
Учебники / Operative Techniques in Laryngology Rosen 2008
.pdf
56 |
Airway Management for Larygeal Surgery |
Fig. 9.6 Illustration of anatomic features in a patient with “difficult airway exposure”
9
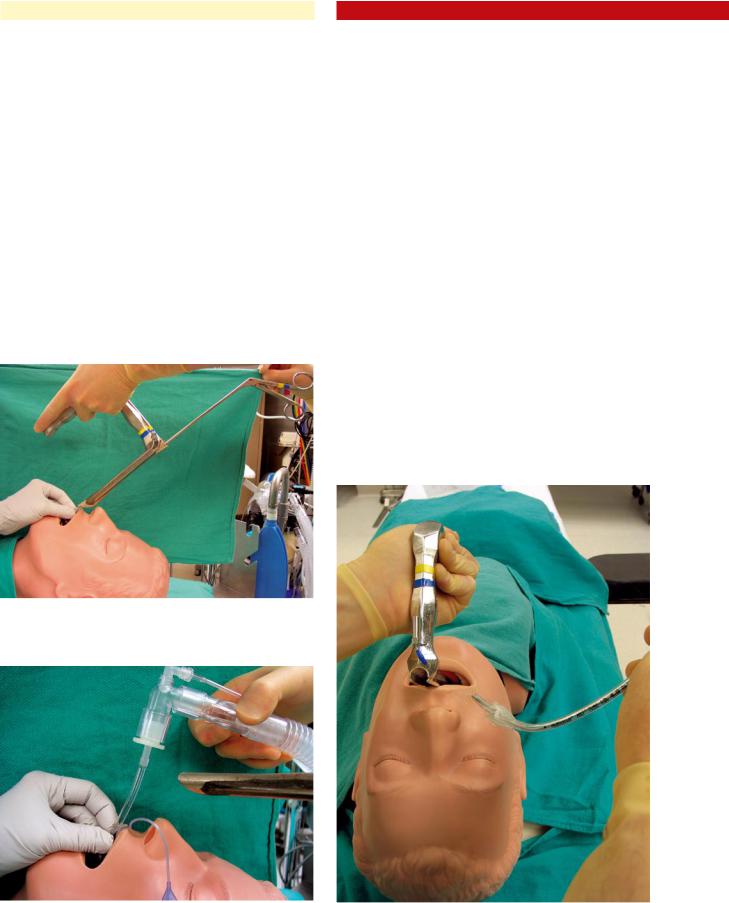
Fig. 9.7 Intubation through an Ossoff–Pilling laryngoscope. A 5.0 ETT or smaller should be used
alternative means of securing the airway must be employed. The following conditions may predict a “difficult exposure” perorally (Fig. 9.6):
a)Retrognathia
b)Lingual hypertrophy/Poor palatal visualization
c)Trismus/reduced interincisor opening
d)Short, thick neck
e)Limited neck extension
2.Alternative methods of obtaining an airway in a “difficult exposure” case:
a)Tracheostomy under local
b)Awake, flexible laryngoscopy with nasotracheal intubation
c)Laryngoscopy and intubation using specialized “anterior” laryngoscope
i.Ossoff–Pilling laryngoscope
d)Laryngoscopy and intubation without visualization of vocal folds
i.Sliding Jackson laryngoscope plus curved ETT with stylet
e)Laryngeal mask anesthesia (LMA)
3.Specialized techniques:
a)Intubation using Ossoff-Pilling laryngoscope
In patients in whom difficulty with rigid transoral airway exposure is anticipated/encountered, the Ossoff–Pilling (OP) laryngoscope is extremely valuable. In close to 99% of surgical patients, the OP laryngoscope allows successful transoral exposure of the glottis.
i.The patient is pre-oxygenated, and mask induction is utilized. Paralytics are avoided, and spontaneous ventilation (or assisted mask ventilation) is maintained. When the patient achieves the desired level of anesthesia, the surgical table is turned 90°, facing the surgeon.
ii.The OP laryngoscope is passed perorally and advanced to the level of the vocal folds (or ideally, slightly distal, into the infraglottis). A suspension device (Lewy) can also be used to achieve additional
Fig. 9.8 Removal of connector from ETT to facilitate passage of the |
Fig. 9.9 Laryngeal cup forceps are used to grasp the ETT |
tube through the laryngoscope |
|
anterior rotation of the laryngoscope in particularly difficult cases, but is not often necessary.
iii.A 5.0 MLT (or smaller) is placed directly through the laryngoscope to secure the airway. The balloon can be inflated, position confirmed, and ventilation/ oxygenation established until the patient is stabilized (Fig. 9.7).
iv.The laryngoscope can then be removed over the tube (with a pseudo-Seldinger technique), leaving the ETT in place:
i.The plastic connector is removed from the proximal end of the ETT (Fig. 9.8).
ii.A medium–large laryngeal cup forceps is used to grasp the proximal ETT (Fig. 9.9).
iii.The surgeon backs the OP scope out of the oral cavity while holding the ETT stationary to prevent extubation.
iv.When the intraoral portion of the tube can be visualized, it is secured by an assistant (Fig. 9.10).
Chapter 9 |
57 |
v. The cup forceps is released, and the OP scope is pulled back until the entire ETT and trailing cuffinflation tubing are passed through its lumen (Fig. 9.11). Larger cuff-inflation ports (especially the liq- uid-filled variety used in laser-protected ETTs), may get caught within the narrow distal lumen of the OP scope. The cup forceps can be used to push this device through the scope, however.
b)Sliding Jackson laryngoscope
In patients in whom it is impossible to visualize the vocal folds with the above (OP laryngoscopic) technique, a Sliding Jackson (SJ) laryngoscope can be used for peroral intubation in select cases. While the SJ scope does not provide superior visualization of the glottis in difficult, “anterior” patients, it can be used as a “familiar” intubation laryngoscope (analogous to the Miller blade used by anesthesiologists). In cases where the glottis cannot be visualized with the OP laryngoscope, the SJ is used to displace the base of tongue and provide a pathway for placement of an ETT “blindly.” A stylet must be used, with an exaggerated curve at the distal end of the ETT. This curve allows the tip of the ETT to extend further anteriorly, beyond the exposure provided by the laryngoscope, and into the glottic inlet. The ETT is advanced into the oral cavity lateral to the laryngoscope (entering at the oral commissure) and is guided toward the midline of the airway (from right to left) (Fig. 9.12). It should
Fig. 9.10 As the laryngoscope is removed, the intraoral portion of the ETT is manually secured
Fig. 9.11 The cup forceps are released as the entire laryngoscope is removed
Fig. 9.12 Intubation using a Sliding Jackson laryngoscope. Note the acute bend at the distal end of the tube

58 |
Airway Management for Larygeal Surgery |
be emphasized that this type of “blind” intubation is not a preferred method of securing the airway. Instead, is a “court of last resort” for peroral intubation when all other options have failed. Also, it should be noted that substantial experience with intubation/difficult laryngeal exposure is required before attempting this technique.
9.6Anesthesia
for Laryngeal Framework Surgery
Monitored anesthesia care for patients undergoing framework surgery is often suboptimal due to a lack of communication between the surgeon and the anesthesiologist. To most anesthesiologists, “monitored anesthesia care” for a patient undergoing a local procedure involves sedation via a propofol (Diprivan)
9 drip. Propofol is felt to be superior to midazolam (Versed), due to its ease of rapid titration, faster wake-up times, and better quality of sedation. However, propofol is poorly suited for framework surgery performed under local anesthesia for the following reasons:
■There is tendency for an “all-or-none” phenomenon; the patients is either deeply sedated (often snoring), or completely awake/alert and uncomfortable.
■Due to the rapid nature of “emergence” from the sedated state, the patient often becomes disinhibited/combative when “awakened” and asked to phonate. This is likely exacerbated by the presence of a noxious stimulus (indwelling flexible transnasal laryngoscope).
Midazolam (Versed) is much better suited for sedation in framework surgery patients, and results in a more relaxed, aware, and cooperative patient.
In terms of local anesthesia, 1% lidocaine with epinephrine is infiltrated into the subcutaneous and deep tissues from the hyoid to the upper cricoid cartilage on the side of the proposed surgery, as well as 1 cm past the midline. The anesthetic solution should be infiltrated down to the depth of the thyroid cartilage. In general, 15–20 ml of solution is required. Additional supplemental injections are usually required during the surgical dissection, as needed. One must be careful to avoid injection into the paraglottic space and/or thyroarytenoid muscle, which could result in an inadvertent “injection augmentation.” In most cases, successful medialization and layered closure of the skin can be achieved without the need for further anesthesia at the incisional site.
Key Points
■A preoperative management plan for securing the patient’s airway must be discussed with the anesthesiologist prior to proceeding with surgery. All necessary equipment should be opened and readily available in the operating room before proceeding.
■In general, lesions located on the anterior two thirds of the larynx (membranous vocal folds) can be adequately exposed/treated with a 5.5 or smaller ETT. Lesions of the posterior third of the
larynx (vocal processes and posterior commissure/ arytenoid region) require jet ventilation, displacement of the ETT anteriorly, or apneic technique.
■Mask induction with inhalational agents, followed by jet ventilation is the preferred method of airway management for endoscopic treatment of subglottic/tracheal stenosis. Endotracheal intubation should be avoided in these cases.
■Jet ventilation is safest when used proximal to the stenotic region; ventilation distal to the stenosis carries an increased risk of air trapping and pneumothorax.
■If tracheostomy is performed in a patient with subglottic/tracheal stenosis due to intraluminal scar formation, then the airway should be entered at least 1 cm inferior to the area of the stenosis. Tracheostomy entry through the area of narrowing is ideal (though not essential) if cartilaginous collapse is present, however.
■The following conditions may predict a “difficult exposure” perorally:
■Retrognathia
■Lingual hypertrophy/poor palatal visualization
■Trismus/reduced interincisor opening
■Short, thick neck
■Limited neck flexion
■Alternative methods of obtaining an airway in a “difficult exposure” case include:
■Tracheostomy under local
■Awake, fiberoptic nasotracheal intubation
■Laryngoscopy and intubation using a specialized “anterior” laryngoscope
■Ossoff–Pilling laryngoscope
■Laryngoscopy and intubation without visualization of vocal folds
■Sliding Jackson laryngoscope plus curved ETT with stylet
■LMA
■Topical 4% lidocaine (laryngotracheal anesthesia, commonly referred to as “LTA”) should be applied to the laryngotracheal region prior to instrumentation of the larynx. In addition, at the end of the surgical case, another application may be repeated (if greater than 45–60 min after the initial lidocaine treatment). Lidocaine reduces the incidence of laryngospasm.
Selected Bibliography
1Hunsaker DH (1994) Anesthesia for microlaryngeal surgery: the case for subglottic jet ventilation. Laryngoscope 104(Suppl.):1–30

|
Chapter 9 |
59 |
2 |
Sofferman RA, Johnson DL, Spencer RF (1997) Lost airway dur- |
3 |
Hochman II. Zeitels SM. Heaton JT (1999) Analysis of the forces |
|
ing anesthesia induction: alternatives for management. Laryngo- |
|
and position required for direct laryngoscopic exposure of the |
|
scope 107:1476–1481 |
|
anterior vocal folds. Ann Otol Rhinol Laryngol 108:715–724 |

Part B Phonomicrosurgery
for Benign Laryngeal
Pathology
IFundamentals
of Phonomicrosurgery

Chapter 10
Principles of Phonomicrosurgery |
10 |
|
10.1Fundamental and Related Chapters
Please see Chaps. 1, 4, 8, 11, 12, 15, 16, 17, 18, 22, and 23 for further information.
10.2Introduction
Phonomicrosurgery encompasses a variety of operations that has the primary goal of improving voice quality. These are elective operations that involve precision microsurgical removal of benign vocal fold pathology—most often from the subepithelial space of the vocal fold. The surgical procedures and principals are based on vocal fold physiology, specifically Hirano’s coverbody theory of vocal fold vibration (see Chap. 1, “Anatomy and Physiology of the Larynx”). Given the importance of the interaction between the epithelium–superficial layer of the lamina propria (cover) and the underlying deep layer of the lamina propria and muscle (body), phonomicrosurgery was born and has evolved to advocate the minimal disruption to the normal microarchitecture of the vocal fold while removing dysphoniainducing pathology. The overarching goal is to limit dissection to the most superficial plane possible and maximize epithelial and lamina propria preservation. The latter tenet is important to facilitate primary wound healing versus secondary wound healing. This is theorized to allow maximal functional recovery (vocal fold mucosal vibration) after surgery.
10.3Surgical Indications and Contraindications
Phonomicrosurgery is an elective surgery, and thus, pressure should not be placed on the patient to proceed with surgery. The risks and benefits of the surgery should be detailed to the patient and most importantly, a realistic and thorough evaluation of the patient’s functional voice limitations and abilities (speech and singing) should be reviewed. Often this review process should be done over several weeks and involve the patient, physician, family members, a speech–language pathologist and possibly a singing voice specialist. When all nonsurgical treatment modalities have been exhausted and significant vocal functional limitations exist, the setting is appropriate for proceeding with phonomicrosurgery (see Chap. 8, “Timing, Planning, and Decision Making in Phonosurgery”).
Important preoperative measures before phonomicrosurgery include:
■Avoiding aspirin, nonsteroidal anti-inflammatory medications or other anticoagulation medications
■Avoiding significant vocal abuse and misuse immediately before surgery
■Avoiding operating during the premenstrual period of a woman’s menstrual cycle, due to the slight edema occurring at this time as well as some increased fragility of the microvasculature of the vocal fold
Preoperative voice therapy (one to two sessions) is extremely important in preparation for phonomicrosurgery for a variety of reasons:
■Psychological preparation for surgery
■Education regarding postoperative voice rest and voice use
■Modification and improvement of improper speaking techniques and habits
■Laying the foundation for postoperative voice therapy, both psychologically as well as from a behavioral perspective
Preoperative voice therapy stresses to the patient the importance of changing inappropriate vocal techniques and implementing healthy voice behaviors in the postoperative period.
Prior to phonomicrosurgery, the patient must realize he/she will be on voice rest and reduced voice use for a variable period (from 3 to 30 days). This is to ensure that the patient has adjusted his/her voice use to be compliant with the surgeon’s voice rest and reduced voice use limitations.
Preoperative consent for phonomicrosurgery should involve the risks of general anesthesia, temporal mandibular joint injury, dental injury, and injury to the lingual nerve. The latter has been shown to be temporary in nature and lasts on average 2 weeks, with a maximum duration of 1 month. A discussion regarding postoperative voice quality after phonomicrosurgery should be taken seriously and done by the surgeon. Discussion should involve the small but real risk of either no improvement of the voice quality (~1–2% incidence) or a reduction in vocal function or voice quality (~1–2% incidence).
The surgeon should review the patient’s most recent stroboscopy (last exam should be within previous 15–20 days) prior to phonomicrosurgery. Preferably, this review is done the day of surgery or 1–2 days before the surgery. The optimal situation for this preoperative stroboscopy review is to have the stroboscopy examination available for review in the operat-

64 Principles of Phonomicrosurgery
ing room immediately before as well as during the procedure. This allows the surgeon to correlate stroboscopic findings with surgical findings and make important decisions on location of pathology, location of placement of incisions, and the degree
Table 10.1 Standard microlaryngeal instrumentation
|
High-quality operating microscope with 400-mm lens |
|
|
Large-bore laryngoscope (largest diameter possible) |
|
|
Examples include: |
|
|
• Universal modular glottalscope (Endocraft) |
|
|
• Sataloff laryngoscope (Medtronic ENT) |
|
|
• Lindholm (Karl Storz) |
|
|
• Operating laryngoscope for anterior commissure (model #8458.011, Richard Wolf ) |
|
|
Specialized laryngoscopes for unique situations |
|
|
• Ossoff–Pilling for difficult exposure (Pilling) |
|
|
• Posterior-commissure laryngoscope (Pilling) |
|
|
Suspension system |
|
|
• Boston University suspension (Pilling or Endocraft) (Figs. 10.16, 10.20) |
|
10 |
||
• Fulcrum suspension: Lewy suspension and table-mounted Mayo stand (Pilling) (Fig. 10.17) |
||
|
|
Operating chair with arm supports (Fig. 10.22)
Instrumentation (Karl-Storz, Medtronic ENT, Instrumentarium)
•Specialized blunt microelevators (Fig. 10.1)
•Microcup forceps (1–2 mm in diameter) (Fig. 10.2)
•Up-angled, right and left micro-ovoid cup forceps (Fig. 10.3)
•Microscissors (Fig. 10.4)
•Curved (left and right)
•Up angled
•Curved alligator forceps (left and right) (Fig. 10.5)
•Straight alligator forceps
•Microlaryngeal suctions (3, 5, and 7 French)
•Triangular (Bouchayer) forceps (left and right) (Fig. 10.6)
•Microlaryngeal knife (sickle or spear)
Miscellaneous equipment
•Cotton surgical pledgets (0.5 × 2 cm)
•1:10,000 epinephrine
•Velcro strap or cloth/silk tape
•Mouth guard (maxillary, ± mandibular)
•Acrylic—custom made by dentist
•Molded “athletic” tooth protector
•Plastic “anesthesiologist” tooth guard, reinforced with layers of cloth tape (Fig. 10.18)
•Foam from operating room headrest or “doughnut” (edentulous patients only) (Fig. 10.9)
Optical telescope
•Diameter: 4–5 mm, length: 20 cm or more
•0, 30, and 70°
Microdebrider—skimmer blade (Medtronic ENT)
Subepithelial infusion needle (25 or 27 g)
•Zeitels needle (Endocraft)
•Orotracheal injector (Medtronic ENT)
Small-diameter, extended-length endotracheal tube (5.0 or 5.5) designed for microlaryngoscopy (Mallinckrodt)
Tracheal jet ventilation tube (Hunsaker jet ventilation tube; Medtronic ENT)
The listed equipment/vendors are those the authors have utilized. This is by no means a complete list of all the vendors who make these products: Endocraft (Providence, R.I.), Karl Storz (Culver City, Calif.), Instrumentarium (Montreal, Quebec, Canada), Mallinckodt (Hazelwood, Mo.), Medtronic ENT (Jacksonville, Fla.), Pilling (Research Triangle, N.C.), Richard Wolf (Vernon Hills, Ill.)

of dissection and excision using the preoperative stroboscopy and the operative findings as guides.
10.4Equipment for Phonomicrosurgery
Specialized laryngoscopes are required for phonomicrosurgery. The larger the laryngoscope, the better for phonomicrosurgery, given that this results in significantly improved exposure and access to the surgical site(s). Multiple large and specialized laryngoscopes exist and a wide variety of laryngoscopes are necessary to manage all different types of phonomicrosurgical lesions and procedures. Specialized laryngoscopes for individualized laryngoscopy needs are important, e. g., posterior commissure laryngoscope for difficult posterior glottic exposure, and the Ossoff-Pilling laryngoscope for microlaryngeal surgery on patients with restricted upper aerodigestive tract anatomy (Table 10.1).
The core set of instruments utilized for phonomicrosurgery includes specialized blunt microelevators, cup forceps, scissors, curved alligators, and small suctions (3, 5, and 7 French). These elevators are often used to palpate submucosal pathology at the start of surgery. In addition, a specialized set of instruments has been developed for microflap retraction. These are called triangular forceps or Bouchayer forceps. Most of the instruments described below are available from several manufacturers of phonomicrosurgery equipment, including Medtronic ENT (Jacksonville, Fla.), Karl Storz (Culver City, Calif.) and Instrumentarium (Montreal, Quebec, Canada).
Key microlaryngoscopy instruments utilized for phonomicrosurgery involve:
■Specialized blunt microelevators (Fig. 10.1)
■The microelevators should be blunt and have several different angles and sized to allow the surgeon to work in various angles in different positions within the vocal fold, specifically, dissecting the vocal fold lesion off the overlying microflap.
Chapter 10 |
65 |
■Microcup forceps (Fig. 10.2)
■Several small special cup forceps have been developed over the last 5–10 years to facilitate several specific situations that are encountered in phonomicrosurgery. These forceps have a sharp cutting edge but a very limited cutting surface, only the most distal 180º of the forceps cut. The most useful micro cup forceps is angled-up and has a 1-mm diameter.
■Micro-ovoid cup forceps (Fig. 10.3)
■Ovoid-shaped microcup forceps are also essential for removing small pieces of pathologic mucosa and papilloma (see Chaps. 15, “Vocal Fold Polyp” and 21, “Recurrent Respiratory Papillomatosis of the Larynx”). This instrument comes in two sizes and is valuable for precision removal of small amounts of tissue.
Fig. 10.2 Microcup forceps (1 mm) cutting surface limited to distal 180°
Fig. 10.1 Angled elevators for phonomicrosurgery |
Fig. 10.3 Micro-ovoid cup forceps |

66 |
Principles of Phonomicrosurgery |
■Microscissors (Fig. 10.4)
■The most commonly used microscissors are right and left curved as well as “straight up,” or angled scissors. These scissors should be maintained at all times to appropriate surgical precision and sharpness, given that they are the primary cutting tool for phonomicrosurgery.
■Curved alligators (Fig. 10.5)
■Epinephrine (1:10,000) and cotton pledget (0.5 × 2 cm)
■Microlaryngeal suctions (3, 5, and 7 French)
■Triangular forceps or Bouchayer forceps (for microflap retraction) (Fig. 10.6)
■These instruments are designed to retract the microflap to allow vocal fold visualization and dissection while minimizing trauma to the microflap. They are made in a variety of sizes and designs for different situations.
10
Fig. 10.4 Microscissors, curved and angled up
■Sickle knife (or spear-shaped knife)
■These knives tend to become dull very quickly, and thus it is recommended that this knife be replaced with every case or at least on a very frequent basis. A dull knife can result in tearing of the mucosa and can significantly limit the efficacy of phonomicrosurgery
■Microdebrider
■The microdebrider is a powered instrument that provides simultaneous suction and cutting activity used for rapid removal of exophytic lesions in the larynx such as recurrent respiratory papillomatosis (RRP) (see Chap. 21, “Recurrent Respiratory Papillomatosis of the Larynx”). There are two different types of cutting blades:
■Conservative (i. e., “skimmer blade”)
■Aggressive
■The conservative blade is the most commonly used for laryngeal surgery. The advantages of the microdebrider are expedient removal of a significant amount of laryngeal pathology; less
pain after surgery (compared with the CO2 laser); less expensive than the laser; and potentially even safer, given the risks of laser laryngeal surgery.
The disadvantages of microdebrider for laryngeal surgery include the powered instrument shaft
is relatively large, and sometimes visualization can be limited, and the risk that the powered instrument may be too strong and injure delicate subepithelial tissues of the vocal fold or other endolaryngeal structures.
Suspension of the laryngoscope is a fundamental aspect of phonomicrosurgery. Two basic designs for placing the laryngoscope into a fixed and stable position exist. These are categorized as a gallows suspension device, and a rotation, or fulcrum device. The gallows suspension laryngoscope is favorable, given that there is more appropriate upward vector of the laryngoscope, which can provide optimal exposure of the en-
Fig. 10.5 Curved alligators for phonomicrosurgery |
Fig. 10.6 Triangular (Bouchayer) forceps |

|
Chapter 10 |
67 |
dolarynx with minimal risk of dental injury, especially to the maxillary teeth. This device is not the most common due to traditional and historical use of rotation-fulcrum devices (i. e., Lewy suspension).
Long Hopkins rod telescopes with various visualization angulations are an essential component to phonomicrosurgery. Rarely is the surgery performed utilizing these telescopes, but these telescopes are used to provide the surgeon a “three-di- mensional visualization” of the vocal folds and their related pathology. The 30 and 70° telescopes, which are approximately 4–5 mm in diameter and 30 cm long, should be utilized immediately prior to phonomicrosurgical incision and are often used during phonomicrosurgery as well as at the end of the surgery to ensure that all appropriate pathology has been removed. These angled telescopes are readily available in most operating rooms, given they are used regularly for cystoscopy. Telescopes used for sinus surgery are too short to be effectively used for laryngeal imaging.
The microscope used for phonomicrosurgery should be of the highest quality and provide the surgeon with a stable visualization method of the endolarynx. There should be significant adjustment as well as control over many different articulated angles of the microscope. This microscope should be the same microscope that is used for precision otologic procedures such as stapes surgery and other middle ear operations. The microscope that is routinely used for the placement of pressure equalizing tubes is typically not appropriate for phonomicrosurgery. Furthermore, the microscope should have the capability of being compatible with the CO2 laser micromanipulator attachment. Typical length of the lens used on the surgical microscope for phonomicrosurgery is 400 mm. This allows adequate space between the proximal end of the laryngoscope and the microscope for hand instruments to be used for phonomicrosurgery.
Another important feature of the surgical microscope is articulated eyepieces; this allows for optimal surgeon ergonomics, which is important for lengthy phonomicrosurgery cases as well as for the long-term health of the phonomicrosurgeon.
Lasers have a limited role in phonomicrosurgery surgical procedures (see Chap. 13, “Principles of Laser Microlaryngoscopy”). The most commonly used laser is the CO2 laser, which can be used for cautery of vascular ectatic lesions. The CO2 laser with the micromanipulator has also been used for making vocal fold incisions or removing free-edge lesions. However, there are no distinct advantages of the use of this laser in this setting, and the risks of thermal injury and costs of the instrument outweigh any potential benefits. The majority of phonomicrosurgery can and should be done with “cold-steel” instrumentation. Recently, the pulsed-dye (PDL) and pulsed-KTP lasers have been advocated for phonomicrosurgery. However, benefits over cold-steel surgery have not yet been demonstrated, but they may be complementary when dealing with vascular lesions associated with other vocal fold lesions (cyst, polyp, etc.). The CO2 laser does offer an “instrument-free” approach to surgery of the vocal folds, and in a very small, crowded surgical space, this can be an advantage. However, for most phonomicrosurgical situations this is not a major problem, and thus the CO2 laser is rarely indicated for this reason alone.
10.5Phonomicrosurgery Procedures, Techniques, and Methods
10.5.1 Anesthesia
A working relationship based on mutual respect, communication, and teamwork with your anesthesia colleague(s) is essential for successful phonomicrosurgery (see Chap. 9, “Anesthesia and Airway Management for Laryngeal Surgery”). Phonomicrosurgery involves general anesthesia, and complete muscle relaxation should be implemented after the induction of general one and continuously monitored throughout the surgery. Preoperatively, one should administer i.v. steroids and Robinol™ (unless contraindicated). Placement of the endotracheal tube is extremely important, given that a misplaced or traumatic placement of the endotracheal tube can cause injury to the vocal folds and may result in cancellation of surgery and/ or injury to the vocal folds. The placement of the endotracheal tube should be under complete controlled conditions, and no stylet should be used for the placement of the endotracheal tube. Furthermore, the otolaryngologist should be present during the intubation to monitor the situation and be available to assist with intubation when the situation is required. Similarly, controlled extubation at the end of phonomicrosurgery is another important aspect of the necessary teamwork between the anesthesia team and the phonomicrosurgeon. Extubation should be done in a controlled fashion, and all measures should be used to reduce the likelihood of the patient coughing after extubation.
The ventilation options for phonomicrosurgery are endotracheal intubation, jet ventilation, or apneic methods. The large majority of phonomicrosurgery is best performed using endotracheal intubation with a small (5.0 or 5.5), specialized endotracheal tube. This provides a still operating field and complete control of the airway. Sometimes the endotracheal tube can be in the way for the surgical procedure and may need to be repositioned or removed in its entirety. Jet ventilation for phonomicrosurgery should be done only on an as-needed basis and is best done when the jet ventilation is delivered from a small jet ventilation catheter placed in the mid-tracheal region. (see Chap. 9, Fig. 9.1; Hunsaker tube, Medtronic ENT) Tracheal jet ventilation is preferred compared with supraglottic jet ventilation, given that the former provides the surgeon with less vibration and desiccation of the vocal fold tissues while phonomicrosurgery is being performed, and allows end-tidal CO2 monitoring.
Appropriate and successful phonomicrosurgery can rarely be performed using an apneic technique for anesthesia, given that the time between ventilations is too short for most phonosurgical procedures. An exception to this may be for bronchoscopy (flexible or rigid) and diagnostic laryngoscopy prior to the placement of an endotracheal tube.
