
1-s2.0-S1547527117312407-main
.pdf
ACCEPTED MANUSCRIPT
229 |
higher heart rate during Control significantly reduced the increase in %eCRT with the algorithm |
|||
230 |
(p<0.05). Finally, having paroxysmal AF (as opposed to persistent or permanent AF) significantly |
|||
231 |
increased the likelihood of a greater increase in %eCRT with the algorithm (p<0.01). None of the |
|||
232 |
other factors considered had a significant effect. |
|
|
|
233 |
Acute testing data were available from 42 subjects comparing no algorithm to CAFR and from 39 |
|||
234 |
subjects comparing no algorithm to eCRTAF. CAFR increased %eCRT pacing from 66±35% (no |
|||
|
|
|
|
T |
235 |
algorithm) to 79±20% (p<0.001). eCRTAF increased %eCRT pacing from 67±37% (no algorithm) to |
|||
236 |
87±17% eCRT pacing (p<0.001). Although these tests were brief, the acute results for CAFR (79±21%) |
|||
237 |
and eCRTAF (87±16%) are consistent with the primary results of the study (81±14% for CAFR/Control |
|||
238 |
and 88±8% for eCRTAF). |
|
CRIP |
|
|
|
|
||
239 |
Safety |
|
|
|
240 |
The algorithm performed as expected and did not result in any unexpected device issues. There |
|||
241 |
were 7 cardiovascular (CV) related adverse events (AEs) during eCRTAF and 3 during CAFR (p=0.37). |
|||
242 |
AEs included shortness of breath (N=4), hypotension (N=2), ICD shock for rapidly conducted AF |
|||
|
|
MANUS |
|
|
243 |
(N=1), fatigue (N=1), and ventricular arrhythmia (N=2). None of the AEs that occurred during the |
|||
244 |
study were adjudicated to be related to either the algorithm or any increase in pacing rate. |
|||
246 |
Discussion |
|
|
|
247 |
On average, the eCRTAF algorithm resulted in a 7% absolute increase in eCRT pacing and %Vp during |
|||
248 |
AF while increasing the mean heart rate by 2.5 bpm. The algorithm had an even greater effect in |
|||
249 |
subjects with lower %Vp during AF while in the Control arm. |
|
|
|
250 |
There are two algorithms currently available in CRT devices to increase pacing during AF but both |
|||
|
ACCEPTED |
|
|
|
251 |
were designed for and tested in a bradycardia pacemaker population. Ventricular Rate |
|
||
252 |
Regularization (VRR, Boston Scientific, Inc.), has not been evaluated in a CRT patient population; |
|||
253 |
however in a pacemaker population with AF, the algorithm was shown to increase %Vp from 38% to |
|||
254 |
58%.7 The rate regularization algorithm in Medtronic devices (CAFR) was used as the control in this |
|||
|
Page 10 of 21 |
|
|
|

ACCEPTED MANUSCRIPT
255study. On average, CAFR achieved 80.8±14.3% eCRT pacing and 83.2±11.9% Vp during AF. There are
256very limited data for delivery of CRT during AF in CRT patients without such an algorithm. Based on
257the limited acute data from this study, the eCRTAF algorithm may produce large increases in %Vp
258and %eCRT when compared to patients without a rate regularization algorithm.
259Although there are data on the optimal %Vp for CRT during AF, there are no similar dataTfor %eCRT
260during AF. Because each beat classified as effective CRT is a V pace beat byCRIPdefinition, loss of %eCRT
261will be at least as clinically important as the loss of %Vp. However, establishing a %eCRT threshold
262for optimal CRT will require additional clinical data.
263It has been demonstrated in several retrospective analyses that small decreases in %Vp (1-3%) are
264associated with a significant increase in mortality.1MANUS-3 Koplan et al. showed that a decrease of as little
265as 1-4 % in V pacing was associated with a significant negative impact on survival free from HF
266hospitalization and all-cause mortality.2 In addition, a history of AF was a significant independent
267predictor of mortality in CRT patients. Hayes et al. also showed in a retrospective study of over
26836,000 CRT patients that a reduction from 1-5% in Vpacing was associated with increased mortality.
269Their analysis alsoACCEPTEDshowed AF had an additive negative effect on mortality.1 The magnitude of the
270increase in %Vp in the current study (7%) suggests that this algorithm could have a significant clinical
271benefit in CRT patients with high AF burden.
272The multi-variate analysis suggests that the biggest impact of the algorithm may be in patients with
273paroxysmal AF although the small number of subjects (N=5) makes it difficult to extrapolate these
274results. This is, however, a plausible correlation as a retrospective analysis of over 12,000 CRT
275subjects with AF demonstrated that those with paroxysmal AF saw the greatest drop in %Vp during
276AF compared to persistent or permanent AF.8 Since low %Vp during AF was also a strong predictor of
277response in the multivariate analysis, its correlation with paroxysmal AF provides an explanation for
278why this group may see the largest effect.
279Our data show that with the eCRTAF algorithm, 5 subjects improved from <90% to >90% eCRT and
280an additional 5 subjects improved from <95% to >95% eCRT. Moreover, in the cohort receiving <80
Page 11 of 21

ACCEPTED MANUSCRIPT
281%Vp during Control, the algorithm improved %eCRT by a mean of 16%. The ability to deliver more
282eCRT during AF may lead to better resynchronization and consequently reduce heart failure
283symptoms. AV junctional ablation (AVJA) is associated with improved outcomes in observational
284trials of patients with permanent AF who did not experience clinical improvement and/or an
285adequate biventricular pacing percentage with rate limiting drugs,9-13 but there are no randomizedT
286controlled trials of AVJA for this indication. The eCRTAF algorithm has theCRIPpotential to increase
287biventricular capture during AF without AVJA . This could improve outcomes in patients not
288previously known to have AF and avoid the need for AVJA in others by achieving high rates of
289biventricular capture. It may also help to identify others for whom AVJA is the only appropriate way
290to achieve sufficient biventricular capture. MANUS
291When considering the applicability of this algorithm to the general CRT patient population, it is
292important to keep in mind that, while most CRT patients do not have AF at initial implant, many will
293develop AF over the course of their disease. A recent retrospective analysis by Hayes et al. suggests
294that as many as 30% of CRT patients will experience clinically significant AF (≥1 day of AT/AF for > 6
295hours) within 2ACCEPTEDyears of implant.14
296Because the eCRTAF algorithm involves additional processing, the impact on device longevity may be
297a concern. According to the manufacturer, a patient with permanent AF (worse-case scenario) will
298experience a 2-3% decrease in device longevity. A 2.5 BPM increase in pacing rate will have an
299additional 1-2% impact on device longevity.
300Limitations
301The majority of the subjects included in this study had permanent or persistent AF. Given the small
302number of paroxysmal AF subjects in the study, additional clinical data is needed to confirm the
303preliminary findings about the algorithm behavior in this group. In addition, the comparison of the
304new algorithm to a control of no rate regularization algorithm at all was only done with a small acute
305dataset. The difference in a chronic ambulatory setting remains to be determined.
Page 12 of 21

306
307
308
309
310
311
312
313
314
315
316
317
318
319
320
ACCEPTED MANUSCRIPT
It is possible that greater variation in RR intervals during AF or an increased number of premature ventricular contractions was associated with lower %VP but this information was not collected in this study. It is also possible that the algorithm would be more effective during regular tachycardias such as atrial flutter, but this study was unable to evaluate this possibility.
|
|
|
T |
Finally, this study did not evaluate long-term clinical events and, therefore, additional investigation is |
|||
|
|
CRIP |
|
needed to demonstrate whether or not a higher %eCRT pacing would result in improved clinical |
|||
outcomes. |
|
|
|
Conclusion |
MANUS |
|
|
|
|
|
|
In a cohort of CRT subjects with high AF burden, eCRTAF was shown to significantly increase the % eCRT pacing during AF from 80.8% to 87.8% (p<0.001) and %Vp during AF from 83.2% to 90.0%
(p<0.001) while increasing the mean HR by an average of 2.5 bpm (p<0.001). Given the significant proportion of CRT patients that will develop AF over their disease course, this algorithm could represent a non-invasive, low risk strategy to increase CRT delivery during AF, potentially improving
CRT response and preventing adverse outcomes.
ACCEPTED
Page 13 of 21

ACCEPTED MANUSCRIPT
321References
3221. Hayes DL, Boehmer JP, Day JD, Gilliam Iii FR, Heidenreich PA, Seth M, Jones PW, Saxon LA.
323Cardiac resynchronization therapy and the relationship of percent biventricular pacing to
324symptoms and survival. Heart Rhythm 2011;8:1469-1475.
3252. Koplan BA, Kaplan AJ, Weiner S, Jones PW, Seth M, Christman SA. Heart Failure
326Decompensation and All-Cause Mortality in Relation to Percent Biventricular Pacing in
327Patients With Heart Failure: Is a Goal of 100% Biventricular Pacing Necessary? JournalT of the
328American College of Cardiology 2009;53:355-360.
3293. Ruwald A-C, Kutyifa V, Ruwald MH, et al. The association between biventricular pacing and
330cardiac resynchronization therapy-defibrillator efficacy when comparedCRIPwith implantable
331cardioverter defibrillator on outcomes and reverse remodelling. European Heart Journal
3322015;36:440-448.
3334. Tse H-F, Newman D, Ellenbogen KA, Buhr T, Markowitz T, Lau C-P. Effects of ventricular rate
334regularization pacing on quality of life and symptoms in patients with atrial fibrillation (Atrial
335fibrillation symptoms mediated by pacing to mean rates [AF SYMPTOMS Study]). The
336American Journal of Cardiology 2004;94:938MANUS-941.
3375. Ghosh S, Stadler RW, Mittal S. Automated detection of effective left-ventricular pacing:
338going beyond percentage pacing counters. Europace: European Pacing, Arrhythmias, And
339Cardiac Electrophysiology: Journal Of The Working Groups On Cardiac Pacing, Arrhythmias,
340And Cardiac Cellular Electrophysiology Of The European Society Of Cardiology 2015.
3416. Hernández-Madrid A, Facchin D, Klepfer RN, Ghosh S, Matía R, Moreno J, Locatelli A. Device
342pacing diagnostics overestimate effective CRT pacing results of the holter for efficacy
343analysis of CRT study (OLE CRT study). Heart Rhythm In Press.
3447. Ciaramitaro G, Sgarito G, Solimene F, Maglia G, Vicentini A, Di Donato G, Raciti G, Parrinello
345G, Del Giudice GB. Role of Rate Control and Regularization Through Pacing in Patients With
346Chronic Atrial Fibrillation and Preserved Ventricular Function: The VRR Study. Pacing &
347ClinicalACCEPTEDElectrophysiology 2006;29:866-874.
3488. Ousdigian KT, Borek PP, Koehler JL, Heywood JT, Ziegler PD, Wilkoff BL. The Epidemic of
349Inadequate Biventricular Pacing in Patients With Persistent or Permanent Atrial Fibrillation
350and Its Association With Mortality. Circulation: Arrhythmia and Electrophysiology
3512014;7:370-376.
3529. Dong K, Shen W-K, Powell BD, Dong Y-X, Rea RF, Friedman PA, Hodge DO, Wiste HJ, Webster
353T, Hayes DL, Cha Y-M. Atrioventricular nodal ablation predicts survival benefit in patients
354with atrial fibrillation receiving cardiac resynchronization therapy. Heart Rhythm
3552010;7:1240-1245.
35610. Ganesan AN, Brooks AG, Roberts-Thomson KC, Lau DH, Kalman JM, Sanders P. Role of AV
357Nodal Ablation in Cardiac Resynchronization in Patients With Coexistent Atrial Fibrillation
358and Heart Failure: A Systematic Review. Journal of the American College of Cardiology
3592012;59:719-726.
36011. Gasparini M, Auricchio A, Metra M, Regoli F, Fantoni C, Lamp B, Curnis A, Vogt J, Klersy C.
361Long-term survival in patients undergoing cardiac resynchronization therapy: the
362importance of performing atrio-ventricular junction ablation in patients with permanent
363atrial fibrillation. European Heart Journal 2008;29:1644-1652.
36412. Gasparini M, Leclercq C, Lunati M, Landolina M, Auricchio A, Santini M, Boriani G, Lamp B,
365Proclemer A, Curnis A, Klersy C, Leyva F. Cardiac Resynchronization Therapy in Patients With
366Atrial Fibrillation. JACC: Heart Failure 2013;1:500-507.
36713. Gasparini M, Steinberg JS, Arshad A, Regoli F, Galimberti P, Rosier A, Daubert JC, Klersy C,
368Kamath G, Leclercq C. Resumption of sinus rhythm in patients with heart failure and
369permanent atrial fibrillation undergoing cardiac resynchronization therapy: a longitudinal
370observational study. European Heart Journal 2010;31:976-983.
Page 14 of 21

ACCEPTED MANUSCRIPT
37114. Hayes DL, Monteiro JV, Klepfer R, Grenz NA, Tsintzos SI, Eggington S, Shah BR. Abstract
37212995: Prevalence and Incidence of Atrial Fibrillation in a Population Implanted With Cardiac
373Resynchronization Therapy Devices Implanted for at Least 30 Days: Evidence From a
374Prospective Clinical Trial. Circulation 2016;134:A12995-A12995.
375
376
|
|
CRIP |
T |
|
MANUS |
|
|
ACCEPTED |
|
|
|
|
|
|
Page 15 of 21

ACCEPTED MANUSCRIPT
377 Table 1. Subject demographics at the time of enrollment.
378
379 |
|
|
Total Analyzed |
|
|
|
|
|
|
|
Subject Characteristics |
|
(N = 54) |
|
|
|
|
|
|
|
Gender (N,%) (Male) |
|
50 |
(92.6%) |
|
|
|||
|
Age (years) |
|
71.0 ± 10.5 |
|
|
|
|||
|
LVEF (%) |
|
28.8 ± 8.1 |
|
|
|
|||
|
Intrinsic QRS Duration (msec) |
|
157.3 ± 36.4 |
|
|
|
|||
|
Heart Rate (bpm) |
|
76.1 ± 10.6 |
|
|
|
|||
|
NYHA Classification (N,%) |
|
MANUS |
|
|
|
|||
|
|
|
||
|
|
|
||
|
Class I |
|
6 (11.1%) |
|
|
Class II |
|
22 |
(40.7%) |
|
Class III |
|
16 |
(29.6%) |
|
Not available |
|
10 |
(18.5%) |
|
|
|
|
|
|
LBBB (N,%) |
|
26 |
(48.1%) |
|
Coronary Artery Disease (N,%) |
|
28 |
(51.9%) |
|
|
|||
|
Ischemic Cardiomyopathy (N,%) |
|
21 |
(38.9%) |
|
|
|||
|
ACCEPTED |
|
|
|
|
|
|
|
|
|
AV Conduction Status |
|
54 (100%) |
|
|
1st degree block |
|
3 |
(5.6%) |
|
2nd degree block |
|
0 (0%) |
|
|
3rd degree block |
|
0 (0%) |
|
|
|
|
|
|
|
Atrial Fibrillation (N,%) |
|
54 (100%) |
|
|
|
|
|
|
|
Permanent |
|
28 |
(51.9%) |
|
Persistent |
|
21 |
(38.9%) |
|
Paroxysmal |
|
5 |
(9.3%) |
|
|
|
|
|
|
Rate/Rhythm Control Drugs (N,%) |
|
54 (100%) |
|
|
|
|
|
|
|
Antiarrhythmics - Class III |
|
7 (13.0%) |
|
|
Beta-Blockers |
|
51 |
(94.4%) |
|
Calcium Channel Blockers |
|
4 |
(7.4%) |
|
Cardiac Glycosides |
|
27 |
(50.0%) |
|
|
|
|
|
|
|
|
|
|
CRIP |
T |
|
Page 16 of 21

ACCEPTED MANUSCRIPT
380
381 Figure 1. Flow diagram for study design.
382
383
384
|
|
CRIP |
T |
|
MANUS |
|
|
ACCEPTED |
|
|
|
|
|
|
Page 17 of 21
ACCEPTED MANUSCRIPT
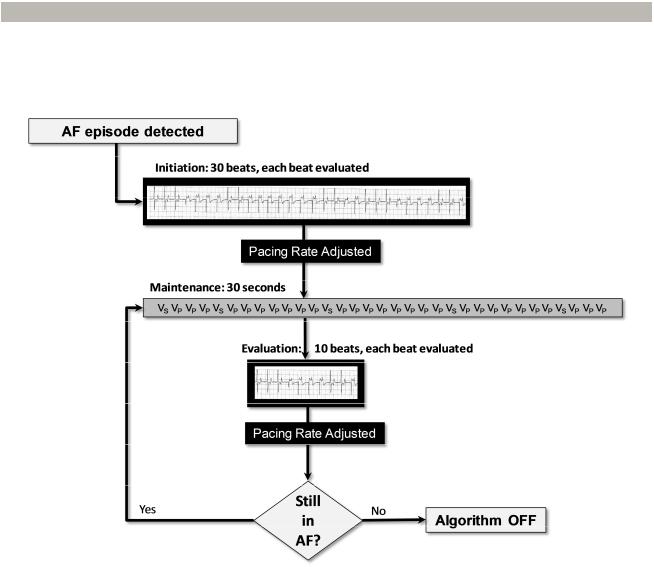
385 Figure 2. Flow diagram for the EffectivCRT during AF algorithm.
386
387
388
|
MANUS |
CRIP |
ACCEPTED |
|
|
|
|
Page 18 of 21

ACCEPTED MANUSCRIPT
389 Figure 3. Cohort distribution of study participants.
390
391
|
MANUS |
CRIP |
ACCEPTED |
|
|
|
|
Page 19 of 21
