
1-280 pdf (1)
.pdf
Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
When conducting differential diagnosis, it should be remembered that, in contrast to heart defects, patients with myxoma of the heart are uncharacteristic of a rheumatic history and any manifestations of anomalies in the development of the heart in childhood and
adolescence. In patients with myxoma, thromboembolism occurs, as a rule, against the background of sinus resistant to drug therapy, and signs of heart disease in most cases
combined with manifestations of the paraneoplastic process: general weakness, weight loss, arthralgia, subfebrile body temperature, inflammatory changes in peripheral blood.
Patients with hereditary myxoma often have comorbid cancers.
Surgical treatment. After removal of the tumor, the prognosis is favorable. In patients with sporadic myxoma, relapses are rare. Hereditary myxomas after
surgical treatment recur in 20% of cases.
1.10.2. Nonmyxomatous benign tumors
Fibroma is a benign connective tissue tumor that is localized predominantly in the myocardium of the anterior wall of the left ventricle and the interventricular septum. The tumor is a single nodule without a capsule. The main
clinical manifestations of fibroma are congestive heart failure resistant to drug treatment, disorders
rhythm and conduction.
Papillary fibroelastoma is a benign intracavitary tumor that is located on the endocardium (mainly papillary muscles, chords, heart valve cusps). As a rule, the tumor has a short stalk. Tumors can be either solitary or multiple. In children, the tumor is less common than in adults, and usually
located on the tricuspid valve. Adults are predominantly over 60 years of age.
damage to the mitral and aortic valves. Clinical manifestations of papillary fibroelastoma - chest pain, symptoms of thromboembolism of the vessels of the systemic circulation. A tumor located on the aortic valve can cause acute
coronary insufficiency.
Rhabdomyoma is a benign intramuscular tumor that is most often located in the interventricular septum and ventricular myocardium. As a rule, it has a plural character. The nodes of the tumor, growing, reduce the volume of the cavities of the heart. The main clinical manifestations are congestive heart failure and arrhythmias.
Lipoma is a benign tumor that, in addition to adipose tissue, may contain fibrous and muscle tissue. In most cases, the lipoma has subendocardial or subepicardial localization. Subendocardial lipoma with intraventricular growth presents with congestive heart failure, subepicardial lipoma causes symptoms
pericarditis.
The diagnosis of benign heart tumors is based on the results of echocardiography, computed tomography, and magnetic resonance imaging. treatment (if
when possible) surgical.
1.10.3. Sarcomas
According to morphological features, sarcomas can originate from various cellular heart elements. Cardiac sarcomas are characterized by rapid infiltrative growth with metastasis to the lymph nodes of the mediastinum, lungs, adrenal glands, liver, and brain. Most often, heart sarcoma is diagnosed at the age of 35 - 45 years and in men 2 times
more often than in women.
161

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
The main clinical manifestation of cardiac sarcoma is usually rapidly progressive heart failure. Due to the fact that the right chambers of the heart are more often affected, phenomena of right ventricular failure with effusion into the pericardial cavity, often with hemopericardium and signs of cardiac tamponade. In the early stages of the disease, most patients develop paraneoplastic syndrome (fatigue, fever, weight loss,
anemia, leukocytosis, an increase in ESR, the content of C-reactive protein and gamma globulins). ECG changes and chest radiographs are nonspecific. Tumor diagnosis
performed using two-dimensional echocardiography, computed tomography and magnetic resonance imaging.
For the treatment of patients, surgical, radiation and medicinal methods are used.
The prognosis is unfavorable.
1.10.4. Secondary malignant tumors
The development of secondary neoplasms in the heart is due either to metastasis or the germination of tumors from organs directly adjacent to the heart.
Most often in the heart metastasizes cancer of the bronchi, mammary glands, stomach, uterus, liver, as well as hypernephroma, melanoma, lymphoma. Metastatic heart disease can be
nodular and diffuse-infiltrative. In secondary cardiac tumors, metastases are usually
found in other internal organs.
Clinical manifestations of secondary heart tumors are similar to those of primary malignant neoplasms. In addition, signs of damage to the organs in which the primary tumor is localized are revealed. Diagnosis is based on
data from echocardiography, computed tomography and magnetic resonance imaging. Treatment of patients with secondary malignant tumors of the heart is symptomatic.
The complex of therapeutic measures includes chemotherapy and radiation therapy. When
a large amount of fluid accumulates in the pericardial cavity, a pericardial puncture is performed.
and drainage of its cavity, sometimes with the introduction of cytostatic drugs.
162

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
1.11. HEART FAILURE
Heart failure (HF) is a syndrome caused by inadequate blood supply to organs and tissues due to impaired pumping function of the heart. Distinguish
acute and chronic HF. The main pathophysiological mechanisms of deterioration in the propulsive capacity of the heart are a decrease in myocardial contractility (systolic dysfunction) and impaired myocardial relaxation (diastolic dysfunction). Term "circulatory failure" is considered obsolete and is no longer in common use.
lyatsya.
1.11.1. Acute heart failure
Definition. Acute heart failure is a clinical syndrome that develops as a result of the onset and rapid progression of cardiac dysfunction.
as a pump due to systolic or diastolic dysfunction, rhythm disturbances and
conduction of the heart, changes in preand afterload, damage to the valvular apparatus and
internal ruptures of the heart, tamponade of the pericardial cavity, which is manifested by stagnation in the small, large circles of blood circulation and a decrease in tissue perfusion.
Etiology. The main causes of acute HF are: decompensation of chronic HF, exacerbation of IHD (acute coronary syndrome), hypertensive crisis, acute arrhythmia, acute onset or worsening valvular regurgitation, severe aortic stenosis, severe acute myocarditis, cardiac tamponade, aortic dissection. Noncardiac factors that contribute to the development of acute HF include: poor
adherence to treatment, volume overload, infections (especially pneumonia and septicemia), sever stroke, major surgery, renal failure, bronchial
asthma, drug overdose, alcohol abuse, pheochromocytoma.
clinical options. There are several clinical variants of acute HF: acute decompensated HF (occurs due to decompensation of chronic HF, expressed
symptoms do not meet the diagnostic criteria for pulmonary edema and cardiogenic
shock, no signs of hypertensive crisis), hypertensive acute HF (occurs in patients with preserved systolic function of the left ventricle due to a pronounced increase in blood pressure, accompanied by radiographic signs of congestion in the pulmonary
circulation and / or symptoms of pulmonary edema), pulmonary edema, cardiogenic shock , acute high cardiac output (occurs in patients with septicemia, thyrotoxic crisis, anemia).
1.11.2. Pulmonary edema
Pulmonary edema is a clinical syndrome caused by acute left ventricular failure, arising either from a decrease in myocardial contractility (for example,
with the development of acute ischemia or MI), or due to an increase in afterload (increased BP, hypertensive crisis).
Due to a decrease in the contractility of the left ventricle occurs after
a gradual increase in pressure in the left atrium, veins, capillaries and arteries of the small
circulation circle. When the pressure in the pulmonary capillaries reaches the level of plasma colloid osmotic pressure, which is 26 - 30 mm Hg. Art., sweating of the
liquid part of the blood into the lung tissue begins - interstitial pulmonary edema develops. At further increase in pressure in the capillaries, the fluid enters the alveoli and develops
163
Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
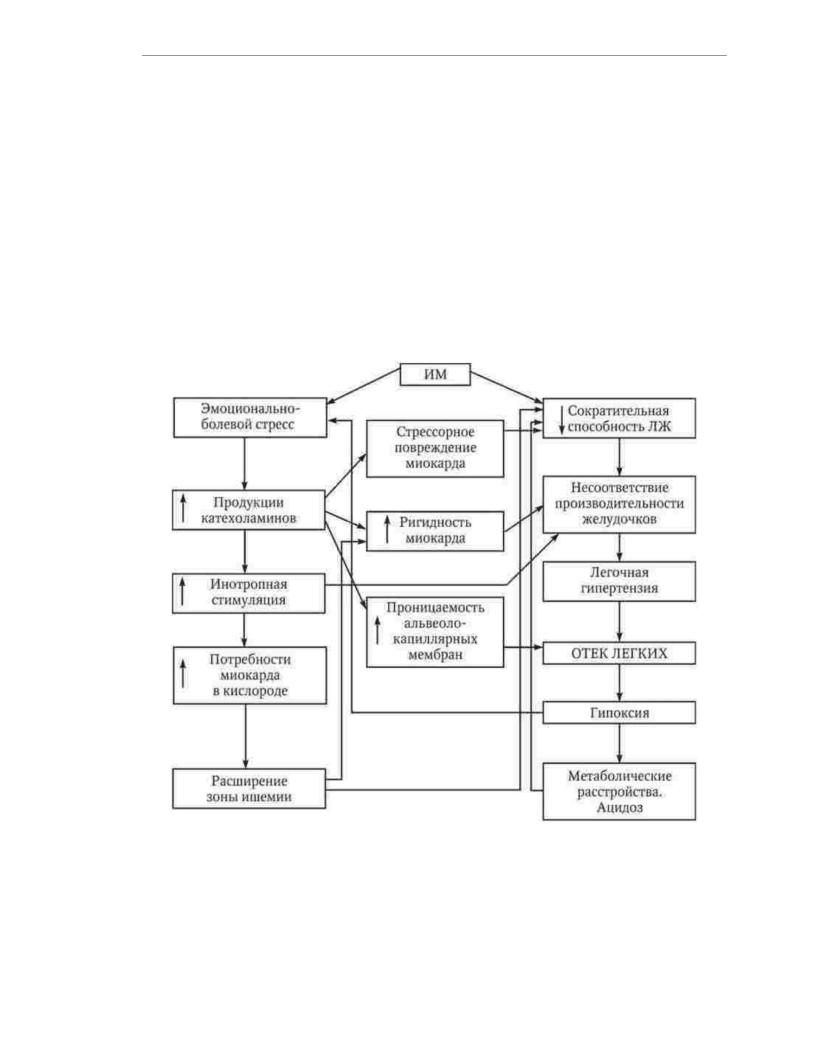
there is alveolar pulmonary edema. Of no small importance in the development of pulmonary edema is the activation of the sympathetic-adrenal system, due to psycho-emotional arousal due to increasing hypoxia and pain due to acute myocardial ischemia. Hypercatecholaminemia leads to an increase in blood pressure and heart rate, which contributes to an increase in myocardial oxygen demand, which may result in the development of myocardial ischemia or an expansion of the MI zone and a further decrease in the contractility of the left ventricle. In myocardial infarction, increased neurohumoral stimulation affects ventricular function differently: an unaffected right ventricle is able to increase its productivity to a greater extent than an infarcted left one, which is an additional reason for overflow of the pulmonary circulation. In the pathogenesis of pulmonary edema, diastolic dysfunction and an increase in afterload due to an increase in systemic blood pressure can play a significant role. In patients of this kind, pulmonary edema develops with relatively intact left ventricular function. The main links in the pathogenesis of pulmonary edema in MI are shown in Fig. 1.13.
Rice. 1.13. Pathogenesis of pulmonary edema in myocardial infarction
Interstitial pulmonary edema is manifested by an attack of cardiac asthma. Patients complain of a feeling of lack of air, shortness of breath, dry cough, tend to take a sitting position, show anxiety. On examination, attention is drawn to the pallor and often increased humidity of the skin, cyanosis of the lips. Characteristic symptoms of acute left ventricular failure are tachycardia, protodiastolic gallop rhythm, accent and bifurcation of the II tone on the pulmonary artery. At the stage of interstitial edema
164

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
percussion of the lungs reveals areas of dullness and a box shade of percussion
tone, with auscultation, dry rales are often heard, due to swelling of the bronchial mucosa. The development of alveolar pulmonary edema is characterized by increased
shortness of breath and cyanosis, the appearance of pink foamy sputum. In the lungs, Liberal moist rales are heard. With a detailed clinical picture of alveolar pulmonary edema
bubbling breath occurs with abundant formation of foam flowing from the oral cavity
and nasal passages.
The rate of development of alveolar pulmonary edema can vary significantly. In some patients with MI, it takes only a few minutes from the appearance of signs of congestion to the filling of the entire tracheobronchial tree with foam. Strive to recognize acute
left ventricular failure at the stage of interstitial pulmonary edema, when proper therapy can prevent the progression of the pathological process. For this
along with methods of physical examination, if time permits, it is advisable to use chest x-ray.
Pulmonary edema is a life-threatening condition that requires emergency
medical activities. Taking into account the peculiarities of pathogenesis, the main directions of treatment
of pulmonary edema are:
1) reduction of hydrostatic pressure in the pulmonary circulation by reducing
reduction of blood flow to the right ventricle;
2)weakening of neurohumoral stimulation of the heart;
3)increased propulsive capacity of the left ventricle;
4)elimination of hypoxia.
A patient with pulmonary edema should be given a half-sitting position with lowered legs, catheterize the central or peripheral vein, provide breathing with humidified oxygen with ethanol vapor through nasal catheters. With pronounced
increase in central venous pressure and rapidly progressive pulmonary edema, bloodletting is allowed in a volume of 300-500 ml. Prior to initiation of parenteral drug therapy
therapy at the level of systolic blood pressure more than 100 mm Hg. Art. nitroglycerin is used in
in the form of tablets, capsules or aerosol at a dose of 5 mg under the tongue every 5 to 10 minutes.
After providing access to the venous bed, morphine sulfate 2–4 mg, furosemide 20–80 mg are introduced, drip administration of nitroglycerin or isosorbide dinitrate is established.
The rate of infusion of nitropreparations is selected individually. Recommended initial
the rate of administration of nitroglycerin is 10 - 20 mcg / min. With rapidly progressive pulmonary edema, jet administration of nitroglycerin at a dose of 5–10 mg is allowed. Main
the criterion for determining the optimal infusion rate is systolic blood pressure, which
it is recommended to reduce by 10 - 15% of the initial level, but not lower than 90 mm Hg. Art. If the first the dose of furosemide does not give a clinical and diuretic effect, after 20-30 minutes the
injection of the drug is repeated at a double dose.
If tachyor bradyarrhythmias are the basis of pulmonary edema, they must be eliminated as as soon as possible with electrical cardioversion or pacing.
In cases where pulmonary edema develops against the background of hypertension, sodium niroprusside is administered intravenously. 50 g of the drug is dissolved in 500 ml of 5%
glucose solution. The initial infusion rate is not more than 25 µg/ min. Every 5 minutes the speed is increased by
10 mcg / min under the control of blood pressure, the level of which should not decrease by more than 25% of
original. Unlike nitroglycerin, sodium nitroprusside has no effect even in small doses. only venodilating, but also arteriodilating effect. In this regard, its positive effect on the propulsive ability of the left ventricle is more pronounced. Vme
However, it should be borne in mind that the use of sodium nitroprusside is associated with a risk
exacerbation of coronary insufficiency due to the phenomenon of stealing.
165

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
With an increase in blood pressure, the use of ganglionic blockers is possible. Pentamine 5 mg or benzohexonium at a dose of 2 mg, diluted in 20-40 ml of 5% glucose solution or isotonic
sodium chloride solution, injected intravenously over 5-10 minutes. The optimal dose of drugs is determined individually, taking into account the clinical effect and the level of blood pressure, which measured after the introduction of every 3 - 5 ml of solution.
With the appearance of symptoms of progressive cerebral hypoxia, a decrease in saturation of arterial blood with oxygen up to 90%, a drop in oxygen tension in arterial blood up to 60 mm Hg. Art., an increase in the tension of carbon dioxide in the blood and an increase in acidosis, it is recommended to intubate the trachea and perform mechanical artificial ventilation of the lungs with a positive end-expiratory pressure. In cases where, for any
For reasons it is not possible to provide adequate ventilation of the lungs, it is possible to use alkalizing solutions. However, in order to avoid iatrogenic alkalosis, complete correction of the base deficiency is not recommended.
Improvement of myocardial contractility in patients with acute coronary syndromes, complicated by acute left ventricular failure, is achieved by reducing
ischemia of the heart muscle. For this purpose, agents are used that provide hemodynamic unloading of the heart (peripheral vasodilators, diuretics) and restore
coronary blood flow (thrombolytics, mechanical revascularization). Cardiac glycosides in the
treatment of pulmonary edema are not only ineffective, but also dangerous, since with a high frequency cause ventricular arrhythmias and, due to inotropic stimulation, can contribute to the expansion
of the zone of myocardial necrosis. The basis for the trial use of cardiac glycosides can only be a combination of pulmonary edema with a tachysystolic form of atrial fibrillation.
1.11.3. Cardiogenic shock
Cardiogenic shock is the most severe form of acute HF. The term "cardiogenic shock" refers to a state of tissue hypoperfusion due to a decrease in cardiac
overshoot that persists after preload correction. Cardiogenic shock does not include cases of low cardiac output syndrome associated with hypovolemia, vasovagal
reactions, electrolyte disturbances, side effects of drug therapy, tachy and bradyarrhythmias.
A pronounced decrease in cardiac output in patients with MI may be due to
only by a drop in myocardial contractility, but also by other reasons: hypovolemia (due to with a reflex vascular response to pain), bradycardia (for example, due to complete atrioventricular blockade), a sharp increase in heart rate (with ventricular tachycardia or tachysystolic form of atrial fibrillation). In this regard, in practice, the diagnosis
cardiogenic shock is often established by exclusion, when the symptoms do not disappear
after elimination of hypovolemia and normalization of the heart rhythm. In patients with extensive MI, covering 40 - 50% of the mass of the left ventricle, a decrease in cardiac output can
have mixed genes.
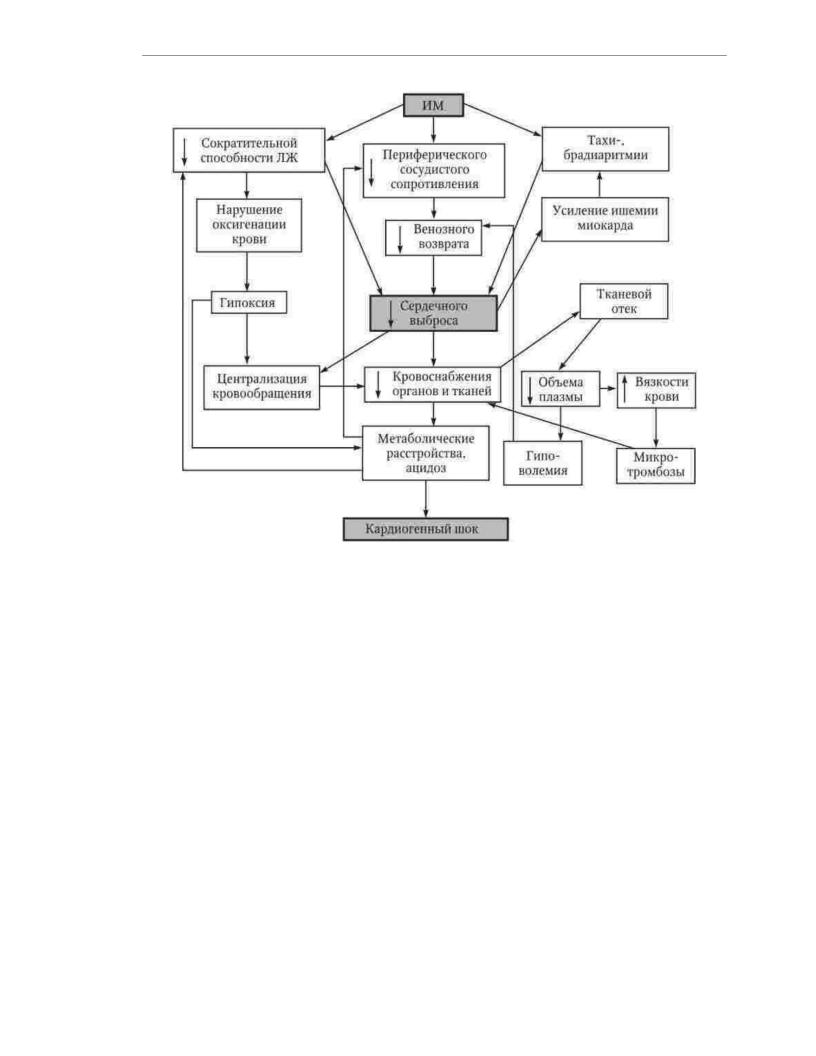
The scheme of the pathogenesis of cardiogenic shock in MI is shown in Fig. 1.14.
166
Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
Rice. 1.14. Pathogenesis of cardiogenic shock in myocardial infarction
A sharp decrease in cardiac output causes spasm of peripheral vessels. Centralization of blood circulation allows for some time to maintain adequate level of blood supply to vital organs. However, hypoperfusion of peripheral organs and tissues develops. Microcirculation disorders are exacerbated due to
with an increase in blood viscosity, increased aggregation of blood cells, the
formation of multiple microthrombi and the development of tissue edema. As a result, there are metabolic disorders, the progression of which is facilitated by a deterioration in
blood oxygenation due to a decrease in pulmonary blood flow and the formation of arteriovenous shunts in the pulmonary circulation. Tissue hypoxia causes dilatation of arterioles and increased blood deposition in the periphery. The resulting decrease
venous return leads to a further decrease in cardiac output. Violation of the blood supply to vital organs leads to functional disorders:
glomerular filtration, dyscirculatory encephalopathy and liver failure develop. A drop in diastolic blood pressure leads to a decrease in coronary perfusion, which
creates the prerequisites for the expansion of zones of necrosis and myocardial ischemia, the occurrence of
rhythm and conduction. As metabolic acidosis progresses, further inhibition of the propulsive ability of the heart.
Acute vascular insufficiency associated with MI with severe pain syndrome is often combined with sinus bradycardia. Vascular collapse can lead to tissue hypoxia and impaired perfusion of vital organs, however, in most
cases, it is not accompanied by generalized microcirculation disorders and
167
Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
development of multiple organ failure, characteristic of cardiogenic shock. Hemodynamically significant arrhythmias and conduction disturbances in case of their timely and effective treatment also do not lead to severe microcirculation disorders. elimination
arrhythmia, as a rule, is accompanied by normalization of blood pressure. In contrast to hypotension of arrhythmic origin in cardiogenic shock, combined with severe arrhythmias and conduction, restoration of sinus rhythm with normal heart rate does not provide
normalization of hemodynamics, since the main cause of circulatory disorders is a critical decrease in the mass of the effectively contracting myocardium.
The development of cardiogenic shock is accompanied by increasing weakness and adynamism of the patient, facial features are sharpened, the skin becomes pale cyanotic. coloration, sweating increases. With a detailed clinical picture, signs of a sharp deterioration in peripheral circulation are revealed: cold, wet hands and
feet, marble cyanotic color of the skin of the distal extremities. The pulse on the radial arteries is threadlike or not palpable, often arrhythmic. systolic blood pressure as usually falls below 80 mm Hg. Art. However, in patients with HD, cardiogenic shock
can develop at blood pressure levels exceeding 90 and even 100 mm Hg. Art. At the same time persons with initial hypotension, a decrease in systolic blood pressure to 80 mm Hg. Art.
may not be accompanied by a clinical picture of shock. A more reliable diagnostic sign of cardiogenic shock is a decrease in pulse pressure to 20 mm Hg. Art. On auscultation muffled heart sounds, protodiastolic gallop and often congestive rales in
posterior regions of the lungs. The characteristic signs of cardiogenic shock include oligouria (reduced diuresis to 20 ml/h) or anuria. Shock is always accompanied by a shift in the acid-base state towards acidosis and often by changes in biochemical parameters characterizing the function of the liver, kidneys, pancreas, which is disturbed.
due to poor blood supply to internal organs.
Cardiogenic shock and hypovolemic shock have similar clinical symptoms, but the methods of their medical correction are fundamentally different. A confident distinction between these clinical conditions is based on the results of a hemodynamic study. The
cardiac index in patients of both categories, as a rule, is reduced to 1.8 l / min / m2 and less, but the value of "jamming" pressure in the capillaries of the lungs, which is normally 18 mm Hg. Art., differ significantly. In cardiogenic shock, the value of this indicator increases to values above 20 mm Hg. Art., with hypovolemic shock - decreases
to values less than 15 mm Hg. Art. For prompt assessment of key hemodynamic parameters necessary for diagnosing the state of blood circulation and selecting doses of
vasoactive drugs, patients with signs of shock are recommended to install in the pulmonary artery floating Swan-Ganz catheter.
Cardiogenic shock is a severe disorder of systemic hemodynamics and microcirculation, the treatment of which is often unsuccessful. However, active therapeutic measures at the initial stage of development of cardiogenic shock, when
hypoperfusion of vital organs has not yet led to the development of irreversible changes, allows interrupt the chain of pathological events ending in the death of the patient.
The main tasks of treating a patient with cardiogenic shock include the following: 1) correction of central hemodynamic disorders and restoration of contractile
myocardial function;
2)maintaining adequate systemic perfusion and blood supply to vital
organs;
3)prevention of microcirculation disorders;
4)correction of the acid-base state.
168

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
Basic management of cardiogenic shock includes humidified oxygen through nasal catheters or through a mask, central venous catheterization,
adequate pain relief, the use of antithrombotic drugs and (in the absence of contraindications) thrombolytic therapy. It must be emphasized that effective
thrombolysis in a number of patients can significantly improve the function of the heart as a pump. The anti-shock effect of thrombolytic therapy is associated with the restoration of perfusion and functional activity of the myocardial region that has not lost its viability. In connection with Therefore, in the treatment of patients with cardiogenic shock, thrombolysis should be sought
as early as possible - if possible at the pre-hospital stage. If, against the background of oxygen inhalation, its tension in the arterial blood does not exceed 60 mm Hg. Art., it is advisable to perform tracheal intubation and continue oxygen therapy by artificial artificial
lung ventilation. For a reasonable choice and evaluation of the effectiveness of therapy, it is necessary ensure control of indicators of the acid-base state and parameters of the central
hemodynamics.
In the presence of hemodynamic signs of hypovolemia, the patient is placed on the bed with the headrest lowered, provide an elevated position of the lower extremities and
produce a rapid (within 10 minutes) intravenous injection of 150-300 ml of plasma-substituting solutions (reopoliglyukin, 5% glucose solution, isotonic chloride solution
sodium). In the absence of changes in blood pressure and central hemodynamic parameters in response to the introduction of fluid is carried out by repeated infusion of plasma substitutes in a volume of 200 ml
in 10 min. Then again control hemodynamic parameters. If "jamming"
pressure in the pulmonary capillaries does not increase, the infusion of plasma substitutes is continued with speed 500 ml/h. With an increase in "jamming" pressure in the pulmonary capillaries
the infusion must be stopped immediately, as further administration of fluid may
cause pulmonary edema. In cases where preload optimization is not accompanied by an increase
in cardiac index and blood pressure, therapeutic measures are supplemented with infusion of sympathomimetic amines.
With extremely low blood pressure, treatment begins with the introduction of norepinephrine at a rate of 2 -
10 µg/ min. Since norepinephrine is a stimulant of both betaand ÿ- adrenergic receptors, when it is used, stimulation of the left ventricular pumping function is combined with an increase in afterload, and an increase in blood pressure is often not accompanied by an increase in pulse rate.
pressure. As the dose of administered norepinephrine increases, its stimulating effect on ÿ- adrenergic receptors increases, which increases the risk of developing (increasing)
stagnation in the pulmonary circulation and microcirculation disorders. In addition, the introduction norepinephrine is associated with a high risk of cardiac arrhythmias.
Therefore, when systolic blood pressure reaches 80 mm Hg. Art., as well as in cases where this level of systolic blood pressure is determined at baseline, the preferred treatment
cardiogenic shock is dopamine.
Dopamine stimulates ÿ- adrenergic receptors more strongly than ÿ- adrenergic receptors, and at a therapeutic dose, compared with norepinephrine, causes less pronounced peripheral vasoconstriction. An additional positive property of dopamine is its stimulating effect on specific dopaminergic receptors, due to which
vasodilation of the kidneys, mesentery, heart and brain. This effect develops at a speed
administration of dopamine 1 - 5 mcg / kg / min, with which the infusion of the drug is usually started. When insufficient efficiency (systolic blood pressure remains below 90 mm Hg. Art.)
the speed is increased to 5 - 10 mcg / kg / min. The vasodilatory effect of dopamine its ââ2iá- adrenostimulating effect gradually weakens and intensifies , as a result which is constriction of peripheral vessels. In patients with refractory hypotension
possible temporary administration of dopamine at a rate of 20-50 mcg / kg / min, as well as combined
169

Machine Translated by Google
. The team of authors. "Internal illnesses. Volume 1"
the use of dopamine and norepinephrine. As the rate of dopamine infusion increases, the age
melts the risk of tachycardia, extrasystole and increased myocardial ischemia.
In the absence of severe arterial hypotension or drug stabilization
systolic blood pressure at a level of more than 90 mm Hg. Art. preferred drug from the group sympathomimetic amine is dobutamine (dobutrex). This connection works
predominantly on ÿ1adrenergic receptors. Possessing a distinct inotropic effect, dobutamine has a weaker effect than dopamine on heart rate and ectopic activity. Recommended
the initial infusion rate of dobutamine is 2.5 mcg/kg/min. If necessary, the rate of administration can be increased by 2.5 µg/ kg/min every 10 to 30 minutes up to 20 µg/ kg/min.
Increased "jamming" pressure in the pulmonary capillaries more than 20 mm Hg. Art., as
as a rule, it is combined with stagnation in a small circle of blood circulation. In these cases, along with infusion of sympathomimetic amines, nitropreparations should be administered intravenously.
The rate of infusion of nitroglycerin and isosorbide dinitrate, depending on the specific clinical situation, can vary over a very wide range: from 10 to 200 µg/ min. The criterion for achieving the optimal speed is the reduction of the "jamming" pressure in
pulmonary capillaries to values less than 20 mm Hg. Art. and reducing the severity of stagnation in
lungs.
Treatment of cardiogenic shock in right ventricular MI begins with the introduction of
plasma substitutes. If volume-replenishing therapy does not lead to an increase in blood pressure and an incre cardiac index, treatment is supplemented with dobutamine. The introduction of nitropreparations
can aggravate the condition of a patient with cardiogenic shock due to right ventricular MI. The use of short-acting nitrates (nitroglycerin) with careful selection of speed
infusion is justified only in cases of a combination of right ventricular and left ventricular failure
sufficiency.
With the development of cardiogenic shock refractory to drug therapy, as well as cardiogenic shock due to anatomical damage to the heart (acute mitral regurgitation, rupture of the interventricular septum), the patient'scondition may be temporarily
stabilized with intra-aortic balloon counterpulsation. This method
consists in changing the volume of an elastic balloon inserted into the descending thoracic aorta, which is synchronized with the work of the heart. During diastole, the balloon inflates which provides an increase in pressure in the aorta and improved myocardial perfusion. During systole, the balloon collapses, resulting in reduced afterload and easier expulsion
blood from the left ventricle. without any significant positive effect on long-term prognosis in cardiogenic shock, circulatory support allows you to prepare
patient for coronary balloon angioplasty or coronary bypass surgery. According to modern concepts, myocardial revascularization performed in
as soon as possible after the development of MI, is the most effective means
treatment of cardiogenic shock.
1.11.4. Chronic heart failure
Definition. Chronic heart failure is a pathophysiological
a syndrome that develops as a result of a violation of the ability of the heart to fill and / or emptying, occurring in conditions of imbalance of vasoconstrictor and vasodilatory neurohumoral systems, accompanied by inadequate perfusion of organs and
body tissues and manifested by a complex of symptoms: shortness of breath, weakness, increased fatigue and fluid retention in the body (edematous syndrome).
The development of chronic heart failure occurs according to uniform pathophysiological laws outside
depending on the etiology, which gives reason to consider this condition not only as a complex
170
