
1-280 pdf (1)
.pdf
Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
ny symptom complex that complicates the course of a particular disease of the cardiovascular system, but also as an independent nosological form.
The term "congestive heart failure" refers to the clinical variant of chronic heart failure, manifested by symptoms of congestion in the pulmonary and/or systemic circulation. Provided that the diagnosis of chronic HF is correctly formulated, the use of this term in medical documents is not recommended. The term chronic insufficiency
blood circulation” has become widespread in our country mainly in connection with the classification of N. D. Strazhesko and V. Kh. Vasilenko, according to which circulatory failure of the heart (or central), vascular (or peripheral) was distinguished
origin and general cardiovascular insufficiency. In the modern classification that regulates the formulation of the diagnosis of chronic HF, the term "chronic circulatory failure" is not used. In accordance with the principle of unification
terminology, its use in medical documents is also discouraged.
Prevalence. Since the 70s. 20th century worldwide there is a rapid increase in the prevalence of chronic heart failure. Currently clinical manifestations
Chronic HF occurs in 1–2% of the population in industrialized countries. In the Russian Federation, the prevalence of chronic HF is 7%. Clinically pronounced chronic HF (II-IV functional class) is diagnosed in 4.5%, severe chronic HF (III-IV functional class) - in 2.1% of the population. Prevalence
chronic HF increases significantly with age, amounting to 20 -
29 years old 0.3%, in the age group over 65 years - 10%, and in the age group over 90
years - about 70%. In the population under 60 years of age among men, the prevalence of chronic heart failure
higher than among women, which is associated with an earlier incidence of hypertension and coronary artery disease in men.
However, in general, due to longer life expectancy, the number of women suffering from chronic HF, 2.6 times higher than the number of sick men.
Etiology. Chronic HF is an outcome of many diseases of the cardiovascular system, but its main causes are coronary artery disease and hypertension. According to the Framingham Study, CAD is the cause of chronic HF in 40% of men and women, and hypertension in 30% of men and 37% of women. Euro Heart Survey HF results, performed on a European sample of patients showed that in 60% of cases chronic
HF is due to ischemic heart disease, in 14% of cases - valvular heart disease, in 11% of cases - dilated cardiomyopathy, in 11% of cases - other causes (amyloidosis, toxic effects and etc.). According to the mentioned study, only 4% of cases of chronic HF are associated
with isolated AG. Meanwhile, AH is registered in more than half of patients with coronary artery disease. AT
Europe, hypertension is observed in 53% of patients with chronic heart failure. Analysis of the results of the study
Russian sample (EPOKHA-O-CHF study) showed that hypertension is the cause of chronic heart failure or is associated with another disease causing it in 80% of cases. Thus, there are reasons to consider hypertension as the main cause of chronic HF in the population
of the Russian Federation. The second place is occupied by coronary artery disease, a chronic form which is the cause of chronic heart failure in 66% of patients. In 19% of patients with chronic heart failure develops as a result of myocardial infarction. Rheumatic heart disease and dilated
cardiomyopathy account for 7.5% and 3.5% of cases, respectively.
Along with the main etiological factors directly associated with chronic HF, there are factors that contribute to cardiac decompensation. To
they include:
1)transient myocardial ischemia;
2)heart rhythm disturbances;
3)pulmonary embolism;
4)physical and emotional overstrain;
171

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
5)exacerbation of chronic inflammatory diseases;
6)bad habits (smoking, alcohol abuse);
7)dietary disorders (excessive consumption of table salt);
8)irregular or ineffective pharmacotherapy of hypertension, coronary artery disease, chronic heart failure;
9)the use of drugs with a negative inotropic,
cardiotoxic action and contributing to fluid retention in the body. Pathogenesis. Morphofunctional changes in the heart muscle, developing
due to diseases of the cardiovascular system, are expressed in the form of myocardial hypertrophy and/or dilatation of the chambers of the heart, which become the basis for the formation of diastolic and/or systolic dysfunction, respectively. Cardiac dysfunction, progressing, leads to a decrease in cardiac output. Reducing the mass of the contracting myocardium and/or increased rigidity of the heart muscle cause a complex of adaptive and pathological reactions, resulting in the formation of chronic HF syndrome.
The period of time from damage to the heart to a decrease in cardiac output can be calculated hours, even minutes, for example, with extensive MI, or stretch for years and decades - in patients with chronic coronary artery disease, hypertension, valvular heart disease, etc.
The pathogenetic mechanisms of chronic HF are universal and do not depend on the etiology of damage hearts.
From the earliest stages of the formation of chronic heart failure, compensatoryadaptive mechanisms are activated that prevent a decrease in cardiac output, the main of which are the Frank-Starling mechanism (increase in the force of contraction
muscle fiber as its diastolic stretch increases) and an increase in heart rate.
The Frank-Starling mechanism normally ensures the adaptation of the heart to increased load, and if it is damaged, it allows you to save the stroke volume of blood, despite
decrease in myocardial contractility. However, the compensatory possibilities of this mechanism not unlimited. Approaching the tensile limit of the muscle fiber is accompanied by
a decrease in the increase in the strength of its systolic shortening, and reaching this limit leads to a decrease in the contraction power. In this regard, as the dilatation of the ventricle increases, the compensatory capabilities of the Frank-Starling mechanism are depleted, the ability of the myocardium to develop additional stress decreases and a progressive decrease in stroke volume begins.
An increase in heart rate is a rapid mechanism for the adaptation of the heart to an increase in the metabolic needs of the body, which is observed, for example, during physical load. With a decrease in stroke volume due to heart damage, an increase in heart rate
allows you to maintain the value of the minute volume of blood circulation at a normal level. At the same time, the shortening of diastole is accompanied by a decrease in the
effectiveness of tachycardia as a mechanism that prevents a decrease in cardiac output, and with a prono With an increase in heart rate, tachycardia becomes an additional factor contributing to a
decrease in the one-time performance of the heart.
The decrease in cardiac output causes constriction of the peripheral vessels. This The compensatory-adaptive mechanism makes it possible to preserve the perfusion of
vital organs due to the deterioration of blood flow in the periphery. Violation of the blood supply to the kid entails sodium and water retention, which, on the one hand, contributes to an increase in
venous return (and, consequently, activation of the Frank-Starling mechanism), but on the other hand, causes the formation of congestive syndrome.
Thus, the action of compensatory-adaptive mechanisms in chronic HF is phase: adaptive processes, as they increase, pass into a pathological phase, acquiring a damaging character.
172

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
The main role in the development of compensatory-adaptive reactions is played by hyperactivation of a number of neurohumoral systems. On the other hand, for the same reason, the transition of adaptive processes to the pathological phase occurs. neurohumoral systems, involved in the regulation of blood circulation can be divided into two groups. To the first group includes systems that provide vasoconstriction, fluid retention in the body, proliferation of cardiomyocytes and smooth muscle elements of the vascular wall. These include the sympatheticadrenal system (norepinephrine and adrenaline), the renin-angiotensin-aldosterone system (angiotensin II, aldosterone), as well as vasopressin, endothelin, factor
growth, cytokines, tumor necrosis factor-a, tissue plasminogen activator inhibitor. The second group includes neurohormones that have opposite effects -
vasodilator, antidiuretic and antiproliferative: nitric oxide, natriuretic peptides, prostaglandins, kallikrein-kinin system (bradykinin), tissue plasminogen activator. Normally, opposing neurohumoral systems are located in
state of equilibrium. With the development of chronic HF, the neurohumoral systems of the first groups begin to prevail over the neurohumoral systems of the second group. at first
an imbalance of neurohormones stimulates adaptive mechanisms: compensatory dilatation and compensatory hypertrophy of the left ventricle develop, a compensatory increase in heart rate occurs, regional blood flow is redistributed towards the heart and
skeletal muscles, sodium and water retention resulting from renal vasoconstriction contributes to maintaining the required level of perfusion of vital organs. However, as the neurohumoral imbalance intensifies, the formation of chronic
hyperactivation of neurohumoral systems of the first group, a direct toxic effect of neurohormones on cardiomyocytes begins to manifest itself, the processes of heart dilatation and myocardial hypertrophy pass into a pathological phase, vasoconstriction and fluid retention
in the body become redundant, and further neurohumoral stimulation contributes to the progression of chronic HF. It should be emphasized that the leading role in the activation of compensatory-adaptive mechanisms and the subsequent disruption of adaptive
reactions are played by tissue neurohormones.
Increased synthesis of neurohormones in cardiomyocytes and associated with this process activation of proinflammatory cytokines and protooncogenes stimulate the development of myocardial hypertrophy. Along with an increase in muscle mass, collagen synthesis also increases.
Moreover, thin collagen filaments that provide communication between individual cardiomyocytes and their associations in muscle bundles are replaced by coarse strands of type III collagen, which prevents
the coordinated work of muscle elements. In addition, thickening of the connective tissue
sheaths surrounding cardiomyocytes and capillaries, makes it difficult for oxygen to diffuse, while as the need for it increases. As a result, myocardial hypoxia increases, and
gradually develops dystrophy of the heart muscle. Due to neurohumoral stimulation, combined with a deterioration in myocardial blood supply, some of the cardiomyocytes flow into
into a state of hibernation (hibernation). The cells of the hibernated myocardium do not actively contract, but at the same time remain viable. If there is no improvement in perfusion of hibernated myocardium, changes in cardiomyocytes become irreversible.
character. In addition to myocardial hypertrophy and hibernation, followed by cardiac dystrophy muscles, tissue neurohormones stimulate apoptosis - programmed cell death.
As a result of these processes, the number of contractile elements in the myocardium decreases, dilatation of the heart progresses, spherization of the cavity of the left ventricle occurs, and the process remodeling of the heart passes into a maladjustment phase.
The decrease in cardiac output is accompanied by the activation of circulating neurohumoral systems. In the bloodstream, the content of norepinephrine, angiotensin II, and aldosterone increases. This leads to the development of adaptive reactions on the systemic and organismal
173

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
levels, involvement in the pathological process of other organs and, as a result, to the formation detailed clinical picture of chronic heart failure.
Most patients develop clinical symptoms of chronic HF
due to a decrease in the performance of the heart. However, in some cases, clinical signs of HF are associated with increased cardiac output. These include pathological conditions in which the metabolic needs of the body increase (thyrotoxicosis), as well as diseases that result in the development of functional
inferiority of other parts of the oxygen transport system (impaired oxygenation
blood, anemia, changes in the properties of hemoglobin, arteriovenous shunting of blood to periphery).
Morphology. Morphological changes in the myocardium in chronic HF are largely determined by the underlying disease. With hypertension and overload of the heart with pressure, concentric hypertrophy of the left ventricle develops, i.e. thickening of its walls without cavity dilatation. When the heart is overloaded with volume, which is characteristic of valvular heart disease and a decrease in myocardial contractility of ischemic origin,
eccentric hypertrophy of the left ventricle develops - the mass of the myocardium increases, but the wall thi ventricle due to its dilatation does not change significantly.
Concentric cardiac remodeling is more favorable and reflects
adaptation phase of the process. After pressure overload is joined by volume overload, eccentric remodeling begins, which reflects the transition of the process to the pathological phase. The starting point of eccentric remodeling is the formation of mitral insufficiency. The immediate cause of mitral
insufficiency in hypertension is diastolic dysfunction of the left ventricle. Thickening and a decrease in the elasticity of the walls of the left ventricle lead to overload and
subsequent dilatation of the left atrium, and then to blood creagurgitation through the left atrioventricular orifice. In hypertensive patients, the concentric remodeling phase may be quite long. The transition of the process to the phase of eccentric remodeling is
accelerated due to the development of myocardial ischemia, which is facilitated by its hypertrophy and progression of atherosclerosis of the coronary arteries. In patients with coronary artery
disease, especially after the development of MI, mitral insufficiency is formed due to systolic dysfunction. left ventricle, which is accompanied by an increase in the residual volume of blood in the
ventricle and dilatation of its cavity. Thus, in a number of patients with coronary artery disease, remodeling of t can immediately acquire an unfavorable eccentric character.
Microscopic examination of the myocardium reveals signs of cardiomyocyte hypertrophy and fibrosis. In cardiomyocytes, dystrophic changes are found in the form of degeneration of mitochondria and myofibrils.
In parallel with cardiac remodeling, vascular remodeling also occurs. essence
this process consists in a decrease in elasticity and an increase in the thickness of the vascular wall mainly due to the muscle layer. The outer diameter of the vessel may remain unchanged as
the vessel lumen narrows. The most important cause of remodeling
vessels is endothelial dysfunction, which, on the one hand, is formed due to imbalance of neurohumoral systems, and on the other hand, contributes to its further
strengthening, as it causes an increase in the secretion of compounds that stimulate the proliferation of smooth muscle cells and have a vasoconstrictor effect. Consequence arterial remodeling is an increase in peripheral vascular resistance
and an increase in the speed of propagation of the pulse wave.
The progression of disorders of central hemodynamics entails a generalized deterioration in blood supply, as a result of which dystrophic changes in the cells of internal organs and atrophy of skeletal muscles develop.
174

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
Classification. In Russia, the classification of N.D. was used for a long time.
Strazhesko and V. Kh. Vasilenko (1935). Subjected to repeated modifications, it has withstood the test of practice for more than 60 years. This classification reflects the staging of morphological changes in organs observed during the progression of chronic HF, but a large number of patients with the preclinical phase remain outside of it.
development of functional inferiority of the heart. On the need to identify the preclinical stage of HF in the mid-30s. of the last century, wrote G. F. Lang. Subsequently, N. M. Mukharlyamov (1978), F. I. Komarov and L. I. Olbinskaya (1978) made proposals to make appropriate changes to the national classification of chronic HF.
In the countries of North America and Europe, since 1964, the classification of chronic HF proposed by the experts of the New York Heart Association (NYHA) has been widely used, in which four functional classes are distinguished depending on the ability of the patient bear physical stress. Unlike the classification of N. D. Strazhesko and V. Kh. Vasilenko, the NYHA classification is based on a functional principle. The value of the functional class determines the prognosis of the patient and is closely related to the nature of the treatment.
In connection with the change in ideas about the pathogenesis and mechanisms of
progression of chronic HF, which have occurred since the creation of the classification by N. D. Strazhesko a H. Vasilenko, in 2002 a new Russian national classification was adopted (Tab.
1.29).
Table 1.29
Russian national classification of chronic heart failure (2002)
175

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
This classification retains the positive features of the old domestic classification and introduces functional criteria. It allows the diagnosis of chronic HF to be established at the preclinical stage. The first part of the classification characterizes the degree of morphological changes in the myocardium, as well as peripheral organs and systems, and the second part
characterizes the functional state of the heart. The stage of the disease reflects the degree of maximum morphological changes associated with the remodeling of the heart and blood vessels, and in the process treatment does not change. In contrast, the functional class of chronic HF
dynamic. The decrease in functional class during therapy reflects a positive
the effect of the treatment on the condition and prognosis of the patient, the absence of changes in the functional class is a sign of insufficiently effective treatment, an increase in the functional class indicates the need to change the treatment program.
clinical picture. Diagnosis of chronic HF is largely based on the results of questioning and physical examination of the patient. The main symptoms (complaints of the patient) include: shortness of breath, fatigue, palpitations,
cough, orthopnea. The most frequent complaints of patients and the earliest manifestations chronic heart failure are shortness of breath and fatigue. Palpitations are noted somewhat less frequently, followed by peripheral edema, cough, and
orthopnea.
In the early stages of the development of chronic heart failure, shortness of breath appears only with physical
load of lesser intensity than in healthy individuals. The cause of shortness of breath in most
cases is a decrease in the contractility of the left ventricular myocardium, which entails an increase in
176

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
decrease in pressure in the pulmonary veins and capillaries, a decrease in the elasticity of the lungs, a decrease
tidal volume and increased bronchial resistance. As you progress
HF dyspnea begins to bother patients in the supine position, in some patients there is paroxysmal nocturnal dyspnea. When moving to a sitting position, shortness of breath decreases and
disappears. This phenomenon is based on the movement of part of the blood into the vessels of the chest, as well as a decrease in the activity of the sympathetic nervous system and respiratory depression. center at night. In severe HF, progression of dyspnea may be facilitated by
accumulation of fluid in the pleural cavities, pericardial cavity and abdominal cavity. General weakness and fatigue also appear early in the development of chronic HF and
gradually worsen. These complaints are due to poor blood supply
skeletal muscles due to a decrease in cardiac output and an increase in the tone of the peripheral arteries. In addition, skeletal muscle metabolism deteriorates due to an increase in the blood concentration of catecholamines, angiotensin II, a number of other neurohormones, and biologically active compounds.
Palpitations in patients with chronic heart failure initially occur during exercise,
and subsequently observed at rest. In most cases, this complaint is due to sinus tachycardia, which is a mechanism to compensate for the decrease in stroke volume, preventing a decrease in cardiac output. In patients with severe HF
palpitations are often associated with permanent AF.
Edema occurs in patients with chronic heart failure with a significant increase in volume extracellular fluid. This is facilitated by increased reabsorption of sodium and water in the kidneys. due to a decrease in the rate of glomerular filtration, which in turn is caused by a violation of central hemodynamics and the balance of neurohormones, in particular,
an increase in the concentration of catecholamines, angiotensin II, aldosterone, vasopressin in
the blood. The exit of the liquid part of the blood from the vessels into the interstitial space is facilitated by an increase in hydrostatic pressure, a decrease in the osmotic and oncotic pressure of blood
plasma, characteristic of chronic HF.
Physical examination of a patient with chronic heart failure may reveal: cyanosis, peripheral edema, jugular vein swelling, tachycardia, gallop rhythm, dilatation
boundaries of relative cardiac dullness and lateral displacement of the apex beat, moist rales in the lungs, hepatomegaly. The severity of clinical signs of HF varies greatly. So, with moderate HF, only cyanosis of the lips is noted, and with severe HF,
cyanosis of the auricles, tip of the nose, nail phalanges of the fingers and toes. For moderate heart failure there is swelling of the rear of the feet and ankles, quickly disappearing in the supine position.
In the terminal stage of the process, pronounced persistent peripheral edema is formed, hydrothorax, hydropericardium, ascites. Jugular vein swelling and hepatomegaly are signs of right ventricular failure. Usually these symptoms are combined with dilatation of the right
chambers of the heart, which is manifested by the expansion of the boundaries of absolute cardiac dullness.
Auscultation of the heart reveals a weakening of the first tone at the apex, an accent of the second tone on the pulmonary arter
(during the formation of pulmonary hypertension), the presence of pathological III and IV tones. In cases severe dilatation of the left and right chambers of the heart appear systolic murmurs of mitral and tricuspid regurgitation. On auscultation of the lungs in patients with congestive
left ventricular failure revealed small bubbling moist rales in the lower paravertebral and lower axillary areas.
To quantify the clinical status of a patient with chronic heart failure, apply a specially developed scale that provides an assessment of the severity
the main symptoms in points, which are subsequently summed up. The maximum score is 20, which corresponds to severe chronic HF. I functional class
177

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
corresponds to the amount up to 3.5 points, II - the amount from 3.5 to 5.5 points, III - the amount from 5.5 to 8.5 points,
IV - the amount of more than 8.5 points.
Scale for assessing the clinical condition in chronic heart failure (Mareev V. Yu., 2000):
1.Shortness of breath: 0 - no, 1 - during exercise, 2 - at rest.
2.Has the weight changed over the past week: 0 - no, 1 - increased.
3.Complaints about interruptions in the work of the heart: 0 - no, 1 - yes.
4.In what position is he in bed: 0 – horizontally, 1 – head up (+ 2 pillows), 2 – head up + nocturnal choking, 3 – sitting.
5.Swollen neck veins: 0 - no, 1 - lying down, 2 - standing.
2
6. Wheezing in the lungs: 0 - no, 1 - lower sections (up to one /3), 2 - up to the shoulder blades (up to/3), 3 - over the entire surface of the lungs.
7.The presence of a gallop rhythm: 0 - no, 1 - yes.
8.Liver: 0 - not enlarged, 1 - up to 5 cm, 2 - more than 5 cm.
9.Edema: 0 - none, 1 - pastosity, 2 - edema, 3 - anasarca.
10.Systolic blood pressure level: 0 - > 120, 1 - (100 - 120), 3 - < 100 mm Hg. Art.
The results of the assessment of the clinical condition make it possible to determine the prognosis of the patient,
and with the repeated application of this technique - to get an objective idea of the effectiveness of therapy.
With an increase in the number and severity of the corresponding symptoms and clinical signs, the likelihood of a diagnosis of chronic heart failure increases. However, all of the above above manifestations of chronic HF are not specific, therefore, to confirm
diagnosis of chronic HF, previously established on the basis of complaints and results physical examination of the patient, it is necessary to use the methods of instrumental and
laboratory research, objectively characterizing the function of the heart and the state of blood circulation.
Laboratory and instrumental diagnostics. In patients with suspected
diagnosis of chronic heart failure, it is recommended to perform the following laboratory tests: clinical blood count, analysis of the content of electrolytes in the blood, determination of the level
serum creatinine and glomerular filtration rate, blood glucose, hepatic enzymes in the blood, urinalysis. In patients with moderate HF
slight anemia, small electrolyte shifts in the form of hyponatremia and hypokalemia, hypercreatininemia can be detected. The above changes are not
specific for CH.
To diagnose chronic heart failure, a blood test for the content of natriuretic hormones is performed. This test is characterized by a high negative diagnostic value - with a low content of natriuretic hormones in the blood, the probability of chronic HF is close to zero. Plasma levels of natriuretic hormones
judge not only the presence or absence of HF, but also the stage of the disease, prognosis, and evaluate the effectiveness of treatment. In practice, the most widely used test is to determine the level of brain natriuretic hormone and its N-terminal precursor.
Their content in blood plasma increases depending on the severity of myocardial
stress. At levels of brain natriuretic hormone and its N-terminal precursor less than 100 and 400 pg/ml, respectively, the diagnosis of chronic HF is unlikely; at levels of 100–400 and 400–2000 pg/ml, respectively, the diagnosis is unclear;
pg/ml, respectively, the diagnosis of chronic HF is likely. The level of natriuretic hormones increases not only in patients with HF, but also in left ventricular hypertrophy, tachycardia, myocardial ischemia, hemodynamic overload of the right ventricle, hypoxemia, kidney dysfunction, liver cirrhosis, sepsis, infection, and in the elderly.
178
Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
The most accessible method to detect objective signs of heart damage is electrocardiography. Unaltered ECG in patients with chronic heart failure
is extremely rare. In an electrocardiographic study of patients with
suspected chronic HF, signs may be identified that indicate the presence of a morphological basis of systolic and / or diastolic dysfunction of the heart, and
also rhythm and conduction disturbances that provoke or aggravate disorders systemic hemodynamics. To electrocardiographic criteria that increase the likelihood of diagnosing chronic HF in patients with relevant clinical symptoms,
include: cicatricial changes in the myocardium, blockade of the left leg of the His bundle, signs of left ventricular hypertrophy and left atrial overload, AF and various variants of tachy-,
bradyarrhythmias.
Chest x-ray is of lesser value in the diagnosis of chronic HF. However, this research method makes it possible to identify indirect signs of damage and dysfunction of the heart, the main of which are: cardiomegaly (increased
cardiothoracic index up to values of more than 50%), venous congestion in the lungs, interstitial or alveolar pulmonary edema.
Echocardiography plays a leading role in the diagnosis of chronic HF. This method makes it possible to detect cardiac dysfunction and determine its nature, quantify global and regional myocardial contractility, determine the size of cavities and
the thickness of the walls of the heart, the diameters of the holes, the pressure in the cavities and main vessels, assess the state of the valvular apparatus and intracardiac hemodynamics, identify changes endocardium and pericardium. The main indicator characterizing systolic function
left ventricle, is the ejection fraction. Unconditionally normal values are considered of this indicator, exceeding 50%, is certainly low - values less than 40%. As
The recommended values of the fraction and ejection of the left ventricle are 8-45%,
calculated on the basis of the results of two-dimensional echocardiography according to Simpson. With the development of mitral regurgitation, normal values of the left ventricular ejection
fraction do not exclude a decrease in stroke volume and cardiac output. The diastolic properties of the left ventricle are assessed by Doppler echocardiography of the transmittal diastolic flow and the flow from the pulmonary veins. Dynamics of echocardiographic indicators reflecting the severity of systolic and diastolic dysfunction of the left
ventricle, is one of the important criteria for evaluating the effectiveness of the treatment of chronic CH.
To determine the volumes of the chambers and the thickness of the walls of the heart, the ejection fraction of the left
ventricle and the dynamics of its diastolic filling, other, more
more accurate than echocardiography, but less accessible imaging modalities: radioisotope angiography and magnetic resonance imaging. To exclude pulmonary genesis
shortness of breath when examining some patients, it is advisable to assess lung function. Stress tests are used in a comprehensive examination of patients with chronic
HF is not so much for verifying the diagnosis as for assessing changes in functional status, reflecting the effectiveness of therapeutic measures, and determining the prognosis. Most accurately, exercise tolerance reflects maximum oxygen uptake. The maximum oxygen uptake is the amount of oxygen uptake that is achieved
at a certain level of physical activity and does not increase with a subsequent increase in the load power. This indicator characterizes the functionality
cardiorespiratory system, since after reaching it, the additional energy required for the work of skeletal muscles is formed due to anaerobic oxidation of glucose and
glycogenolysis.
179
Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
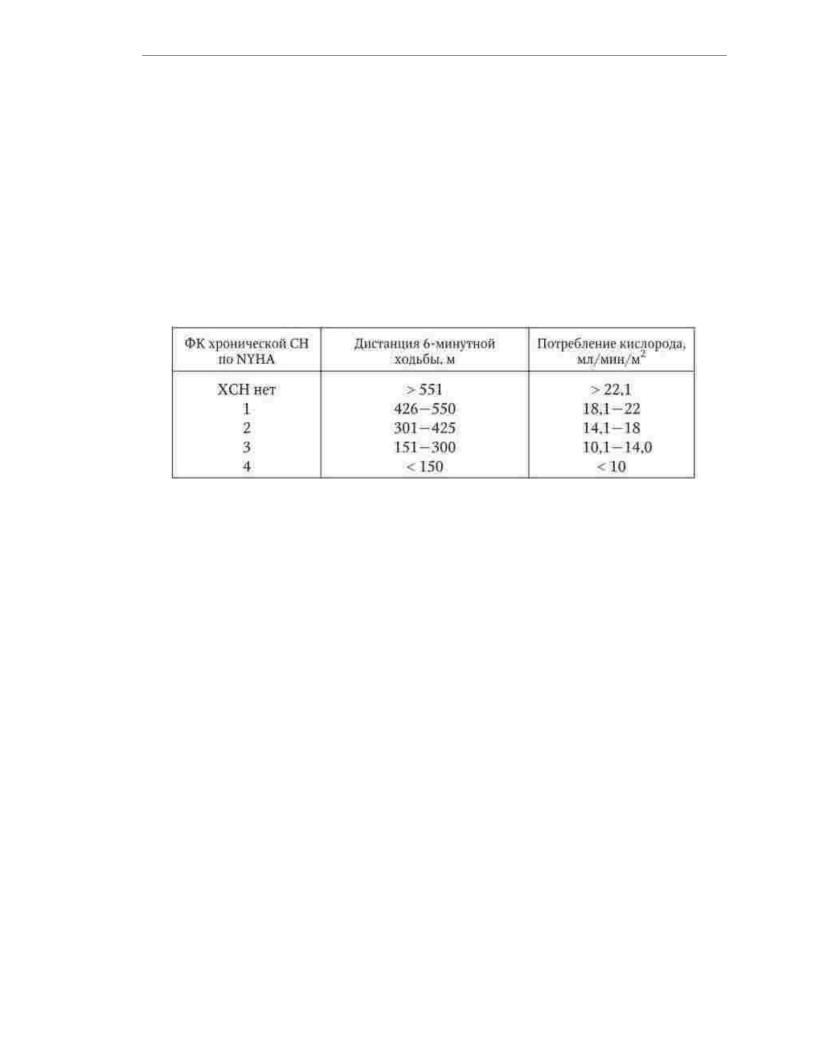
In everyday practice, when examining patients with chronic HF, it is recommended performing a 6-minute walk test. For the test, it is necessary to mark 1 m
long hospital corridor. The patient'stask is to walk the maximum possible distance along this corridor in 6 minutes. The pace of walking the patient chooses arbitrarily, with in the event of any discomfort associated with the load, it is allowed to reduce the speed of walking up to a complete stop, followed by the resumption of movement.
The distance covered by the patient in 6 minutes is closely correlated with the maximum intake oxygen. Results of the 6-minute walk test provide an objective assessment of tolerance
to physical activity (Table 1.30).
Table 1.30
Relationship between exercise tolerance and maximum oxygen consumption in patients with chronic heart failure of various functional classes
It should be emphasized that the diagnostic value of the test is reduced in the presence of additional reasons that limit the walking speed of the patient: angina
pectoris III-IV functional class, atherosclerosis of the arteries of the lower extremities, obstructive bro In a number of patients with coronary heart disease, additional instrumental
methods are used to determine the fact and degree of participation of coronary insufficiency in the genesis of chronic HF: ECG Holter monitoring, stress
echocardiography, positron emission tomography, and coronary angiography. To clarify the cause of cardiomegaly, ventriculography may be used. With chronic decompensation
HF and the development of acute HF to select and evaluate the effectiveness of therapy, an invasive method of monitoring the main hemodynamic parameters (cardiac output, "jamming" pressure in the pulmonary capillaries) using a Swan-Ganz catheter. In some cases, endomyocardial biopsy is used to confirm a possible association of chronic HF with inflammatory or toxic myocardial damage.
Diagnosis. The sequence of actions of a doctor in the process of diagnosing chronic heart failure shown in fig. 1.15.
If symptoms and/or clinical signs of chronic HF are detected, studies should be performed to obtain objective evidence of heart involvement (ECG registration, chest x- ray and, if possible, a study of the content of brain natriuretic hormone in the blood). In cases where the results
performed studies do not differ from the norm, the diagnosis of chronic HF is not enough
probable.
180
