- •Abstract
- •Chapter 1 – Introduction
- •Chapter 2 - Methods
- •Chapter 3 - What is stroke
- •Figure 1 Post stroke disabilities (Genentech., 2014)
- •Ischaemic stroke happens when a blockage in the artery supplying the brain occurs, leading to hypoxia. Causes of ischaemic stroke include:
- •Figure 4 Molecular process of neuronal ischaemia. (Colledge, Walker and Ralston., 2010, p. 1182)
- •Available treatments for stroke
- •Figure 5 The mechanism of aspirin inhibiting ptgs enzyme (Novara., 2013)
- •Figure 6 Mechanism of t-pa action, (Genentech, 2014)
- •Embryonic stem cells
- •Figure 8 Formation of neurons from a blastocyst (Lindvall et al., 2004)
- •Adult stem cells
- •Figure 10 Reprogramming adult stem cells into induced pluripotent stem cells usig Oct4, Klf4, Sox2 and c-Myc genes (Meregalli et al., 2011).
- •Mesenchymal stem cells
- •MsCs for treatment of stroke
- •Chapter 5 - Migratory mechanisms of msCs
- •Chapter 6 - Discussion
Figure 1 Post stroke disabilities (Genentech., 2014)
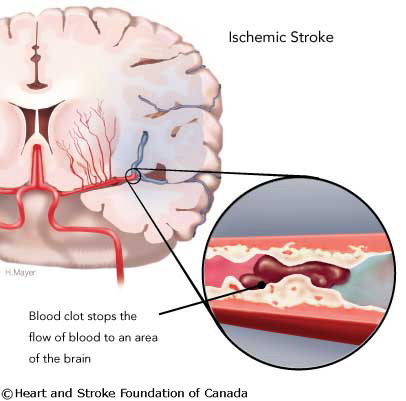
Two major types of stroke are: ∙ Ischaemic sroke (Figure 2)
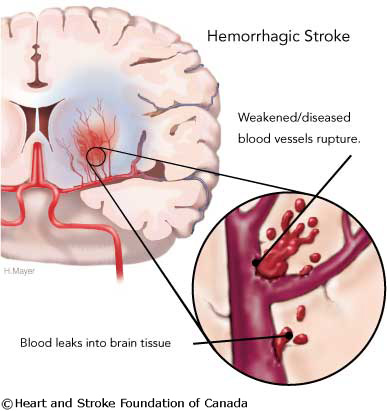
∙ Haemorrhagic stroke (Figure 3)
The majority of strokes are ischemic (87%), others are haemorrhagic (Heart and stroke foundation of Canada, 2008).
|
|
Figure 2 Ischaemic Stroke (Heart and stroke foundation of Canada, 2008)
|
Figure 3 Haemorrhagic Stroke (Heart and stroke foundation of Canada, 2008)
|
Ischaemic stroke happens when a blockage in the artery supplying the brain occurs, leading to hypoxia. Causes of ischaemic stroke include:
Thrombosis - thrombus (blood clot) forms locally, obstructing blood vessels within the brain, either veins or arteries.
Systemic hypoperfusion – such as in shock , for example hypovolemic, which results from inadequate blood volume for the continuation of satisfactory cardiac output, blood pressure, and tissue perfusion.
Cerebral embolism – embolus (blood clot) forms in any blood vessel within the body and travels to the brain.
Cryptogenic stroke – obscure or of unknown origin, without any obvious explanations, occurs in 30-40% of ischaemic strokes.
H
Cerebral venous sinus thrombosis
Arteriovenous malformation
Bleeding within a tumour
Amyloid angiopathy
aemorrhagic strokes are intracerebral bleeds and can be caused by:
Penetrating head trauma
Depressed skull fractures
Rupture of an aneurysm
Acceleration-deceleration trauma
The risk factors for stroke can either be fixed or amendable and include: (Colledge et al., 2010)
A
High blood pressure
Heart disease (atrial fibrillation, heart failure)
Diabetes mellitus
Hyperlipidaemia
Smoking
Excess alcohol consumption (≥2/day)
Polycythaemia
Oral contraceptives
Social deprivation
Gender (male > female, except in the very young and very old)
Race (Afro-Carribean > Asian > European)
Heredity
High fibrinogen
Previous vascular event, e.g. MI, stroke or peripheral embolism
Menopause
A study by Nakano et al., (2011) demonstrates that susceptibility for haemorrhagic stroke can also be increased after infection with serotype k Streptococcus mutants that express collagen-binding protein (CBP). This is because the bacteria are able to bind to collagen fibres in the damaged blood vessels, as CBP prevents collagen-dependent platelet aggregation, therefore the blood vessel remains open and bleeding continues.
Molecular mechanisms of neuronal ischaemia and infarction are depicted in Figure 4 and occur in the following order:
Reduced blood flow decreases oxygen and glucose supply and therefore also decreasing ATP levels.
Without ATP, energy-dependent transmembrane ion transporters fail, leading to membrane depolarisation and cytotoxic oedema, which allows glutamate to be released and calcium to enter.
Glutamate-gated channels transport calcium into cells.
Calcium then activates lipid peroxidises, poteases and other destructive enzymes, which in turn destroy intracellular organelles and the phospholipid cell membrane by releasing of free radicals.
The release of free fatty acid activates coagulation, which intensifies local ischaemia.
Glial cells take up H+ions instead of extracellular glutamate. This lack of glutamate leads to apoptosis of glial cells. The release of inflammatory mediators by microglia and astrocytes lead to necrosis of all cell types in the whole arterial territory.