs is indicated for all patients with
chronic heart failure (for any etiology and stage of the process). The sooner treatment begins
the greater the chance of success and prolonging the life of patients. Not prescribing ACE inhibitors is considered unjustified and leads to a deliberate increase in the risk of death of decompensated patients.
The maximum degree of evidence of effect in the treatment of chronic HF of all stages have enalapril and captopril. In addition, therapeutic and prophylactic efficacy
proven for fosinopril, perindopril and lisinopril. Taking into account the data of a number of clinical studies to prevent chronic HF in post-MI patients, captopril, ramipril, trandolapril, fosinopril and zofenopril can be used. For prevention
chronic HF in patients with coronary artery disease without exacerbation, perindopril and ramipril are recommended.
In addition to these drugs, efficacy in the treatment of chronic heart failure is less number of patients demonstrated quinapril and spirapril. Dosages of ACE inhibitors
used for the treatment and prevention of chronic heart failure are presented in Table. 1.31. Absolute contraindications to the use of ACE inhibitors are pregnancy, severe hyperkalemia,
bilateral renal artery stenosis (or stenosis
artery of the only functioning kidney), anamnestic data on angioedema that developed during therapy with drugs of this class. Among the side
effects of ACE inhibitors that require stopping treatment include: increased levels
creatinine (frequency 5-15%), dry cough (frequency 2-3%), symptomatic hypotension (frequency
2 - 3%). To reduce the risk of their occurrence, treatment with ACE inhibitors should begin with the use of low doses. Increasing the doses of drugs to the optimal should be carried out gradually - no more than once every 2-3 days. To prevent hypotension
The first dose of an ACE inhibitor should be given at least 24 hours after profuse diuresis and prior discontinuation of vasodilators. In order to reduce the likelihood of an excessive decrease in blood pressure, it is better to start therapy with ACE inhibitors in the evening - under this condition, the patient, in case of an excessive decrease in blood pressure, will be in the position
lying down, which will minimize the possible negative consequences of arterial
hypotension. In patients with an initially high level of plasma potassium (more than 5.2 mmol / l) at the beginning
treatment with ACE inhibitors, potassium-sparing diuretics should be avoided. At
a significant deterioration in kidney function, it is advisable to transfer the patient to a reception of less dangerous drugs with a double (through the kidneys and gastrointestinal tract) elimination route - fosinopril or spirapril. At the initial stage of therapy with ACE inhibitors, it is recommended
control the level of blood pressure and the content of electrolytes in the blood after 1-2 weeks. after each
increasing the dose of the drug.
Table 1.31
Dosages of ACE inhibitors for the treatment of chronic heart failure (mg % dose)
186

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
Angiotensin II receptor blockers rarely cause dry cough and therefore
are recommended for the treatment of chronic heart failure with intolerance to ACE inhibitors. 3 drugs of this class have the strongest evidence base: candesartan, valsartan and losartan. In terms of their effectiveness in chronic HF, these drugs are not inferior to ACE inhibitors and can be used on an equal basis with them. The results of cohort studies have shown the advantage of angiotensin II receptor blockers over ACE inhibitors in the
treatment of women with chronic HF, especially when it is combined with hypertension. Dose titration angiotensin II receptor blockers are carried out according to the same principles as titration
doses of ACE inhibitors (Table 1.32).
Use of angiotensin II receptor blockers in addition to ACE inhibitors
in patients with chronic HF is not recommended because all patients with chronic HF should receive combination therapy with ACE inhibitors and ÿ- blockers.
Along with the fact that triple neurohumoral blockade can enhance the effect on the process of cardiovascular remodeling, the combination of ACE inhibitors, ÿ- blockers and angiotensin II receptor blockers can lead to an excessive decrease in blood pressure. and reactivation of neurohumoral systems responsible for the progression of chronic CH. For this reason, it is recommended to add an aldosterone antagonist rather than an angiotensin II receptor blocker as a third neurohumoral modulator to the combination of an ACE inhibitor and a ÿ- blocker.
ÿ- blockers have a negative inotropic effect. Concerning
drugs of this class until the mid-90s. 20th century were considered absolutely
contraindicated for patients with chronic HF. However, the accumulation of data on negative consequence hyperactivation of the sympathetic-adrenal system, characteristic of chronic HF, created a
theoretical basis for the use of ÿ- adrenoblockers to correct dysfunctions of the heart as a pump and improve prognosis.
Table 1.32
Dosages of angiotensin II blockers for the treatment of chronic heart failure insufficiency (mg % frequency of administration)
187

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
An important negative consequence of hypercatecholaminemia is the accumulation of cyclic adenosine monophosphate in cardiomyocytes. This leads to an overload of cells with ions. calcium, the development of contracture of myofibrils, electrical instability of the myocardium, structural disorders in the sarcolemma and becomes the direct cause of the death of part cardiomyocytes. Under the influence of catecholamines, the synthesis of proinflammatory cytokines increases, which, in turn, contribute to the formation of oxidative stress and the activation of apoptosis. Hypercatecholaminemia contributes to myocardial hypertrophy,
causes an increase in heart rate and afterload, as a result of which the demand of the heart muscle for oxygen. An increase in the activity of the sympathetic-adrenal system causes stimulation renin-angiotensin-aldosterone system. Increased production of angiotensin II and al
dosterone leads to increased vasoconstriction and fluid retention in the body, and then
consequently, to an increase in postand preload, progression of the remodeling process
heart, deterioration of coronary perfusion. Along with irreversible morphological disorders of the heart muscle due to necrosis and apoptosis of cardiomyocytes, areas of hibernated myocardium are formed under conditions of hyperactivation of the sympathetic-adrenal system.
By weakening the effects of hyperactivation of the sympathetic-adrenal system, ÿ-
blockers, when administered to patients with chronic heart failure, prevent the development of necrosis, apo hibernation of cardiomyocytes, ischemia and hypertrophy of the myocardium, as well as the
occurrence of ventricular arrhythmias, which reduces the risk of sudden death in patients. In addition, the use of ÿ- blockers for a long time leads to increased sensitivity
and ÿ- adrenergic receptors in the myocardium.
In the development of the clinical effect of ÿ- blockers in chronic HF, distinguish two phases. Initially, due to the weakening of neurohumoral stimulation,
decrease in myocardial contractility and heart rate, which can lead to a decrease in cardiac ejection. But at the same time, myocardial oxygen demand also decreases. Some cardiomyocytes come out of the state of hypoxic contracture, as a result of which the diastolic relaxation of the myocardium improves. In the future, the positive effects of protecting the heart from excessive neurohumoral stimulation will increase: apoptosis will be inhibited,
the number of hibernating cardiomyocytes will decrease, myocardial contractility will increase and eventually cardiac output will increase. Achieving long-term effects of ÿ- adrenergic blockers is the goal of their use in chronic HF. However, at the beginning
therapy in patients with tachycardia, a distinct positive effect can be obtained, due to the lengthening of the diastole, due to which the diastolic filling of the left ventricle increases and myocardial perfusion improves.
The results of a series of large prospective studies have convincingly confirmed the
ability of ÿ- blockers to improve the prognosis of patients with chronic HF. By the beginning of the XXI centur more than 30 studies have been completed that analyzed the results of long-term
treatment of more than 20,000 patients. In patients with chronic heart failure treated with ÿ- blockers, the risk of death was 29% less than in patients receiving basic therapy, including ACE
inhibitors.
188
Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
To date, efficacy, safety and positive impact on prognosis
in chronic HF, it has been proven for three compounds: the selective ÿ- blockers biso prolol and metoprolol (sustained release) and the non-selective ÿ- adrenoblocker carvedilol, which has the properties of a ÿ-1- adrenoblocker and antioxidant. Other ÿ- blockers do not have the ability to improve the prognosis of patients with chronic heart failure.
The use of atenolol and metoprolol tartrate for the treatment of patients with chronic HF is contraindicated. In the treatment of patients older than 70 years, in addition to the three listed drugs nebivolol may be used. While not reducing overall mortality, this drug reduces morbidity, readmissions, and the risk of sudden death in elderly patients with
chronic heart failure.
According to current recommendations, ÿ- blockers should be prescribed to all
patients with chronic heart failure and a left ventricular ejection fraction of less than 40% who do not have contraindications to the use of this class of drugs. Absolute contraindications to the use of ÿ-
blockers are: bronchial asthma and severe pathology
bronchi, symptomatic bradycardia (less than 50 bpm), symptomatic hypotension (less than 85 mm rt. Art.), AV block II degree or more, severe obliterating endarteritis. ÿ- blockers are recommended only in addition to ACE inhibitors (and, if necessary, diuretics) after stabilization of the patient's condition. Treatment with ÿ- adrenergic blockers is recommended to start with
one
/8 therapeutic dose. Dose titration should
be administered slowly: it is not recommended to increase the dose more than once every two weeks
and more than double. The optimal dose of the drug is selected individually, taking into account the heart rate,
blood pressure level and dynamics of clinical manifestations of chronic heart failure.
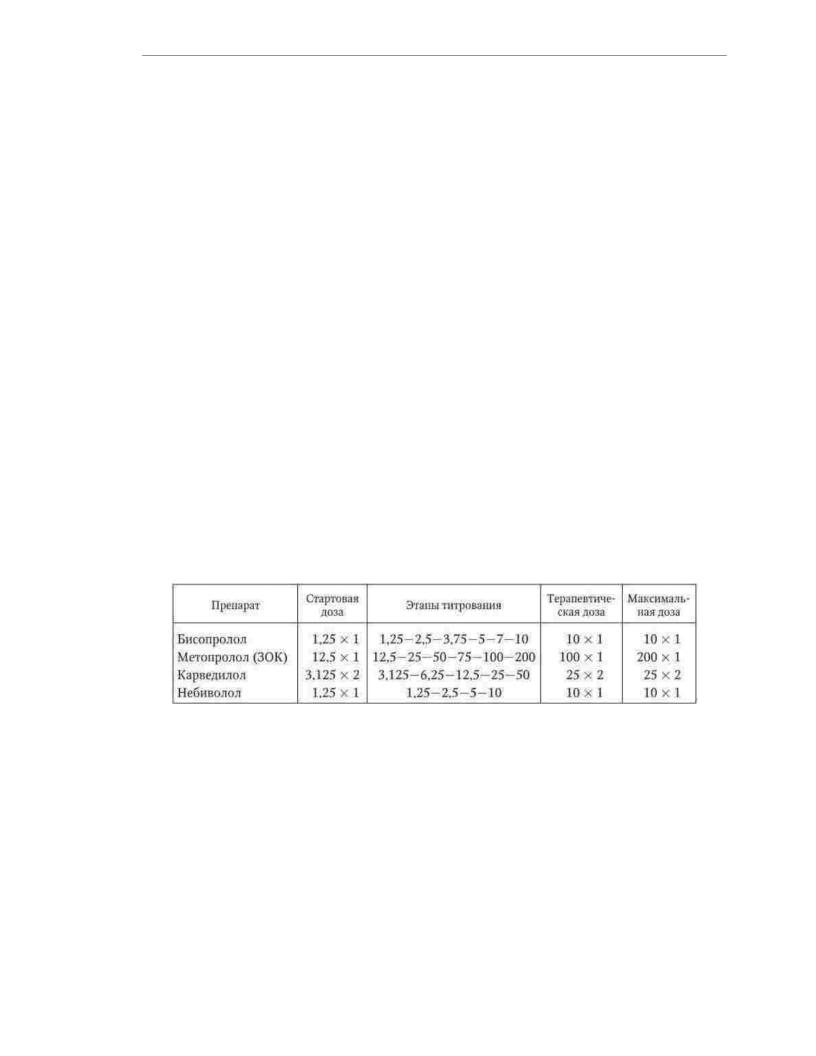
Recommended doses and titration steps of ÿ- blockers for patients with chronic heart failure are presented in Tab
Table 1.33
Dosing of ÿ- blockers in the treatment of patients with chronic heart failure (mg % frequency of administration)
If during therapy with ÿ- blockers there is an increase in the clinical symptoms of HF, it is recommended to increase the dose of ACE inhibitors and diuretics and only if
the ineffectiveness of this measure, temporarily reduce the dose of ÿÿblockers. With the development of hypotension and bradycardia, doses of vasodilators and compounds that reduce
heart rate should first be reduced. The dose of ÿ- blockers is temporarily reduced (up to the termination reception) only in case of ineffectiveness of other measures to stabilize hemodynamics. If the patient'scondition improves, an attempt should be made to increase the dose of ÿ- blockers or
resume therapy. If a patient develops chronic decompensation
HF requiring inotropic support, then levosimendan should be considered the treatment of choice, belonging to the class of calcium sensitizers - drugs whose effect does not depend on
degree of blockade of ÿ- adrenergic receptors.
In case of intolerance or insufficient effectiveness of ÿ- blockers in patients
with an ejection fraction of the left ventricle 7 35% and preserved sinus rhythm at heart rate
189

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
> 70 in 1 min, it is recommended to use ivabradine, an inhibitor of If-channels, which has property of an isolated decrease in heart rate.
Aldosterone antagonists. One of the consequences of chronic activation of the renin- angiotensin-aldosterone system is increased production of aldosterone, a neurohormone that acts on specific receptors located in the distal tubules.
kidneys, vascular endothelium and myocardium. Activation of aldosterone receptors leads to a delay
sodium and water, increased secretion of potassium and hydrogen ions into the lumen of the tubules, promotes perivascular fibrosis and progression of cardiosclerosis. As a result of these processes
systolic and diastolic dysfunction of the myocardium increases, the risk of developing acute coronary insufficiency and ventricular arrhythmias increases. Competitive aldosterone antagonists (spironolactone, eplerenone), binding to receptors
aldosterone in the distal renal tubules, inhibit sodium reabsorption and potassium excretion from the body. However, the therapeutic effect of competitive aldosterone antagonists
in chronic heart failure is mainly due to neuromodulatory rather than diuretic effect of drugs of this class, since the blockade of aldosterone receptors located
in vessels and myocardium, provides inhibition of the process of cardiovascular remodeling
vanity.
To achieve a diuretic effect in decompensated chronic heart failure, spironolactone is used at a dose of 100–300 mg/day. After elimination of edematous syndrome (through
1 - 3 weeks.) The dose of the drug is reduced to 25 - 50 mg / day. The drug is prescribed either once in the morning, or twice in the morning. When combined with ACE inhibitors (especially
at the beginning of therapy), it is necessary to control the level of potassium and creatinine in the blood.
Diuretics are an essential component of the treatment of chronic HF, accompanied by development of edematous syndrome. The central mechanism of fluid retention in the body during chronic heart failure is a decrease in glomerular filtration rate, which is due to
deterioration of blood supply to the kidneys due to a decrease in cardiac output. However, glomerular filtration is not directly related to renal blood flow, so
how its decrease is partly offset by an increase in intraglomerular pressure due to
spasm of the efferent artery due to increased production of angiotensin II. However, when this increases obligate reabsorption in the proximal tubules, due to the action of aldosterone, the reabsorption of sodium and water in the distal tubules increases, and vasopressin enhances the reabsorption of water in the collecting ducts. Thus, there is an excess
fluid retention in the vascular bed and an increase in the volume of circulating blood. Damage to the glomerular membranes seen in chronic HF due to hemodynamic and
neurohumoral disorders, leads to the development of proteinuria and hypoproteinemia. Following
the effect of an increase in hydrostatic pressure, a decrease in oncotic and osmotic pressure
ion in the vascular bed, conditions are created for sweating of fluid into the interstitial
space. The movement of fluid from the vessels into the tissues leads to the formation of edema. Diuretics can eliminate the edematous syndrome and reduce the frequency of
hospitalizations of patients with chronic heart failure. However, they (with the exception of torasemide) do n slow the progression of the disease and do not improve the prognosis, and their impact on the quality
life of patients is ambiguous and largely depends on the treatment regimen. Thiazide diuretics act on the cortical segment of the ascending loop
Henle and the initial section of the distal tubules. By interfering with sodium reabsorption, drugs of this group increase diuresis by 30 - 50%. A fundamentally important condition for the development of the diuretic effect of thiazide diuretics is the preserved kidney function. As filtration decreases, the effect of thiazide diuretics progressively weakens. At a glomerular filtration rate of less than 30 ml / min, the use of thiazide diuretics is meaningless.
Loop diuretics (furosemide, uregit, bumetanide) block sodium reabsorption for pro-
190
