
Lecture 2.5: Hypersensitivity (Allergy)
Plan:
Type I (Anaphylactic) Reactions
Type II (Cytotoxic) Reactions
Type III (Immune Complex) Reactions
Type IV (Delayed Cell-Mediated) Reactions
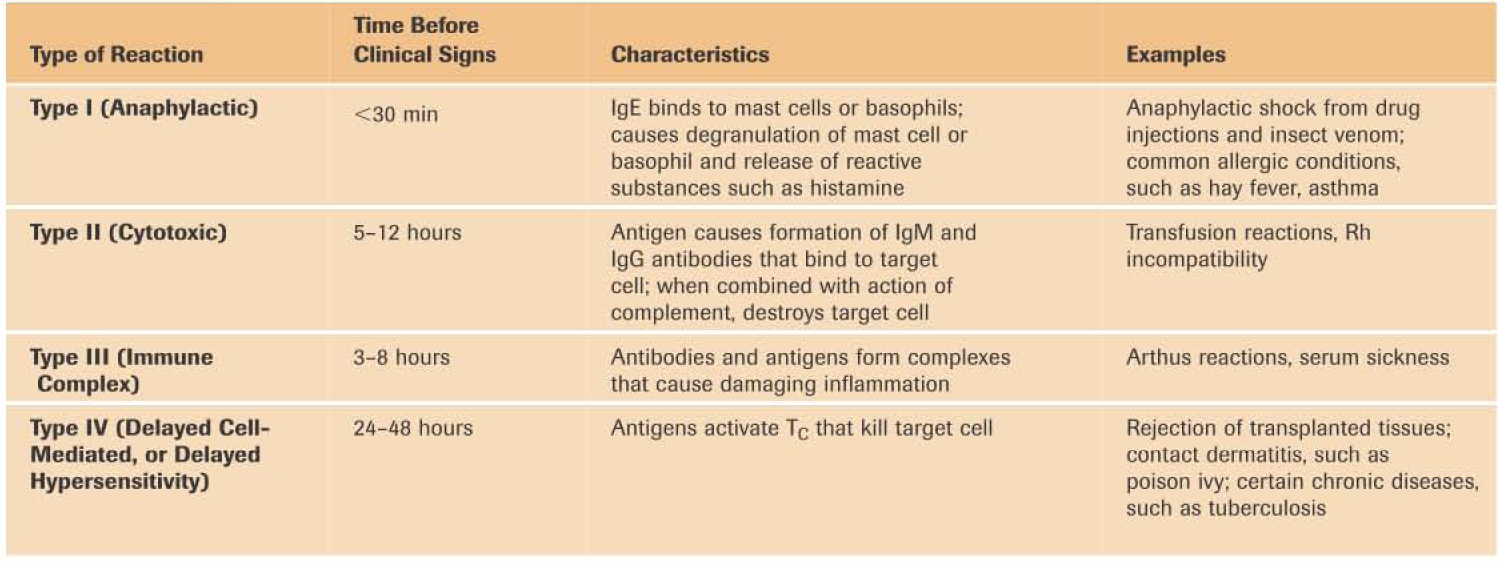
The term hypersensitivity refers to an antigenic response beyond that which is considered normal; the term allergy is more familiar and is essentially synonymous. Hypersensitivity responses occur in individuals who have been sensitized by previous exposure to an antigen, which in this context is sometimes called an allergen. When an individual who was previously sensitized is exposed to that antigen again, his or her immune system reacts to it in a damaging manner. There are four principal types of hypersensitivity reactions: anaphylactic, cytotoxic, immune complex, and cell-mediated (or delayed-type) reactions (Table1).
Table 1
Types of Hypersensitivity
Type I (Anaphylactic) Reactions
Type I, or anaphylactic, react ions often occur within 2 to 30 minutes after a person sensitized to an antigen is reexposed to that antigen. Anaphylaxis means opposite of protected," from the prefix ana-, meaning against, and the Greek phylaxis, meaning protection. Anaphylaxis is an inclusive term for the reactions caused when certain antigens combine with IgE antibodies. Anaphylactic responses can be systemic reactions, which produce shock and breathing difficulties and are sometimes fatal, or localized reactions, which include common allergic conditions such as hay fever, asthma, and hives (slightly raised, often itchy and reddened areas of the skin).
The IgE antibodies produced in response to an antigen, such as insect venom or plant pollen, bind to the surfaces of cells such as mast cells and basophils. These two cell types are similar in morphology and in their contribution to allergic reactions. Mast cells are especially prevalent in the connective tissue of the skin and respiratory tract and in surrounding blood vessels. The name is from the German word mastzellen, meaning “well fed”; they are packed with granules (Figure 1a). Basophils circulate in the bloodstream, where they constitute fewer than 1 % of the leukocytes. Both are filled with granules containing a variety of chemicals called mediators.

Figure 1a The mechanism of anaphylaxis. IgE antibodies, produced in response to an antigen, coat mast cells and basophils. When an antigen bridges the gap between two adjacent antibody molecules of the same specificity, the cell undergoes degranulation and releases histamine and other mediators.
Mast cells and basophils can have as many as 500,000 sites for IgE attachment. The Fc (stem) region of an IgE antibody can attach to one of these specific receptor sites on such a cell, leaving two antigen-binding sites free. Of course, the attached IgE monomers will not all be specific for the same antigen. But when an antigen such as plant pollen encounters two adjacent antibodies of the same appropriate specificity, it can bind to one antigen-binding site on each antibody, bridging the space between them. This bridge triggers the mast cell or basophil to undergo degranulation, which releases the granules inside these cells and also the mediators they contain (Figure 1 b).
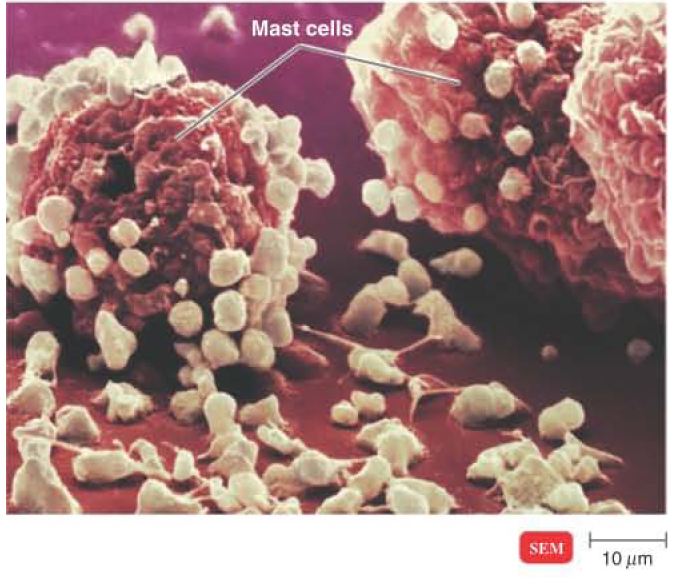
Figure 1b The mechanism of anaphylaxis. A degranulated mast cell that has reacted with an antigen and released granules of histamine and other reactive mediators.
These mediators cause the unpleasant and damaging effects of an allergic reaction. The best-known mediator is histamine. The release of histamine increases the permeability and distension of blood capillaries, resulting in edema (swelling) and erythema (redness). Other effects include increased mucus secretion (a runny nose, for example) and smooth muscle contraction, which in the respiratory bronchi results in breathing difficulty.
Other mediators include leukotrienes of various types and prostaglandins. These mediators are not preformed and stored in the granules but are synthesized by the antigen-triggered cell. Because leukotrienes tend to cause prolonged contractions of certain smooth muscles, their action contributes to the spasms of the bronchial tubes that occur during asthmatic attacks. Prostaglandins affect smooth muscles of the respiratory system and increase mucus secretion.
Collectively, all these mediators serve as chemotactic agents that, in a few hours, attract neutrophils and eosinophils to the site of the degranulated cell. They then activate various factors that cause inflammatory symptoms, such as distension of the capillaries, swelling, increased secretion of mucus, and involuntary contractions of smooth muscles.
Systemic Anaphylaxis
At the turn of the twentieth century, two French biologists studied the responses of dogs to the venom of stinging jellyfish. Large doses of venom usually killed the dogs, but sometimes a few survived the injections. These surviving dogs were used for repeat experiments with the venom, and the results were surprising. Even a very tiny dose of the venom, one that should have been almost harmless, killed the dogs. They suffered difficulty in respiration, entered shock as their cardiovascular systems collapsed, and quickly died. This phenomenon was called anaphylactic shock.
Systemic anaphylaxis (or anaphylactic shock) can result when an individual sensitized to an antigen is exposed to it again. Injected antigens are more likely to cause a dramatic response than antigens introduced via other portals of entry. The release of mediators causes peripheral blood vessels throughout the body to enlarge, resulting in a drop in blood pressure (shock). This reaction can be fatal within a few minutes. There is very little time to act once someone develops systemic anaphylaxis. Treatment usually involves self-administration with a preloaded syringe of epinephrine, a drug that constricts blood vessels and raises the blood pressure.
Localized Anaphylaxis
Whereas sensitization to injected antigens is a common cause of systemic anaphylaxis, localized anaphylaxis is usually associated with antigens that are ingested (foods) or inhaled (pollen). The symptoms depend primarily on the route by which the antigen enters the body.
In allergies involving the upper respiratory system, such as hay fever, sensitization usually involves mast cells in the mucous membranes of the upper respiratory tract. The airborne antigen might be a common environmental material such as plant pollen, fungal spores, feces of house dust mites, or animal dander. The typical symptoms are itchy and teary eyes, congested nasal passages, coughing, and sneezing. Antihistamine drugs, which compete for histamine receptor sites, are often used to treat these symptoms.
Antigens that enter the body via the gastrointestinal tract can also sensitize an individual. So-called food allergies may not be related to hypersensitivity at all and are more accurately described as food intolerances. For example, many people are unable to digest the lactose in milk because they lack the enzyme that breaks down this disaccharide milk sugar. The lactose enters the intestine, where it osmotically retains fluid, causing diarrhea.
Gastrointestinal upset is a common symptom of food allergies, but it can also result from many other factors. Hives are more characteristic of a true food allergy, and ingestion of the antigen may result in systemic anaphylaxis. Death has even resulted when a person sensitive to fish ate french fries that had been prepared in oil previously used to fry fish. Only eight foods are responsible for 97% of food-related allergies: eggs, peanuts, tree-grown nuts, milk, soy, fish, wheat, and peas.
