
English Lectures / lipids 3 ENG
.pdf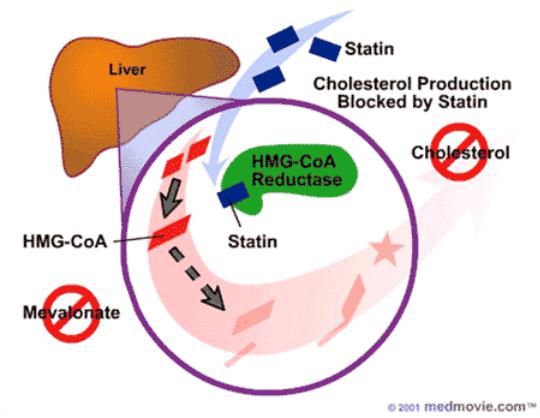
Biochemical basis for the treatment of atherosclerosis and prevention of myocardial infarction
•The most effective drugs used in the treatment of atherosclerosis are HMG-CoA reductase inhibitors. These drugs - antibiotics, for example, mevacor, are transformed into the active form in the liver and effectively inhibit the regulatory enzyme of cholesterol biosynthesis. Such drugs can almost completely suppress the synthesis of their own cholesterol in the body. Under these conditions, the liver increases the uptake of cholesterol from the blood. For this, in liver cells, the synthesis of protein receptors for L-PNP is almost doubled and, accordingly, the uptake of LDL from blood is increased. Thus, the concentration of cholesterol in the blood even in patients with a heterozygous form of familial hypercholesterolemia can be brought almost to normal.

Biochemical basis for the treatment of atherosclerosis and prevention of myocardial infarction
• Medicines - fibrates (clofibrate, fenofibrate) - accelerate the catabolism of VLDL, activating LP-lipase. These drugs also activate the oxidation of fatty acids in the liver, thereby reducing the synthesis of triacylglycerols and cholesterol esters and, as a result, the secretion of VLDL by the liver. Clofibrate induces the synthesis of peroxisome enzymes capable of oxidizing fatty acids. Fibrates are usually used with a combination of hypertriglycerolemia and hypercholesterolemia. For the effective treatment of atherosclerosis, as a rule, the combined effect of several drugs is used.
Biosynthesis and catabolism of sphingolipids
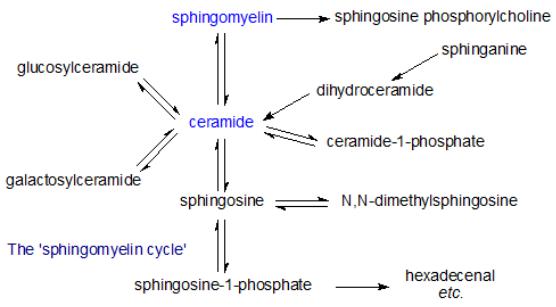
•The biosynthesis of de novo sphingolipids begins with the condensation of serine and the acyl derivative of coenzyme A, resulting in the formation of 3-ketosphinganin. The reaction is catalyzed by pyridoxal-5-phosphate-dependent serine-palmitoyltransferase or 3-keto-sphinganin synthase localized on the cytosolic surface of the endoplasmic reticulum.
•Then 3-ketosphinganin is rapidly reduced to sphinganin under the influence of NADPH-dependent reductase.
•Next, sphinganin is acylated with the formation of N- acylsphinganin (dihydroceramide).
•The reaction is catalyzed by sphinganin-M-acyltransferase or ceramide synthase, which does not favor sphinganin or sphingenin.
•During phosphorylation of ceramide using specific ceramide kinase, ceramide-1-phosphate is formed. Joining at the C-1 position of one or more carbohydrate residues leads to the formation of various glycosphingolipids.
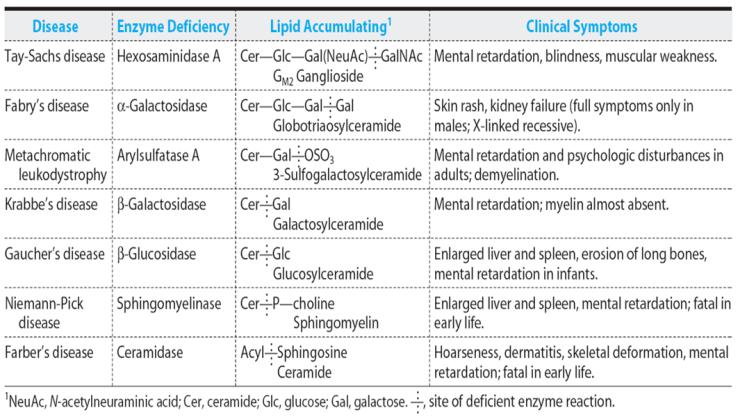
Sphingolipidoses
•Sphingolipidoses - a group of congenital, genetically caused diseases, which are based on a hereditary defect of enzymes that ensure the catabolism of sphingolipids. Diseases are accompanied by the accumulation of sphingolipids in a particular organ that violates the functions of this organ. Sphingolipidoses belong to lysosomal diseases - diseases of accumulation.
Quantitative determination of serum cholesterol
•The principle of the method. The serum cholesterol is treated with the Lieberman-Burchard reagent (a mixture of acetic anhydride,
glacial acetic acid and concentrated H2SO4). In this case, cholesterol loses water and turns into a unsaturated hydrocarbon, which forms a green color with acetic anhydride. The intensity of the color obtained is determined by FEC.
Clinical and diagnostic value of determination of cholesterol in blood serum (plasma)
•Serum cholesterol in a person depends on age. The blood serum of a healthy adult contains 1.5-2.4 g/L (3.63-5.2 mmol/L) of cholesterol, in children - 1.0-1.3 g/L, boys - 1.3 -1.8 g/L, in older people above 2.4 g/L. In men older than 60 years, the serum cholesterol content is slightly lower than in men 50-60 years old. This is due to a decrease in the production and secretion of sex hormones in the blood. Serum cholesterol in women of childbearing age is lower than in men; after 60 years, gender differences in the level of this indicator disappear.
•The blood level of cholesterol reflects the state of lipid metabolism. Cholesterol metabolism is often impaired in various diseases.
Principle and chemistry of quantitative determination of lipoproteins
• The principle of the method. With the interaction of LDL serum with a heparin reagent appears turbidity, the intensity of which is determined photometrically. Heparin reagent is a mixture of heparin with calcium chloride.
•Clinical and diagnostic value. The content of LDL (b-lipoproteins) in the blood varies depending on age, gender and is normally 3.0-4.5 g/L. An increase in LDL concentration is observed with atherosclerosis, obstructive jaundice, acute hepatitis, chronic liver diseases, diabetes, glycogenosis, xanthomatosis and obesity, a decrease - with b-plasmacytoma. The average LDL cholesterol is about 47%.
