

Manuscript Author
Manuscript Author
Manuscript Author
Manuscript Author
Hsich |
Page 9 |
Another consideration is to create an allocation score. This would change a rule based” system to an “algorithmic based” system. Algorithmic based systems can predict waitlist mortality, such as the Model for End-Stage Liver Disease (MELD score) used for liver transplantation. 54 They can also be constructed to predict both pre-and post-transplant mortality to minimize death on the waitlist and yet prevent futility, such as the lung allocation score (LAS score) for lung transplantation.55 In order to create an algorithmic based allocation system, risk factors must be identified. This task is possible but would be substantial given the number of high-risk groups potentially present and possible interactions with many variables.
Geographic disparity can be reduced by either transporting people or organs across current UNOS regions. Relocating organs may be possible. However; relocating patients is often limited to more affluent individuals, which raises ethical concerns given the need to keep organ allocation fair and equitable to all. Another alternative to reducing geographic disparity is to broaden sharing or reorganize regions to better match the population density with donor availability. The liver transplant allocation system is considering restructuring their program from 11 regions to either 4 or 8 in order to better match organs with high priority recipients. All these attempts have the potential to reduce waitlist mortality but ultimately just rearrange the existing structure. Additional options are needed to make more substantial changes to matching the market.
Ventricular assist devices (VADs) provide an important alternative to transplantation. They have been proven to extend life for both women and men with advanced heart failure48 and shown to be superior to medical therapy for Interagency Registry for Mechanically Assisted Circulatory Support (INTERMACS) level 4-7.65 Currently, devices are implanted for bridge to transplant and less frequently as destination therapy.66 In fact, many who are “labeled as destination therapy” are later switched to bridge to transplantation.67 The lack of enthusiasm for embracing VADs as permanent alternatives to transplantation is due to the risk of pump thrombosis, stroke and driveline infections.66, 68 So who should receive VADs as an alternative to transplantation? VADs are indicated for patients who are INTERMACS profile 4 or worse, with consistent symptoms of heart failure at rest or minimal activity. The use of VADs or listing for transplantation should also be considered in INTERMACS Profile 5 patients, who are comfortable at rest but have minimal functional reserve, as documented by peak VO2 less than 12-14 ml/kg/min. More research will need to be done to better identify this cohort.
Conclusion
Strategies to better match the market for heart transplantation are necessary to enable a scarce resource to be maximally utilized. There are 3 ways to achieve this goal: 1) increase the donor pool, 2) reduce the waitlist, and 3) improve the allocation system. Although it is easier to focus national efforts on only one strategy, all must be done simultaneously to ensure that the growth of the waitlist matches the number of available donors. Advances in technology should provide better opportunity to engage young people to become organ donors such as Facebook.28 Other social media needs to be explored and more successful programs like state revenue reserved for donation recruitment needs to be encouraged.18
Circ Heart Fail. Author manuscript; available in PMC 2017 June 05.

Manuscript Author
Manuscript Author
Manuscript Author
Manuscript Author
Hsich |
Page 10 |
Minority groups need to be considered separately and successful programs like Dow-Tip should be replicated. These efforts will increase the number of potential donors that “Opt In.” Although it is not clear which method is best in the United States, it is clear that the best donor is young and healthy. Family members are likely to be distraught and surprised when a young person dies and less likely to donate organs voluntarily. Therefore, it may be best to figure out how to have more of these potential donors “Opt In” and make it clear prior to death their wishes to be an organ donor. The waitlist also needs to be reduced and strict uniform criteria based on outcome data will need to be utilized. This will likely be the most difficult aspect. Just because we can transplant a patient with multiple co-morbidities or tobacco abuse we need to remember that we have a limited resource that should be distributed to only those with the best outcome for success. Finally, efforts to improve the allocation system need to be embraced. Objective data to define tiers in my opinion will prevent “gaming the system” and research needs to be done to better determine optimal timing for urgent transplantation in high risk groups like restrictive cardiomyopathy. Alternatives to transplant like the usage of VADs should be considered, especially once patients are identified that have similar survival with either option. Finally, collaboration between many medical and community participants will be vital in order to begin the rematch between supply and demand as we strive for more effective allocation of the scarce resource of human hearts for transplantation.
Supplementary Material
Refer to Web version on PubMed Central for supplementary material.
Acknowledgements
A special thank you to Dr. Lynne Stevenson, who provided suggestions and the inspiration to write this review.
Sources of Funding
Supported by the National Heart, Lung and Blood Institute of the National Institute of Health under Award Number R56HL125420-01A1. The content is solely the responsibility of the author and does not necessarily represent the official views of the National Institutes of Health.
Abbreviations
DOW-TIP Dow Take Initiative Program
HDS Heart Donor Score
HOTA Human Organ Transplant Act
HRSA Health Resources and Services Administration
INTERMACSInteragency Registry for Mechanically Assisted Circulatory Support
OPTN Organ Procurement and Transplantation Network
SRTR Scientific Registry of Transplant Recipients
UNOS United Network for Organ Sharing
Circ Heart Fail. Author manuscript; available in PMC 2017 June 05.

Manuscript Author
Manuscript Author
Manuscript Author
Manuscript Author
Hsich |
Page 11 |
US |
United States |
VADs |
Ventricular Assist Devices |
References
1.Lund LH, Edwards LB, Kucheryavaya AY, Dipchand AI, Benden C, Christie JD, Dobbels F, Kirk R, Rahmel AO, Yusen RD, Stehlik J. The registry of the international society for heart and lung transplantation: Thirtieth official adult heart transplant report--2013; focus theme: Age. J Heart Lung Transplant. 2013; 32:951–964. [PubMed: 24054804]
2.Stinson EB, Dong E Jr. Schroeder JS, Harrison DC, Shumway NE. Initial clinical experience with heart transplantation. Am J Cardiol. 1968; 22:791–803. [PubMed: 4880224]
3.U.S. Department of Health and Human Services. [June 19, 2015] Timeline of Historical Events Significant Milestones in Organ Donation and Transplantaton. Available at http:// www.organdonor.gov/legislation/timeline.html
4.Mudge GH, Goldstein S, Addonizio LJ, Caplan A, Mancini D, Levine TB, Ritsch ME Jr. Stevenson LW. 24th bethesda conference: Cardiac transplantation. Task force 3: Recipient guidelines/ prioritization. J Am Coll Cardiol. 1993; 22:21–31. [PubMed: 8509544]
5.O'Connell JB, Bourge RC, Costanzo-Nordin MR, Driscoll DJ, Morgan JP, Rose EA, Uretsky BF. Cardiac transplantation: Recipient selection, donor procurement, and medical follow-up. A statement for health professionals from the committee on cardiac transplantation of the council on clinical cardiology, american heart association. Circulation. 1992; 86:1061–1079. [PubMed: 1516181]
6.Mehra MR, Canter CE, Hannan MM, Semigran MJ, Uber PA, Baran DA, Danziger-Isakov L, Kirklin JK, Kirk R, Kushwaha SS, Lund LH, Potena L, Ross HJ, Taylor DO, Verschuuren EA, Zuckermann A. The 2016 international society for heart lung transplantation listing criteria for heart transplantation: A 10-year update. J Heart Lung Transplant. 2016; 35:1–23. [PubMed: 26776864]
7.Haller JD, Cerruti MM. Heart transplantion in man: Compilation of cases. January 1, 1964 to october 23, 1968. Am J Cardiol. 1968; 22:840–843. [PubMed: 4880230]
8.[february 4, 2016] Unos transplant trends: Transplants by organ type . Available at https:// www.Unos.Org/data/transplant-trends/
9.Rithalia A, McDaid C, Suekarran S, Myers L, Sowden A. Impact of presumed consent for organ donation on donation rates: A systematic review. BMJ. 2009; 338:a3162. [PubMed: 19147479]
10.Dave R, James C, Ahmad N. Expanding organ donation in the uk: Ethical, moral and logistical dilemmas. Br J Hosp Med (Lond). 2013; 74:512–517. [PubMed: 24022552]
11.Rieu R. The potential impact of an opt-out system for organ donation in the uk. J Med Ethics. 2010; 36:534–538. [PubMed: 20817820]
12.Kwek TK, Lew TW, Tan HL, Kong S. The transplantable organ shortage in singapore: Has implementation of presumed consent to organ donation made a difference? Ann Acad Med Singapore. 2009; 38:346–348. [PubMed: 19434338]
13.Gonzalez-Vilchez F, Gomez-Bueno M, Almenar L, Crespo-Leiro MG, Arizon JM, Palomo J, Delgado J, Roig E, Lage E, Manito N. Spanish heart transplantation registry. 25th official report of the spanish society of cardiology working group on heart failure and heart transplantation (1984-2013). Rev Esp Cardiol (Engl Ed). 2014; 67:1039–1051. [PubMed: 25455756]
14.Matesanz R. Spain: A leader in harvesting hearts for transplantation. Circulation. 2007; 115:f45–
46.[PubMed: 17378021]
15.Bramhall S. Presumed consent for organ donation response. Ann R Coll Surg Engl. 2011; 93:565–
565.[PubMed: 22128399]
16.del Rio Gallegos F, Nunez Pena JR, Soria Garcia A, Moreno Roy MA, Varela A, Calatayud J. Non heart beating donors. Succesfully expanding the donor's pool. Ann Transplant. 2004; 9:19–20.
17.Lavee J, Brock DW. Prioritizing registered donors in organ allocation: An ethical appraisal of the israeli organ transplant law. Curr Opin Crit Care. 2012; 18:707–711. [PubMed: 22914426]
Circ Heart Fail. Author manuscript; available in PMC 2017 June 05.

Manuscript Author
Manuscript Author
Manuscript Author
Manuscript Author
Hsich |
Page 12 |
18.Chatterjee P, Venkataramani AS, Vijayan A, Wellen JR, Martin EG. The effect of state policies on organ donation and transplantation in the united states. JAMA Intern Med. 2015; 175:1323–1329. [PubMed: 26030386]
19.Khatami SM, Mahdavi-Mazdeh M. Perfect is the enemy of good: The iranian system of paid donation. Am J Transplant. 2014; 14:1222–1223. [PubMed: 24618409]
20.Gordon EJ, Gill JS. Where there is smoke there is fire: The iranian system of paid donation. Am J Transplant. 2013; 13:3063–3064. [PubMed: 24224692]
21.Einollahi B. Cadaveric kidney transplantation in iran: Behind the middle eastern countries? Iran J Kidney Dis. 2008; 2:55–56. [PubMed: 19377209]
22.Zuniga-Fajuri A. Increasing organ donation by presumed consent and allocation priority: Chile. Bull World Health Organ. 2015; 93:199–202. [PubMed: 25767299]
23.Kransdorf EP, Stehlik J. Donor evaluation in heart transplantation: The end of the beginning. J Heart Lung Transplant. 2014; 33:1105–1113. [PubMed: 25012979]
24.The organ donation breakthrough collaborative: Best practices final report (september 2003). Nephrol Nurs J. 2003; 30:529–531, 590-521. [PubMed: 14621632]
25.Callender CO, Bey AS, Miles PV, Yeager CL. A national minority organ/tissue transplant education program: The first step in the evolution of a national minority strategy and minority transplant equity in the USA. Transplant Proc. 1995; 27:1441–1443. [PubMed: 7878936]
26.Ganikos ML, McNeil C, Braslow JB, Arkin EB, Klaus D, Oberley EE, White MF. A case study in planning for public health education: The organ and tissue donation experience. Public Health Rep. 1994; 109:626–631. [PubMed: 7938382]
27.[june 18, 2015] The reports of the surgeon general. 1991. Available at http:// profiles.Nlm.Nih.Gov/ps/retrieve/resourcemetadata/nnbcyz/p-segmented/true
28.Cameron AM, Massie AB, Alexander CE, Stewart B, Montgomery RA, Benavides NR, Fleming GD, Segev DL. Social media and organ donor registration: The facebook effect. Am J Transplant. 2013; 13:2059–2065. [PubMed: 23777475]
29.Ison MG, Hager J, Blumberg E, Burdick J, Carney K, Cutler J, Dimaio JM, Hasz R, Kuehnert MJ, Ortiz-Rios E, Teperman L, Nalesnik M. Donor-derived disease transmission events in the united states: Data reviewed by the optn/unos disease transmission advisory committee. Am J Transplant. 2009; 9:1929–1935. [PubMed: 19538493]
30.Brieke A, Krishnamani R, Rocha MJ, Li W, Patten RD, Konstam MA, Patel AR, Udelson JE, Denofrio D. Influence of donor cocaine use on outcome after cardiac transplantation: Analysis of the united network for organ sharing thoracic registry. J Heart Lung Transplant. 2008; 27:1350– 1352. [PubMed: 19059117]
31.Xu DS, Hartman D, Ludrosky K, Campbell J, Starling RC, Taylor DO, Smedira NG, GonzalezStawinski GV. Impact of donor high-risk social behaviors on recipient survival in cardiac transplantation. Transplantation. 2010; 89:873–878. [PubMed: 20090571]
32.Wever Pinzon O, Stoddard G, Drakos SG, Gilbert EM, Nativi JN, Budge D, Bader F, Alharethi R, Reid B, Selzman CH, Everitt MD, Kfoury AG, Stehlik J. Impact of donor left ventricular hypertrophy on survival after heart transplant. Am J Transplant. 2011; 11:2755–2761. [PubMed: 21906259]
33.Stehlik J, Feldman DS, Brown RN, VanBakel AB, Russel SD, Ewald GA, Hagan ME, Folsom J, Kirklin JK. Interactions among donor characteristics influence post-transplant survival: A multiinstitutional analysis. J Heart Lung Transplant. 2010; 29:291–298. [PubMed: 19804989]
34.Khush KK, Zaroff JG, Nguyen J, Menza R, Goldstein BA. National decline in donor heart utilization with regional variability: 1995-2010. Am J Transplant. 2015; 15:642–649. [PubMed: 25676093]
35.Weiss ES, Allen JG, Kilic A, Russell SD, Baumgartner WA, Conte JV, Shah AS. Development of a quantitative donor risk index to predict short-term mortality in orthotopic heart transplantation. J Heart Lung Transplant. 2012; 31:266–273. [PubMed: 22093382]
36.Smits JM, De Pauw M, de Vries E, Rahmel A, Meiser B, Laufer G, Zuckermann A. Donor scoring system for heart transplantation and the impact on patient survival. J Heart Lung Transplant. 2012; 31:387–397. [PubMed: 22177692]
Circ Heart Fail. Author manuscript; available in PMC 2017 June 05.

Manuscript Author
Manuscript Author
Manuscript Author
Manuscript Author
Hsich |
Page 13 |
37.Zaroff JG, Rosengard BR, Armstrong WF, Babcock WD, D'Alessandro A, Dec GW, Edwards NM, Higgins RS, Jeevanandum V, Kauffman M, Kirklin JK, Large SR, Marelli D, Peterson TS, Ring WS, Robbins RC, Russell SD, Taylor DO, Van Bakel A, Wallwork J, Young JB. Consensus conference report: Maximizing use of organs recovered from the cadaver donor: Cardiac recommendations, march 28-29, 2001, crystal city, va. Circulation. 2002; 106:836–841. [PubMed: 12176957]
38.Nixon JL, Kfoury AG, Brunisholz K, Horne BD, Myrick C, Miller DV, Budge D, Bader F, Everitt M, Saidi A, Stehlik J, Schmidt TC, Alharethi R. Impact of high-dose inotropic donor support on early myocardial necrosis and outcomes in cardiac transplantation. Clin Transplant. 2012; 26:322– 327. [PubMed: 21981698]
39.Colvin-Adams M, Smith JM, Heubner BM, Skeans MA, Edwards LB, Waller CD, Callahan ER, Snyder JJ, Israni AK, Kasiske BL. Optn/srtr 2013 annual data report: Heart. Am J Transplant. 2015; 15(Suppl 2):1–28.
40.Stevenson LW. Crisis awaiting heart transplantation: Sinking the lifeboat. JAMA Intern Med. 2015; 175:1406–1409. [PubMed: 26030521]
41.[june 7, 2015] The international society for heart and lung transplantation: 2014 slides for adult heart transplantation statistics. Available at https://www.Ishlt.Org/registries/slides.Asp? Slides=heartlungregistry
42.Khanna AK, Xu J, Uber PA, Burke AP, Baquet C, Mehra MR. Tobacco smoke exposure in either the donor or recipient before transplantation accelerates cardiac allograft rejection, vascular inflammation, and graft loss. Circulation. 2009; 120:1814–1821. [PubMed: 19841304]
43.Corbett C, Armstrong MJ, Neuberger J. Tobacco smoking and solid organ transplantation. Transplantation. 2012; 94:979–987. [PubMed: 23169222]
44.Lietz K, Miller LW. Improved survival of patients with end-stage heart failure listed for heart transplantation: Analysis of organ procurement and transplantation network/u.S. United network of organ sharing data, 1990 to 2005. J Am Coll Cardiol. 2007; 50:1282–1290. [PubMed: 17888847]
45.Barr ML, Taylor DO. Changes in donor heart allocation in the united states without fundamental changes in the system: Rearranging deck chairs and elephants in the room. Am J Transplant. 2015; 15:7–9. [PubMed: 25534539]
46.Dardas T, Mokadam NA, Pagani F, Aaronson K, Levy WC. Transplant registrants with implanted left ventricular assist devices have insufficient risk to justify elective organ procurement and transplantation network status 1a time. J Am Coll Cardiol. 2012; 60:36–43. [PubMed: 22541833]
47.Meyer DM, Rogers JG, Edwards LB, Callahan ER, Webber SA, Johnson MR, Vega JD, Zucker MJ, Cleveland JC Jr. The future direction of the adult heart allocation system in the united states. Am J Transplant. 2015; 15:44–54. [PubMed: 25534445]
48.Hsich EM, Naftel DC, Myers SL, Gorodeski EZ, Grady KL, Schmuhl D, Ulisney KL, Young JB. Should women receive left ventricular assist device support?: Findings from intermacs. Circ Heart Fail. 2012; 5:234–240. [PubMed: 22260946]
49.Pitt B, Remme W, Zannad F, Neaton J, Martinez F, Roniker B, Bittman R, Hurley S, Kleiman J, Gatlin M. Eplerenone, a selective aldosterone blocker, in patients with left ventricular dysfunction after myocardial infarction. N Engl J Med. 2003; 348:1309–1321. [PubMed: 12668699]
50.Elmariah S, Goldberg LR, Allen MT, Kao A. Effects of gender on peak oxygen consumption and the timing of cardiac transplantation. J Am Coll Cardiol. 2006; 47:2237–2242. [PubMed: 16750689]
51.Bardy GH, Lee KL, Mark DB, Poole JE, Packer DL, Boineau R, Domanski M, Troutman C, Anderson J, Johnson G, McNulty SE, Clapp-Channing N, Davidson-Ray LD, Fraulo ES, Fishbein DP, Luceri RM, Ip JH. Amiodarone or an implantable cardioverter defibrillator for congestive heart failure. N Engl J Med. 2005; 352:225–237. [PubMed: 15659722]
52.Cleland JG, Daubert JC, Erdmann E, Freemantle N, Gras D, Kappenberger L, Tavazzi L. The effect of cardiac resynchronization on morbidity and mortality in heart failure. N Engl J Med. 2005; 352:1539–1549. [PubMed: 15753115]
53.Lund LH, Mancini D. Heart failure in women. Med Clin North Am. 2004; 88:1321–1345, xii. [PubMed: 15331319]
Circ Heart Fail. Author manuscript; available in PMC 2017 June 05.

Manuscript Author
Manuscript Author
Manuscript Author
Manuscript Author
Hsich |
Page 14 |
54.Kamath PS, Wiesner RH, Malinchoc M, Kremers W, Therneau TM, Kosberg CL, D'Amico G, Dickson ER, Kim WR. A model to predict survival in patients with end-stage liver disease. Hepatology. 2001; 33:464–470. [PubMed: 11172350]
55.Egan TM, Murray S, Bustami RT, Shearon TH, McCullough KP, Edwards LB, Coke MA, Garrity ER, Sweet SC, Heiney DA, Grover FL. Development of the new lung allocation system in the united states. Am J Transplant. 2006; 6:1212–1227. [PubMed: 16613597]
56.Singh TP, Almond CS, Taylor DO, Milliren CE, Graham DA. Racial and ethnic differences in waitlist outcomes in patients listed for heart transplantation in the united states. Circulation. 2012; 125:3022–3030. [PubMed: 22589383]
57.Hsich EM, Starling RC, Blackstone EH, Singh TP, Young JB, Gorodeski EZ, Taylor DO, Schold JD. Does the unos heart transplant allocation system favor men over women? JACC Heart Fail. 2014; 2:347–355. [PubMed: 25023811]
58.Johnson MR, Meyer KH, Haft J, Kinder D, Webber SA, Dyke DB. Heart transplantation in the united states, 1999-2008. Am J Transplant. 2010; 10:1035–1046. [PubMed: 20420651]
59.Davies RR, Russo MJ, Yang J, Quaegebeur JM, Mosca RS, Chen JM. Listing and transplanting adults with congenital heart disease. Circulation. 2011; 123:759–767. [PubMed: 21300954]
60.Lamas D, Rosenbaum L. Very complicated math--reconfiguring organ allocation. N Engl J Med. 2014; 371:2447–2450. [PubMed: 25539103]
61.[january 9, 2014] Scientific registry of transplant recipients: Heart waiting list by gender
2000-2009. Available at: Http://srtr.Transplant.Hrsa.Gov/annual_reports/2010/1103_cangender_hr.Htm
62.Weidner G, Zahn D, Mendell NR, Smits JM, Deng MC, Zittermann A, Spaderna H. Patients' sex and emotional support as predictors of death and clinical deterioration in the waiting for a new heart study: Results from the 1-year follow-up. Prog Transplant. 2011; 21:106–114. [PubMed: 21736238]
63.Hsich EM, Starling RC, Blackstone E, Rogers J, Taylor DO, Schold JD. Restrictive cardiomyopathy and risk of mortality on waiting list for heart transplantation. The Journal of Heart and Lung Transplantation. 33:S66–S67.
64.Colvin M, Smith JM, Skeans MA, Edwards LB, Callahan ER, Snyder JJ, Israni AK, Kasiske BL. Heart. Am J Transplant. 2016; 16(Suppl 2):115–140. [PubMed: 26755266]
65.[july 2015] Roadmap study demonstrating benefits of heartmate ii left ventricular assist device presented at international society for heart and lung transplanation. 2015. Available at http:// www.Ishlt.Org/contentdocuments/pressrelease_ishlt2015_roadmap.Pdf
66.Kirklin JK, Naftel DC, Pagani FD, Kormos RL, Stevenson LW, Blume ED, Miller MA, Timothy Baldwin J, Young JB. Sixth intermacs annual report: A 10,000-patient database. J Heart Lung Transplant. 2014; 33:555–564. [PubMed: 24856259]
67.Birks EJ. A changing trend toward destination therapy: Are we treating the same patients differently? Tex Heart Inst J. 2011; 38:552–554. [PubMed: 22163133]
68.Starling RC, Blackstone EH, Smedira NG. Increase in left ventricular assist device thrombosis. N Engl J Med. 2014; 370:1465–1466.
Circ Heart Fail. Author manuscript; available in PMC 2017 June 05.

Manuscript Author
Manuscript Author
Manuscript Author
Manuscript Author
Hsich |
Page 15 |
Figure 1.
Organ Donation Registration and The Impact of Facebook Organ Donor Initiative. On May 1, 2012 Facebook launched to 30% of their customers a Facebook “Timeline” platform that included organ donor designation. At that site one could link to educational information and state registration. Upon registering, potential donor's “network of friends” was notified of the change in status. Figure A. Graphs the Facebook Initiative and the effect on new online registration compared to those who were already an organ donor at time of Facebook usage. Figure B. Compares the effect of online Facebook registration to Department of Motor Vehicle registration. Copied from Cameron et al.28
Circ Heart Fail. Author manuscript; available in PMC 2017 June 05.

Hsich |
Page 16 |
Manuscript Author
Manuscript Author
Figure 2.
Interaction between Donor Left Ventricular Hypertrophy and Ischemic Time on Post-
Transplant Survival. Copied from Wever Pinzon et al32
Manuscript Author
Manuscript Author
Circ Heart Fail. Author manuscript; available in PMC 2017 June 05.

Manuscript Author
Manuscript Author
Manuscript Author
Manuscript Author
Hsich |
Page 17 |
Figure 3.
Cardiac Transplant Research Database: Adults Heart Transplantation and the Effect of Donor Hypertension (A) or Diabetes Mellitus (B) and Gender. The cohort consists of 7,322 patients from 32 heart transplant centers who were transplanted between 1990-2007. Copied from Stehlik et al33
Circ Heart Fail. Author manuscript; available in PMC 2017 June 05.
Hsich |
Page 18 |
Manuscript Author
Manuscript Author
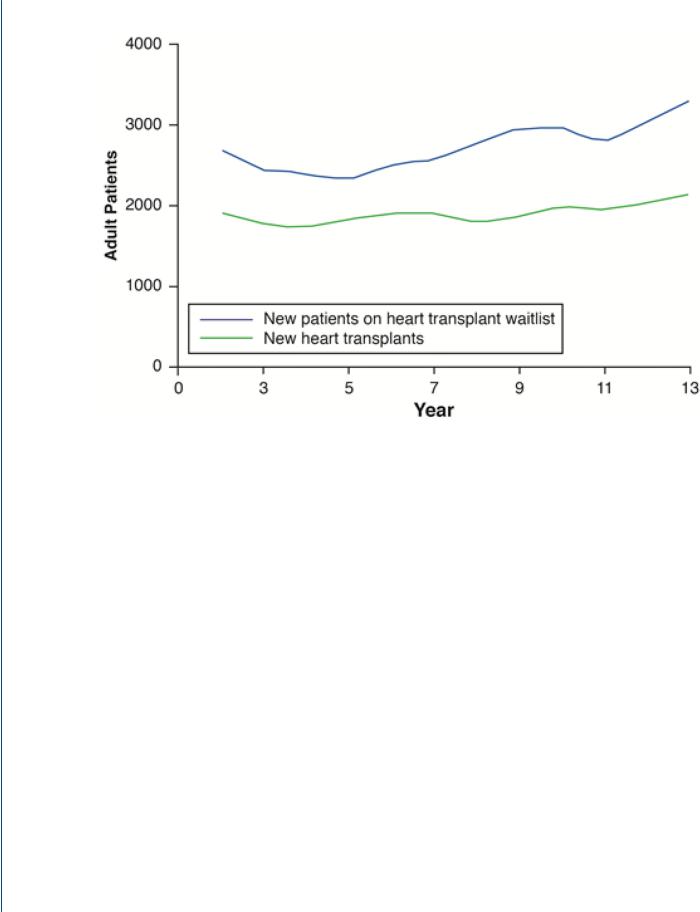
Figure 4.
Scientific Registry of Transplant Recipients: Total Patients Awaiting and Receiving Heart
Transplantation from 2002-2013. Adapted from Colvin-Adams et al39
Manuscript Author
Manuscript Author
Circ Heart Fail. Author manuscript; available in PMC 2017 June 05.
Manuscript Author
Manuscript Author
Manuscript Author
Manuscript Author
Hsich |
Page 19 |
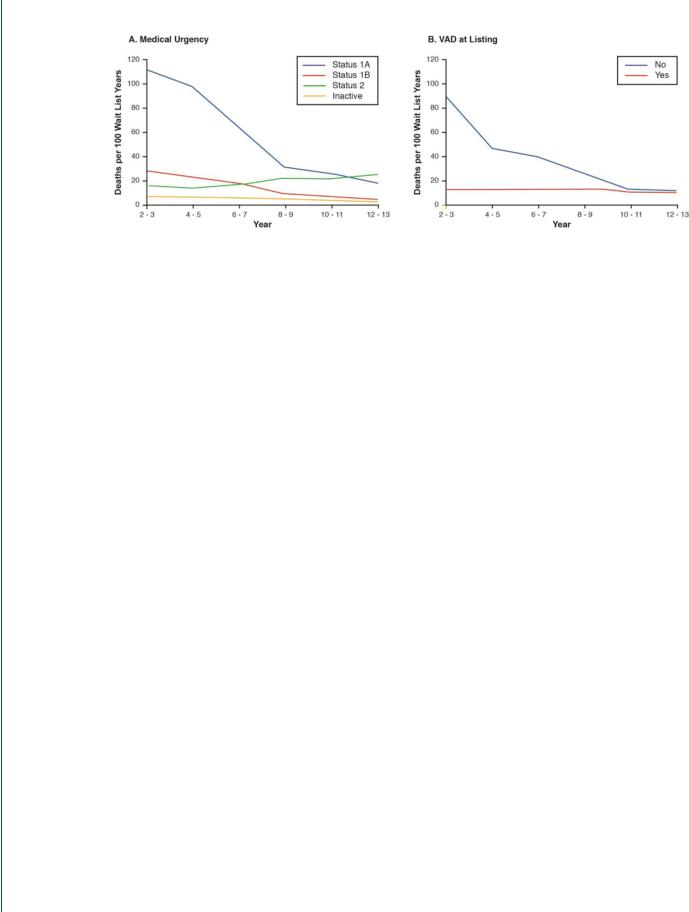
Figure 5.
Scientific Registry of Transplant Recipients: Mortality on Waiting List For Heart Transplantation from 2002-2013. Figure A. Mortality stratified by UNOS Status. Figure B. Mortality stratified by presence of a ventricular assist device. Adapted from Colvin-Adams et al39
Circ Heart Fail. Author manuscript; available in PMC 2017 June 05.
Manuscript Author
Manuscript Author
Manuscript Author
Manuscript Author
Hsich |
Page 20 |
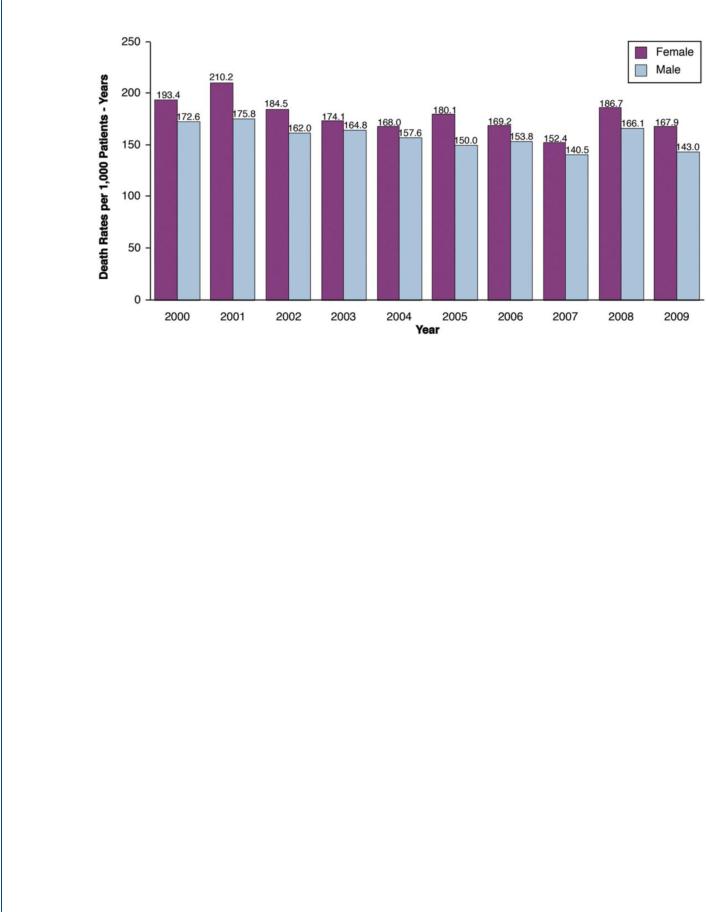
Figure 6.
Scientific Registry of Transplant Recipients: Gender Differences in Survival on Heart Transplant Waiting List from 2000-2009. Adapted from SRTR data61
Circ Heart Fail. Author manuscript; available in PMC 2017 June 05.
Manuscript Author
Manuscript Author
Manuscript Author
Manuscript Author
Hsich |
Page 21 |
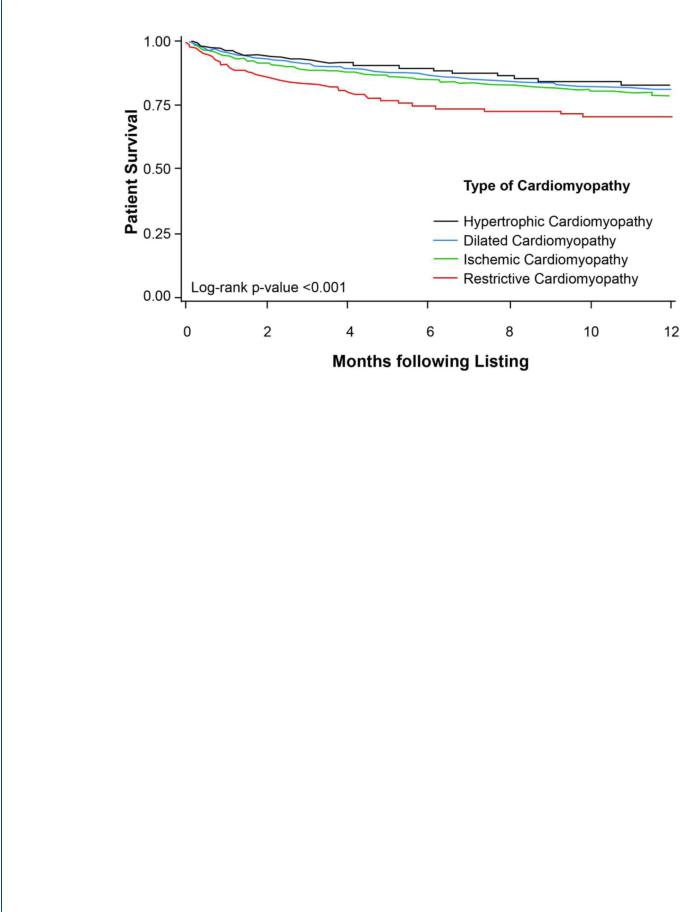
Figure 7.
Scientific Registry of Transplant Recipients Between 2000-2010: Survival on Heart Transplant Waiting list based on Type of Cardiomyopathy. Copied from Hsich et al63
Circ Heart Fail. Author manuscript; available in PMC 2017 June 05.
